Jang, Hwang, Jin, Shin, and Cho: Factors Affecting Cage Obliquity and the Relationship between Cage Obliquity and Radiological Outcomes in Oblique Lateral Interbody Fusion at the L4-L5 Level
Abstract
Objective
This retrospective study investigated the factors that affect cage obliquity angle despite orthogonal maneuvers performed during oblique lateral interbody fusion (OLIF) and assessed the relationship between cage obliquity angle and radiological outcomes post-surgery.
Methods
Twenty-nine males who underwent L4-L5 OLIF for lumbar degenerative disease between 2019 and 2021 with a follow-up duration greater than 12 months were analyzed. Radiological parameters were measured including psoas muscle volume, total psoas area index (total psoas muscle area [cm2]/height squared [m2]), distance from the iliac artery to the origin of the psoas muscle (DIAPM), angle between the origin of the psoas muscle and the center of the vertebral disc (APCVD), iliac crest height, disc height, lumbar flexibility (lumbar flexion angle minus extension angle), cage location ratio, cage-induced segmental lumbar lordosis (LL) (postoperative index level segmental LL minus used cage angle), foraminal height changes, fusion grade.
Results
DIAPM, APCVD, iliac crest height, postoperative index level segmental LL, and cage-induced segmental LL were significantly correlated with OLIF cage obliquity angle. However, other radiological parameters did not correlate with cage obliquity. Based on multiple regression analysis, the predictive equation for the OLIF cage obliquity angle was 13.062-0.318×DIAPM+0.325×A PCVD+0.174×iliac crest height. The greater the cage obliquity, the smaller the segmental LL compared to the cage angle used.
Conclusion
At the L4-L5 level, OLIF cage obliquity was affected by DIAPM, APCVD, and iliac crest height, and as the cage obliquity angle increases, LL agnle achievable by the used cage could not be obtained.
Key Words: Spinal fusion · Lumbosacral region · Iliac artery · Psoas muscles · Spine.
INTRODUCTION
Oblique lateral interbody fusion (OLIF) was first described by Michael Mayer in 1997 [ 15, 16] and involves minimally invasive spine access to the disc space via a corridor between the peritoneum and psoas muscle [ 4]. Compared to direct lateral interbody fusion (DLIF), OLIF has fewer complications related to lumbar sympathetic plexus injuries, such as anterior thigh pain, paresthesia over the thigh and groin region, and hip flexor weakness [ 19]. Unlike DLIF, which confirms true lateral configuration and the cage is inserted straight, during OLIF, the cage is often observed in the disc space in an oblique form. Some studies report that it is common to see cases of cage obliquity on postoperative computed tomography (CT) or magnetic resonance imaging (MRI) with cage insertion after OLIF [ 3, 11], In addition, in one study, the average cage obliquity was 13.0°±5.9°, and a representative moderate case was reported to be 19.1°±5.2° [ 3]. In particular, it was reported that the cage obliquity is greater at the L4-L5 level than at other levels [ 20]. As such, incorrect placement of the lateral cage resulted in : 1) impingement of the retroperitoneal vessels or nerves; 2) spillage of high concentrations of bone morphogenic protein, which is often placed into the cage to enhance fusion; 3) coronal malalignment of the segment; and 4) increased gap between the cage and vertebral endplate, which can also result in problems such as pseudoarthrosis [ 3, 21]. Therefore, to account for instrumentation shifting, an orthogonal maneuver is required to change the cage from an oblique trajectory to a direct lateral trajectory [ 6]. The purpose of this study was to investigate the factors that affect cage obliquity angle despite orthogonal maneuvers and determine the relationship between cage insertion angle and radiological outcomes occurring after surgery.
MATERIALS AND METHODS
After approval from the Institutional Review Board of Armed Force Capital Hospital (No. AFCH 2022-10-004-001) was obtained, we retrospectively reviewed the medical records of patients. Informed consent was waived. We retrospectively reviewed the medical records of patients who underwent OLIF at L4-L5 from January 2019 to December 2021.
Patient enrollment
We performed a retrospective data survey of 59 patients who underwent OLIF for degenerative stenosis with or without spondylolisthesis. To minimize the influence of biomechanical differences in the lumbar vertebral site, we only included patients who underwent surgery at L4-L5. Patients with facetectomy due to cage malposition, cage anterior migration during the follow-up period, prior transforaminal lumbar interbody fusion (TLIF) to OLIF revision, and OLIF with posterior decompression, were excluded.
The indications for OLIF were as follows : 1) central stenosis with instability; 2) degenerative spondylolisthesis; 3) degenerative scoliosis; and 4) neural foraminal stenosis, confirmed by spine radiographs, CT, and MRI.
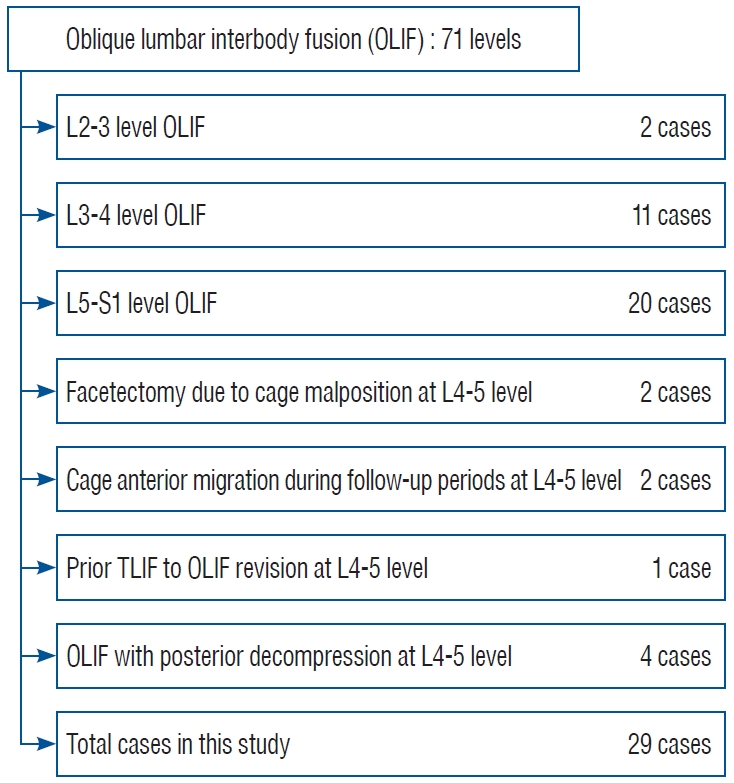
Ultimately, we enrolled 29 patients who underwent OLIF at L4-L5 ( Fig. 1). These patients underwent whole spine radiographs, dynamic radiographs, lumbar spine CT, and MRI preoperatively, and at 6 months and 12 months postoperatively.
Surgical procedure and postoperative management
All operations were performed by one neurosurgeon (S.H.H.). The patients were positioned in the right local decubitus position, and then positioned using a bean bag after general anesthesia. After draping, the surgical site was confirmed with a C-arm, and an oblique skin incision of two fingers was performed in the front of the abdomen in the vertebral anterior body line. External, internal, and transverse abdominis muscles were sequentially split, and then retroperitoneal fat was observed downwards. The psoas muscle was palpated with a finger and bluntly dissected. The peritoneum was pushed forward, and by exposing the psoas muscle, the iliac blood vessels and the origin of the psoas muscle were confirmed, and blunt dissection at the origin of the psoas muscle was performed. The tubular retractor was inserted under C-arm guidance. The tubular retractor was fixed to the L4 ventral body with a fixing pin and opened to check the disc space. Annulotomy was performed based on the origin of the psoas muscle. Moreover, annulotomy was mostly conducted at the anterior third of the disc space. The intervertebral disc was removed using a shaver, endplate preparation was performed, and then cage insertion was performed. At this time, the cage was properly inserted using the orthogonal maneuver which was performed by inserting the cage at an angle first and entering the anterior one-third of the way, and then the assistant pushed the patient’s back forward and at the same time erected the cage vertically. The trapezoid-shaped polyether ether ketone cage (Clydesdale; Medtronic, Minneapolis, MN, USA) was filled with the demineralized bone matrix (Accell Connexus®; Seaspine, Carlsbad, CA, USA), allobone chip (Maxxeus, Kettering, OH, USA), and bone morphogenetic proteins (Novosis; CGBio, Seoul, Korea). After changing the patient to the prone position, using the spine table to create sufficient lumbar lordosis (LL), and confirming with the C-arm, posterior fixation was performed using the percutaneous pedicle screw system (Longitude system; Medtronic).
All patients were encouraged to ambulate from the day of surgery and were discharged 14 days after surgery. The patients were instructed to wear a lumbar-sacral orthosis for 6 months for instrumented fusion.
Clinical evaluation
To investigate changes in clinical outcomes before and after surgery, we used the immediate preoperative and 12-month postoperative visual analog scale (VAS) scores and Oswestry Disability Index (ODI) values.
Radiologic evaluation
All patients were evaluated using whole spine radiographs, preoperative static and dynamic lumbar radiographs, CT, and MRI. For follow-up, whole spine radiographs, static and dynamic lumbar radiographs, and CT were obtained 6 and 12 months postoperatively.
On whole spine radiographs, pelvic incidence, sagittal vertical axis (SVA), lumbar coronal and sagittal Cobb angles were measured preoperatively and at 6 months and 12 months postoperatively. The segmental lumbar lordotic angle (SLA), segmental lumbar coronal Cobb angle (SCA), disc anterior height (DAH), and iliac crest height were examined with standing neutral lateral radiograph imaging at L4-L5. The iliac crest height was marked with + if it invaded the disc space, and the distance between the L5 upper endplate and the furthest point where the vertical line meets the iliac crest was marked. On the other hand, cases where the iliac crest was lower than the L4-L5 disc space was marked as -, and the distance between the L5 upper endplate and the portion where the line drawn perpendicular to the iliac crest first met was measured. If the left and right heights were different in the image, and the surgical site was the left, the left pelvic height was measured in the lateral X-ray view with reference to the standing AP X-ray. The highest point of the iliac crest was chosen as the measurement site because the surgery was performed in a lateral position without bending, and the highest point was deemed to be highly reproducible during OLIF surgery at the L4-L5 level. The sagittal range of motion (lumbar flexibility) was measured using standing lateral extension and flexion radiograph imaging at L4-L5. Lumbar flexibility was calculated as the difference between the LL angle during flexion and extension in lumbar spine dynamic radiographs. Moreover, cage location ratio was measured by comparing the center of the cage and the upper endplate of the caudal vertebral body [ 21] ( Fig. 2). Cage obliquity angle, foraminal height (FH), fusion grade, and subsidence rate were measured using CT images. The cage obliquity angle was measured based on a line perpendicular to the line from the spinous process to the center of the intervertebral disc and a line formed by the cage metallic marker. FH was measured in sagittal view from the pedicle interior margin of the gastric vertebral body to the upper margin of the pedicle of the lower vertebral body, and the fusion grade was measured using the Bridwell fusion grade [ 2] ( Supplementary Table 1). On MRI, the area of the psoas major muscle of the corresponding surgical level, the total psoas muscle area index (TPAI), the distance from the iliac artery to the origin of the psoas muscle (DIAPM), and the angle between the origin of the psoas muscle and the center of the vertebral disc (APCVD) were measured. The psoas muscle area was measured using the axial cross-section of the left psoas major muscle approached during surgery on MRI at T2, and the TPAI was measured using the left and right psoas major muscle area of L3-L4 divided by the height [ 8, 17]. The DIAPM was measured as the straight distance from the iliac artery to the point where the psoas muscle was attached to the vertebral disc [ 22]. The APCVD was measured as the angle between the transverse line of the intervertebral disc to the point where the psoas muscle was attached to the vertebral disc ( Fig. 2).
Statistical analysis
Linear regression analysis was performed with several independent variables to determine if the measured data were related to cage obliquity. In addition, independent variables thought to affect cage obliquity were analyzed using a multiple linear regression model, and a p-value <0.05 was considered statistically significant. Estimated regression expression statistics of the cage obliquity angle were calculated with significant values from the multiple linear regression analysis.
In addition, demographic data and pre- and postoperative radiographic parameters in the two groups (a group with an obliquity angle greater than 15° and a group with an obliquity angle less than 15°) were compared. Data obtained via the radiological analysis were analyzed for statistical significance using the Student t-test. Descriptive variables were analyzed with the chi-square test or Fisher exact test. The results are presented as mean±standard deviation. Variables with p<0.1 in the univariate analysis were used in the multivariate analysis. Moreover, we used receiver-operating characteristic (ROC) curves to assess the predictability cutoff values.
Statistical analysis was performed using IBM SPSS statistics for Windows version 21.0 (IBM Corp., Armonk, NY, USA).
Interclass and intraclass correlations
All measurements were performed twice at intervals of >2 weeks by one neurosurgeon (C.W.J.), and twice by another neurosurgeon (S.H.H.). The intraobserver and interobserver intraclass correlation coefficients were calculated for mean values.
RESULTS
The cage obliquity angle in patients who underwent OLIF surgery at L4-L5 during March 2019 to December 2021 was 15.1°±5.7° (range, 5.8°-27.5°). All patients included in the study were male and the mean age was 44.8±8.9 years (range, 19-58). The average body mass index (BMI) of the patients was 26.9±3.4 (range, 21.1-33.2), the psoas muscle volume encountered at surgical approach was 20.8±3.5 (range, 13.0-26.5), and the TPAI, an approximate indicator of skeletal muscle mass, was 10.2±1.8 (range, 7.6-13.5). The DIAPM was 14.8±5.2 mm (range, 4.9-25.3) and the APCVD was 22.7°±7.3° (range, 9.3°-43.4°). In standing neutral lateral radiograph imaging at L4-L5, the iliac crest height was -1.3±9.4 mm (range, -12.5 to 15.7), and in standing dynamic radiograph imaging, L4-L5 flexibility (flexion-extension angle) was 13.4°±6.6° (range, 1.8°-28.6°). The cage angles used were 6º and 12º, and the cage heights used were 10, 12, 14, and 16 mm ( Table 1).
Radiological measurements
The cage obliquity angle measured at 12 months postoperatively was 15.1±5.7 (range, 5.8-27.5). The SLA, SCA, DAH, and FH changes were increased by 1.8°±4.2°, -0.47°±1.8°, 4.2±2.7 mm, and 5.4±3.3 mm on average, respectively. The changing pattern of SLA compared to the cage angle used (postoperative index level SLA - used cage angle) and the changing pattern of disc height compared to the cage height used (postoperative index level DAH - used cage height) were -0.4°±3.5° and -0.1°±1.9°, respectively, and the average fusion grade was 1.7±0.5 ( Table 2). There was no statistically significant difference in LL (L1-S1) and SVA preoperatively versus 12 months postoperatively, and SLA did not change statistically but tended to increase. However, DAH (8.4±3.6 vs. 12.8±2.2 mm, p<0.05) and FH (17.8±2.8 vs. 23.2±3.1 mm, p<0.05) showed statistically significant increases preoperatively versus 12 months postoperatively ( Table 3).
Single and multiple regression analysis
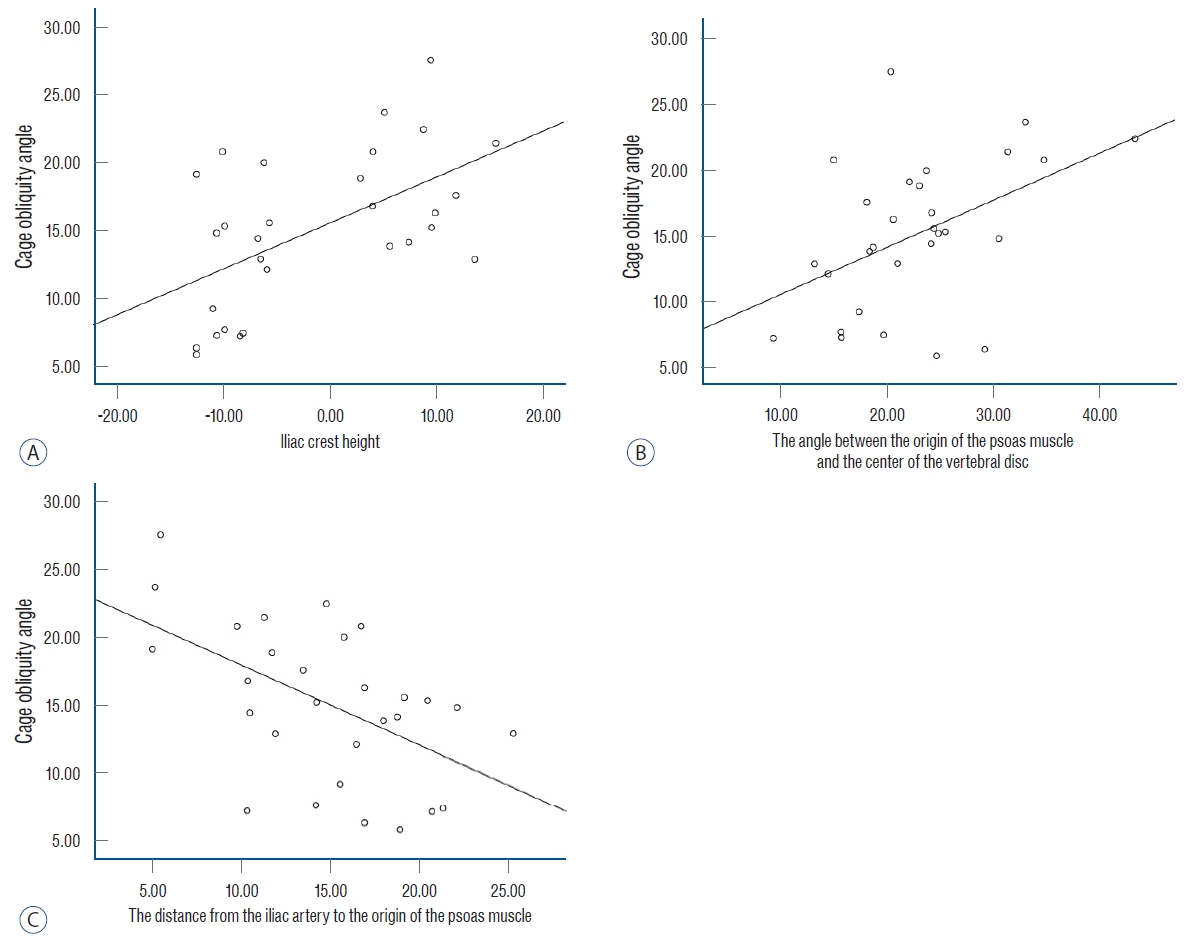
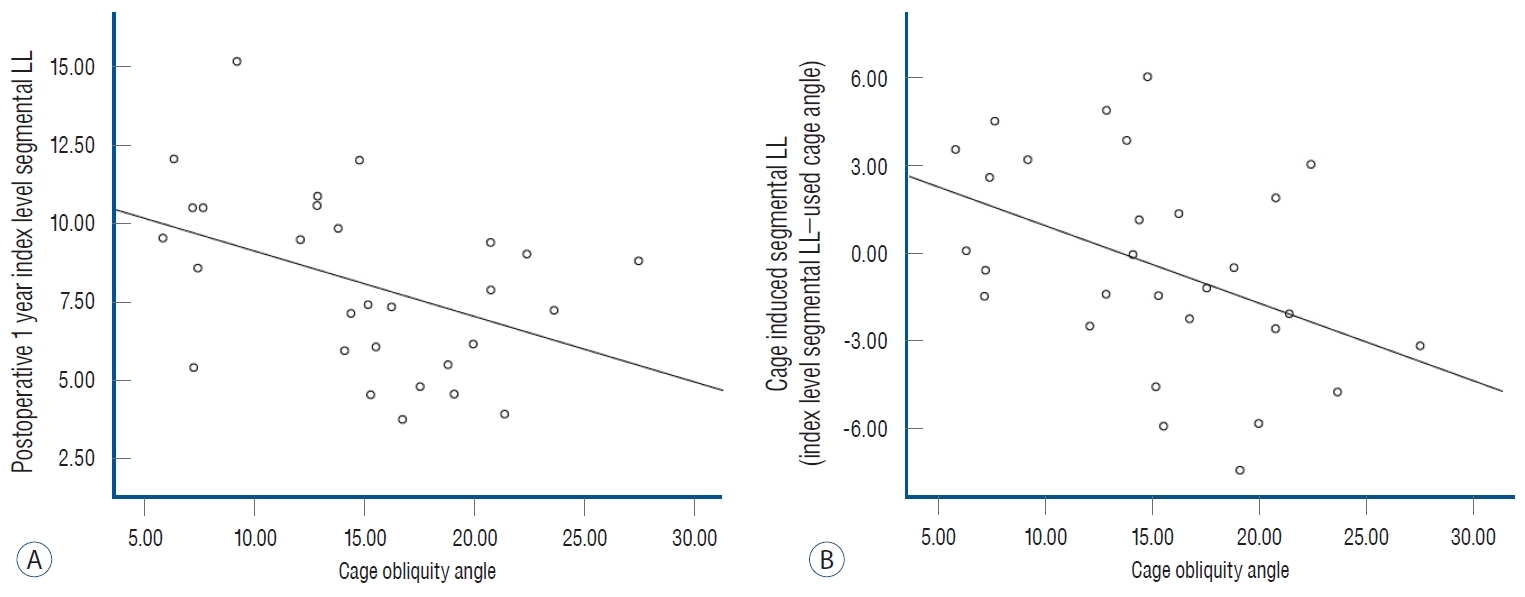
A single linear regression analysis was performed for each of the factors thought to affect cage obliquity angle, revealing that DIAPM, APCVD, and iliac crest height were three factors that were significantly correlated with cage obliquity angle (R 2=0.28 and p=0.003, R 2=0.21 and p=0.012, and R 2=0.31 and p=0.002, respectively) ( Fig. 3). Moreover, the 12 month-postoperative index level SLA and cage-induced segmental LL were significantly affected by cage obliquity angle (R 2=0.18 and p=0.02 and R 2=0.19 and p=0.02, respectively) ( Table 4 and Fig. 4). As a result of multiple linear regression analysis of factors thought to affect cage obliquity angle, these three factors were also statistically significant : DIAPM, APCVD, and iliac crest height. The variance factor (the Durbin-Watson factor) was 2.418 and the adjusted R2, indicating explanatory power, was 0.551. Based on this, the equation to predict the preoperative cage obliquity angle was calculated as : cage obliquity angle = 13.062-0.318×DIAPM+0.325×APCVD+0.174×iliac crest height ( Table 5). The correlation analysis between DIAPM, APCVD, and iliac crest height, which appear to affect cage obliquity, was not statistically significant ( Table 6).
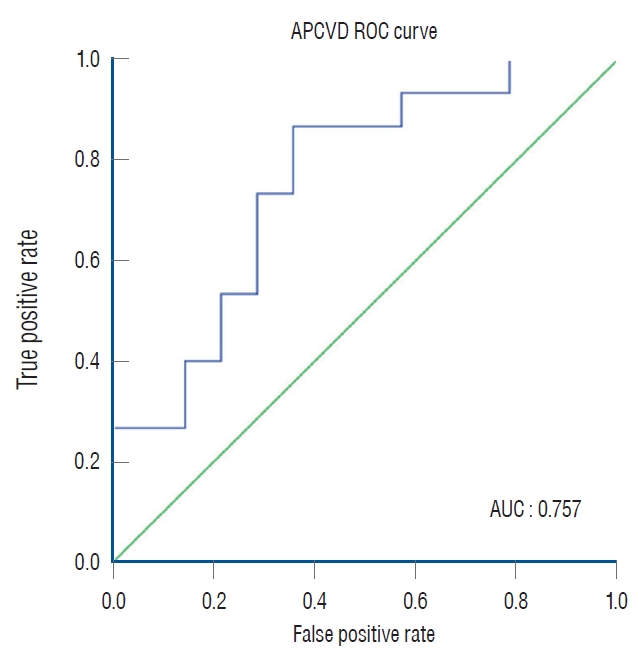
Statistical comparison by artificially dividing participants into two groups
The study divided the participants into two groups based on the mean cage obliquity angle of 15° : the small cage obliquity angle group (n=14) and the large cage obliquity angle group (n=15). The cage obliquity angle in each group was 10.4°±3.4° and 19.4°±3.5°, respectively ( p<0.05). There were statistically significant differences in preoperative DIAPM, APCVD, and iliac crest height between the two groups. Additionally, postoperative 1-year index level SLA and cage-induced segmental LL demonstrated significant differences of 9.8°±2.6° versus 6.4°±1.9° and 1.7°±2.7° versus -2.4°±3.0°, respectively ( Table 7). In univariate analysis, all three variables, DIAPM, APCVD, and iliac crest height, showed statistically significant differences. However, in multivariate analysis, only APCVD demonstrated a significant value ( Table 8). The area under the ROC curve of the APCVD was 0.757, When the cutoff value of the APCVD was calculated at 21.58°, and the sensitivity and specificity were 73.3% and 71.4%, respectively ( Fig. 5).
Clinical outcomes
At 12 months postoperatively, back and leg VAS and ODI values showed improvement ( Supplementary Table 2). However, none of these values were related to the cage obliquity angle ( Table 6).
Intra-rater and inter-rater reliabilities
For all radiological parameters, the intra-rater correlation coefficient was greater than 0.88 and the inter-rater correlation coefficient was greater than 0.82, and therefore, the mean values of the four measurements were used for the present study (e.g., intraclass correlation coefficient of the iliac crest height [ 2, 2], 0.907; 95% confidence interval, 0.827-0.949; p<0.001).
DISCUSSION
It is widely known that OLIF fusion surgery is a surgical method that can further minimize lumbar plexus injury compared to DLIF [ 1]. In OLIF, unlike DLIF, the cage is inserted diagonally into the disc space, usually based on fluoroscopic imaging of the C-arm during surgery. In this procedure, an orthogonal maneuver is performed to enable the cage to be inserted in a vertical direction similar to DLIF, without generating cage obliquity at the disc space. However, it is uncommon for the cage obliquity angle to converge to 0° with OLIF. In some studies, the reported cage obliquity angle reached 13.0°±5.9° [ 3, 19], and one more advanced study reported it as 11.3°±6.9° and that cage obliquity angle was greater at the L4- L5 level than at other levels (13.4°±6.4°) [ 20]. In this study, the average cage obliquity angle was measured at 15.1°±5.7° (range, 5.8°-27.5°) at L4-L5 level in lumbar spine CT images performed after surgery. Cage obliquity can cause several problems. Radiculopathy may be caused by a large cage and incorrect position due to cage obliquity [ 11]. In addition, concerns such as spillage of high concentrations of bone morphogenic protein, which is often placed in cages to enhance fusion, coronal malalignment of the segment, and pseudoarthrosis due to an increased gap between the cage and vertebral endplate may arise, and research on this is still lacking [ 3, 14, 21]. However, in some studies, it has been shown that cage obliquity has no effect on indicators such as postoperative bone union rate, differing degrees of foraminal decompression between right and left side neural foramen, and VAS and ODI score improvement [ 3, 9, 14]. These results are consistent with that of our study, and patient clinical outcomes and fusion grades were not correlated with cage obliquity ( Tables 4 and 6). Although there have been studies on the factors affecting cage obliquity, previous studies on the effects of orthogonal maneuvers are scarce. In this study, we considered whether factors influencing cage obliquity would be affected by the cage insertion entry point, cage insertion trajectory, and interfering factors during orthogonal maneuvers. In terms of studies on cage insertion entry points, there has been one study on surgical corridors in OLIF. According to this study, the position of the psoas major muscle and iliac artery or aorta in humans may be sufficiently different. In this study, the positions of the iliac artery and psoas muscle were categorized into six vertical zones (A, I, II, III, IV, P) and four horizontal zones (R, a, b, c, L), resulting in a total of 14 types. Our patients were classified as type Aa, Ab, Ac, Ib, and Ic, and their distribution is illustrated in Fig. 6 [ 22]. The results of this study align with the fact that the distance between the psoas major muscle where it is attached to the disc and the major blood vessel is an important factor. At this time, even though the psoas major muscle is dissected from the intervertebral disc, the orthogonal maneuver cannot be properly performed because excessive movement in a narrow space of the surgical corridor is unlikely to damage blood vessels or damage anterior longitudinal ligaments and cause cage malposition. In addition, the APCVD was taken into account considering the fact that the cage insertion trajectory enters toward the disc space midline during cage insertion before the orthogonal maneuver. This was a factor influencing cage obliquity and was significantly correlated. When divided according to a mean cage obliquity angle of 15°, APCVD stood out as the only significant risk factor, indicating that it potentially exerts the highest impact among the three factors (DIAPM, APCVD, iliac crest height) investigated in this study.
Interfering factors during orthogonal maneuvers included psoas muscle volume at the index level, TPAI reflecting approximate skeletal muscle, BMI reflecting obesity, disc height reflecting preoperative disc space collapse, and lumbar flexibility at the index level which reflects the leverage effect and that cage vertical movement can occur more easily during cage insertion [ 7, 8]. However, none of these were statistically correlated with cage obliquity. This study was limited to the L4- L5 level only, and unlike other levels of L2-L4, the iliac crest acts as an interfering factor during orthogonal maneuvers [ 10]. In several studies, surgery may be difficult due to the relationship between the location of the iliac crest and L4-L5 level, and in some cases, a surgical method for removing some of the iliac crest is also suggested [ 5, 18]. In this study, the effect on the iliac crest and the possibility of a failed orthogonal maneuver due to the iliac crest was considered. As shown in Tables 4 and 5, the cage obliquity was affected by the iliac crest. In addition, in this study, the induced cage obliquity angle was found to be a significant result among the values found to be influenced by cage obliquity. This is evaluated as the difference between the originally used cage angle and the segmental LL angle we obtained after surgery, and this value decreased as the cage obliquity increased. This means that as the cage obliquity increases, the SLA that we can obtain after surgery is small compared to the cage angle used. Similarly, other studies have shown that the SLA increases when the cage angle is horizontal rather than oblique during TLIF [ 12- 14]. This implies that as the cage approaches a horizontal position, the contact area between the vertebral body and the endplate increases in the horizontal direction, allowing the original cage angle to be achieved and promoting the creation of LL. Therefore, by dissecting slightly further from the psoas muscle origin point and placing the entry point more inward, along with a reduced trajectory angle, cage obliquity can be minimized. Additionally, considering the individual iliac crest height of each patient before surgery, surgeons can anticipate and strive to achieve the desired segmental LL angle, thus minimizing cage obliquity.
Limitations
The present study has several limitations. First, this was a retrospective study involving a small number of patients, which may have affected the strength of the results of the statistical analysis. Second, this study included only male patients who were soldiers and officers on active military duty under the age of 60 years (range, 19-58), and the design of the present study meant that there was a chance of selection bias. In the future, large-scale studies including the elderly and women are needed to overcome the limitations of this study which focused only on men. Nevertheless, the present study makes a significant contribution in that it identified factors that influence cage obliquity and factors that are affected by cage obliquity in OLIF at the L4-L5 level.
CONCLUSION
In OLIF at the L4-L5 level, cage obliquity was not correlated with the patient’s skeletal muscle mass or psoas muscle volume, but was correlated with DIAPM and APCVD, indicating a correlation with cage entry point and trajectory. Moreover, the iliac crest height was affected during orthogonal maneuvers. There was no correlation with changes in clinical outcome, fusion grade, and foramen height changes according to the degree of cage obliquity. However, the more severe the cage obliquity, the less segmental LL was produced at the index level, and less segmental LL was produced than the intended cage angle used by the surgeon. To prevent these issues, it is recommended that the three mentioned factors (DIAPM, APCVD, and iliac crest height) are considered and that orthogonal maneuvers are performed during surgery. A longterm follow-up study with a large number of patients is necessary to provide further evidence of the effectiveness of cage obliquity in OLIF.
Acknowledgements
Previous Presentations: 13th Asia Spine, A Joint Meeting with The 36th Annual Meeting of the KSNS.
Fig. 1.
Flow chart of the selection of patients. TLIF : transforaminal lumbar interbody fusion. 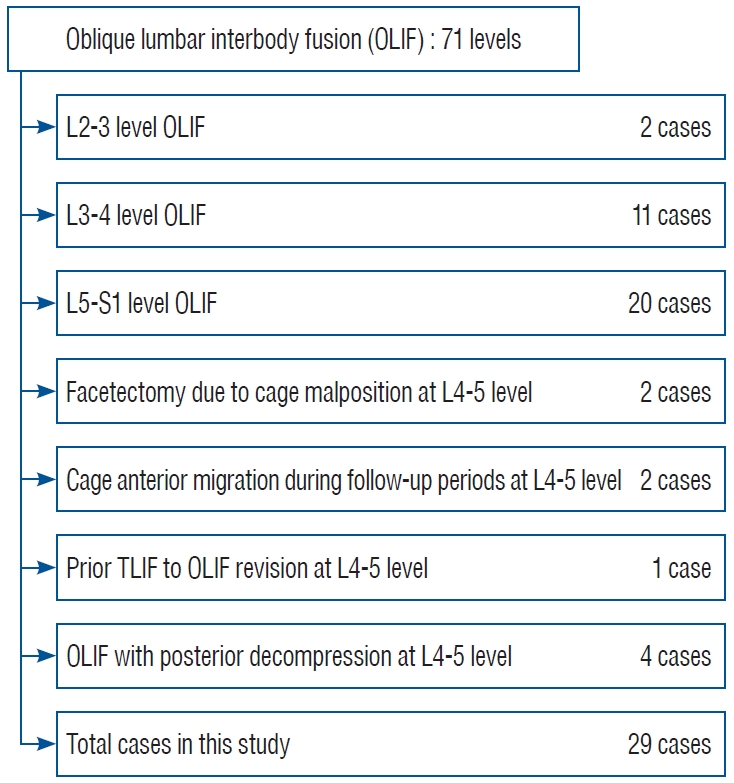
Fig. 2.
Images illustrating the iliac crest height (A and B); lumbar flexibility (C), which is the difference between flexion and extension Cobb angles; the distance from the iliac artery to the origin of the psoas muscle (DIAPM; D); the angle between the origin of the psoas muscle and the center of the vertebral disc (APCVD; D); cage obliquity (E), which is measured based on a line perpendicular to the line from the spinous process to the center of the intervertebral disc and a line formed by the cage metallic marker; foraminal height (F) measured in sagittal view from the pedicle interior margin of the gastric vertebral body to the upper margin of the pedicle of the lower vertebral body; cage location ratio (G) calculated by the center of the cage compared to the upper endplate of the caudal vertebral body (“2”/”1”) [ 21]. 
Fig. 3.
Three factors that affect cage obliquity angle : iliac crest height, APCVD, and DIAPM. The linear regression graphs for these three factors are shown in (A-C), respectively. APCVD : angle between the origin of the psoas muscle and the center of the vertebral disc, DIAPM : distance from the iliac artery to the origin of the psoas muscle. 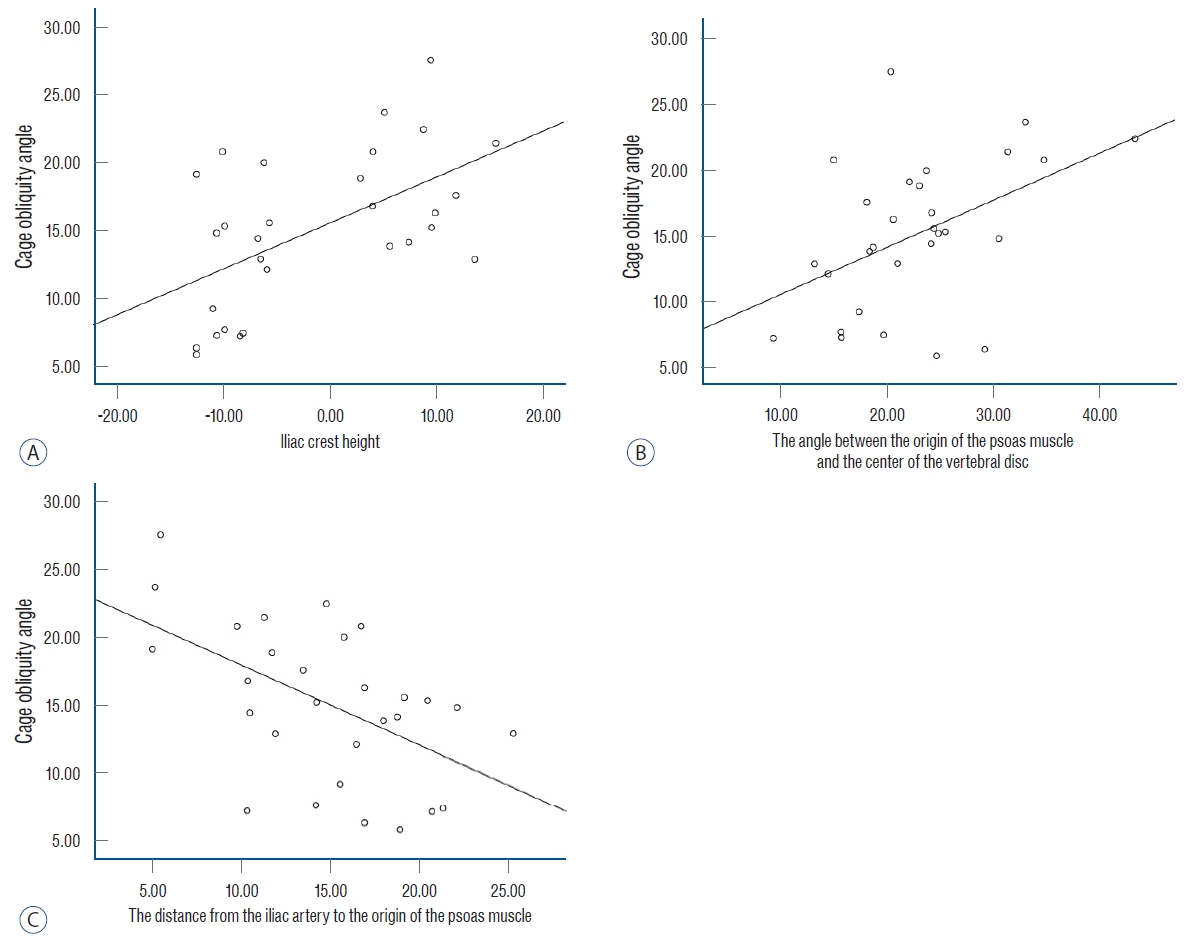
Fig. 4.
Linear regression shows the relationship between cage obliquity angle and postoperative 1-year index level segmental lumbar lordotic angle (A) and cage-induced segmental lumbar lordotic angle, which is the difference between the index level segmental lumbar lordotic angle and the cage angle used (B). LL : lumbar lordosis. 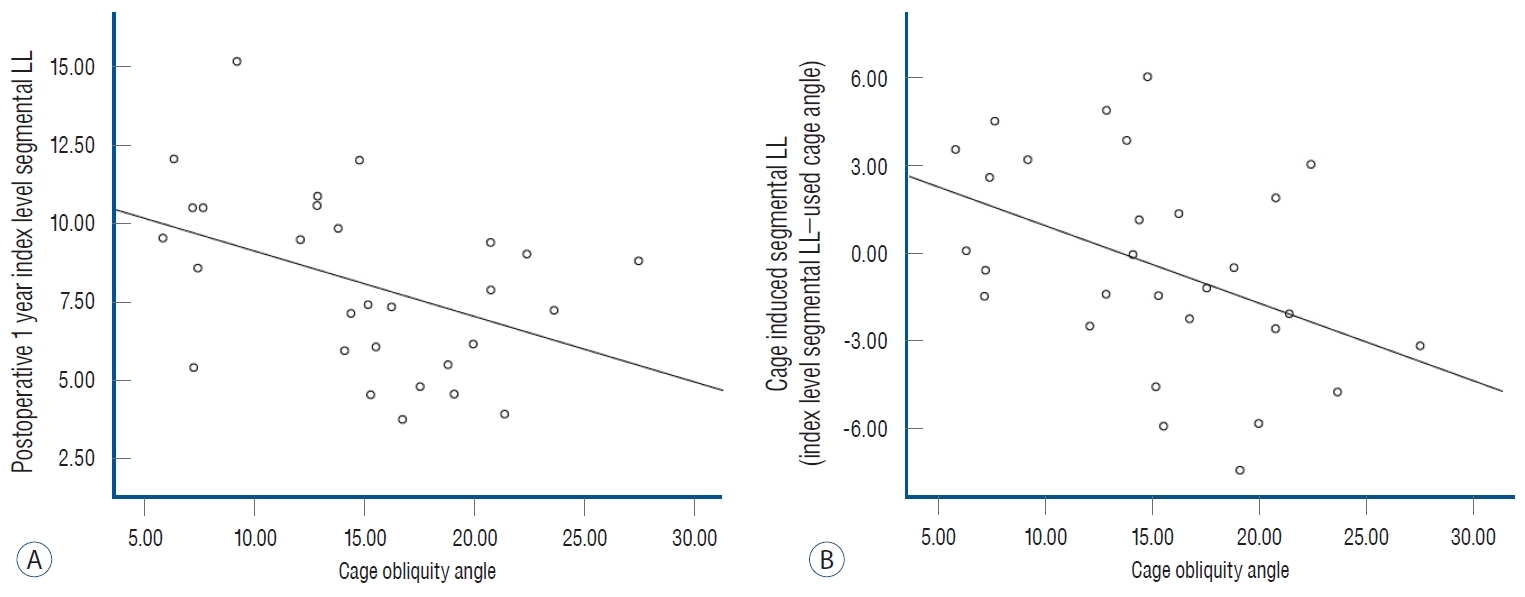
Fig. 5.
Receiver-operating characteristic (ROC) curve of the APCVD. The area under the ROC (AUC) curve for a cage obliquity angle greater than 15° after oblique lateral interbody fusion (OLIF) is 0.757. When the cutoff value of the APCVD is calculated as 21.58°, the sensitivity, and specificity are 73.3% and 71.4%, respectively. APCVD : angle between the origin of the psoas muscle and the center of the vertebral disc. 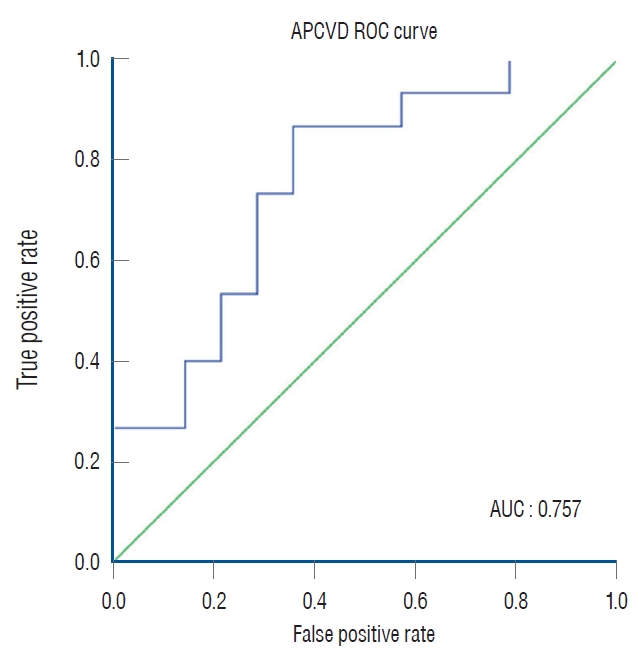
Fig. 6.
Classification according to the locations of the left psoas muscle and the major artery as a result of the study and the distribution of patients in this paper according to this classification. Adopted from Wang et al. [ 23]. 
Table 1.
characteristics of demographic data for patients who underwent OLIf surgery at L4-L5
|
Value |
|
Total number of patients |
29 |
|
Age (years) |
44.8±8.9 (19 to 58) |
|
Height (cm) |
174.8±5.2 (165 to 186) |
|
Weight (kg) |
82.4±11.7 (65 to 104) |
|
DM, yes/total |
4/29 |
|
Smoking, yes/total |
25/29 |
|
BMI (kg/m2) |
26.9±3.4 (21.1 to 33.2) |
|
Index level left psoas volume |
20.8±3.5 (13.0 to 26.5) |
|
TPAI |
10.2±1.8 (7.6 to 13.5) |
|
DIAPM |
14.8±5.2 (4.9 to 25.3) |
|
APCVD |
22.7±7.3 (9.3 to 43.4) |
|
Preoperative PI |
46.7±9.2 (29.0 to 63.0) |
|
Iliac crest height |
-1.3±9.4 (-12.5 to 15.7) |
|
Index level flexibility (flexion-extension angle) |
13.4±6.6 (1.8 to 28.6) |
|
Cage angle used |
|
|
6º |
17 |
|
10º |
2 |
|
Cage height used |
|
|
10 mm |
12 |
|
12 mm |
15 |
|
14 mm |
10 |
|
16 mm |
2 |
Table 2.
Twelve-month postoperative radiological parameters
|
Value |
|
Total number of patients |
29 |
|
Cage obliquity angle |
15.1±5.7 (5.8 to 27.5) |
|
Cage location ratio |
47.9±8.5 (33.4 to 69.9) |
|
LL changes |
2.0±7.6 (-11.4 to 11.8) |
|
SVA changes |
0.4±5.2 (-7.3 to 8.5) |
|
Index level SLA changes |
1.8±4.2 (-6.2 to 13.1) |
|
Index level SCA changes |
-0.47±1.8 (-3.2 to 4.7) |
|
Index level DAH changes |
4.2±2.7 (-2.1 to 10.2) |
|
Index level FH changes |
5.4±3.3 (0.3 to 14.0) |
|
Cage induced segmental LL, postoperative index level SLA - used cage angle |
-0.4±3.5 (-7.5 to 6.0) |
|
Cage induced disc height, postoperative index level DAH - used cage height |
-0.1±1.9 (-5.9 to 3.2) |
|
Fusion grade |
1.7±0.5 |
|
Subsidence rate |
2 of 29 |
Table 3.
Pre- and postoperative radiographic values
|
Parameter |
Preoperative |
Postoperative |
p-value |
|
LL |
40.8±9.9 (21.2 to 68.0) |
43.2±9.9 (25.9 to 60.0) |
0.48 |
|
SVA |
2.3±3.0 (-3.2 to 11.7) |
2.7±3.9 (-3.0 to 9.2) |
0.79 |
|
Index level SLA |
6.3±4.3 (-5.7 to 14.9) |
8.1±2.8 (3.7 to 15.2) |
0.07 |
|
Index level SCA |
1.6±1.5 (0.1 to 6.0) |
1.9±1.3 (0.1 to 4.3) |
0.41 |
|
Index level DAH |
8.4±3.6 (1.8 to 14.9) |
12.8±2.2 (8.0 to 16.3) |
<0.05 |
|
Index level FH |
17.8±2.8 (12.9 to 24.1) |
23.2±3.1 (18.0 to 29.7) |
<0.05 |
Table 4.
Single linear regression analysis of the correlation between cage obliquity angle and other factors (n=29)
|
R2
|
p-value |
|
Age (years) |
0.001 |
0.84 |
|
Height (cm) |
0.005 |
0.73 |
|
Weight (kg) |
0.075 |
0.15 |
|
BMI |
0.099 |
0.09 |
|
DM |
0.043 |
0.28 |
|
Smoking |
0.002 |
0.81 |
|
Preoperative PI |
0.029 |
0.37 |
|
Preoperative LL |
0.001 |
0.90 |
|
Preoperative SVA |
0.066 |
0.21 |
|
Preoperative FH |
0.084 |
0.15 |
|
Preoperative index level SLA |
0.018 |
0.49 |
|
Preoperative index level SCA |
0.033 |
0.10 |
|
Index level left psoas muscle volume |
0.014 |
0.54 |
|
TPAI |
0.046 |
0.27 |
|
DIAPM |
0.28 |
0.003*
|
|
APCVD |
0.21 |
0.012*
|
|
Iliac crest height |
0.31 |
0.002*
|
|
Preoperative index level DAH |
0.021 |
0.46 |
|
Index level flexibility (flexion-extension angle) |
0.02 |
0.52 |
|
Cage location ratio |
0.02 |
0.52 |
|
Postoperative 1 year index level SLA |
0.18 |
0.02*
|
|
Postoperative 1 year index level SCA |
0.095 |
0.35 |
|
Cage induced segmental LL, postoperative index level SLA - used cage angle |
0.19 |
0.02*
|
|
Cage induced disc height, postoperative index level DAH - used cage height |
0.02 |
0.49 |
|
Index level DAH changes |
0.00 |
0.94 |
|
Index level FH changes |
0.03 |
0.38 |
|
Fusion grade |
0.00 |
0.91 |
|
Subsidence rate |
0.005 |
0.72 |
Table 5.
Multiple linear regression analysis of the correlation between cage obliquity angle and other factors
|
Parameter |
Non-standardized coefficient
|
Standardized coefficient
|
T |
p-value |
TOL |
VIF |
|
B |
SE |
ß |
|
Constant |
13.062 |
3.116 |
|
4.192 |
0.000 |
|
|
|
DIAPM |
-0.318 |
0.142 |
-0.330 |
-2.239 |
0.037 |
0.901 |
1.110 |
|
APCVD |
0.325 |
0.087 |
0.524 |
3.730 |
0.001 |
0.989 |
1.011 |
|
Iliac crest height |
0.174 |
0.077 |
0.334 |
2.278 |
0.034 |
0.909 |
1.100 |
|
F(p) |
10.415 (0.000) |
|
Adjusted R2
|
0.551 |
|
Durbin-Watson |
2.418 |
Table 6.
The correlation analysis between dIaPM, aPcVd, and iliac crest height, which have been identified as risk factors
|
DIAPM |
APCVD |
Iliac crest height |
|
DIAPM |
|
|
|
|
Pearson correlation coefficient (R) |
1 |
|
|
|
p-value |
|
|
|
|
APCVD |
|
|
|
|
Pearson correlation coefficient (R) |
-0.049 |
1 |
|
|
p-value |
0.799 |
|
|
|
Iliac crest height |
|
|
|
|
Pearson correlation coefficient (R) |
-0.351 |
0.066 |
1 |
|
p-value |
0.062 |
0.735 |
|
Table 7.
comparison of demographic data and pre- and postoperative radiographic parameters between a group with a cage obliquity angle greater than 15° and a group with a cage obliquity angle less than 15°
|
Parameter |
Small cage obliquity angle group (n=14) |
Large cage obliquity angle group (n=15) |
p-value |
|
Cage obliquity angle (°) |
10.4±3.4 |
19.4±3.5 |
<0.05 |
|
Age (years) |
46.3±9.7 |
43.4±8.2 |
0.39 |
|
Height (cm) |
173.6±6.7 |
175.9±3.2 |
0.26 |
|
Weight (kg) |
81.9±11.2 |
82.9±12.5 |
0.81 |
|
BMI |
27.1±2.5 |
26.8±4.1 |
0.84 |
|
DM |
2 |
2 |
0.94 |
|
Smoking |
13 |
12 |
0.33 |
|
Preoperative PI |
45.0±9.6 |
48.2±8.8 |
0.36 |
|
Preoperative LL |
42.0±9.6 |
39.5±7.2 |
0.47 |
|
Preoperative SVA |
1.6±2.4 |
3.1±3.4 |
0.23 |
|
Preoperative index level FH |
16.3±2.1 |
19.3±2.7 |
0.004 |
|
Preoperative index level SLA |
7.2±4.3 |
5.4±4.2 |
0.25 |
|
Preoperative index level SCA |
1.8±1.8 |
1.5±1.1 |
0.56 |
|
Preoperative index level DAH |
7.9±4.4 |
8.9±2.7 |
0.51 |
|
Index level left psoas muscle volume |
20.6±3.3 |
20.9±3.8 |
0.85 |
|
TPAI |
10.2±2.1 |
10.3±1.6 |
0.97 |
|
DIAPM |
17.2±4.5 |
12.6±4.9 |
0.015 |
|
APCVD |
19.4±6.0 |
25.6±7.2 |
0.019 |
|
Iliac crest height |
-5.4±8.2 |
2.5±9.0 |
0.02 |
|
Index level flexibility (flexion-extension angle) |
14.0±6.7 |
12.9±6.8 |
0.70 |
|
Cage location ratio |
47.0±8.6 |
48.8±8.7 |
0.56 |
|
Postoperative index level FH |
22.3±3.7 |
24.1±2.1 |
0.14 |
|
Postoperative 1 year index level SLA (°) |
9.8±2.6 |
6.4±1.9 |
0.00 |
|
Postoperative 1 year index level SCA |
2.0±1.3 |
1.9±1.4 |
0.85 |
|
Postoperative index level DAH |
13.1±2.3 |
12.6±2.1 |
0.61 |
|
Cage induced segmental LL, postoperative index level SLA - used cage angle (°) |
1.7±2.7 |
-2.4±3.0 |
0.001 |
|
Cage induced disc height, postoperative index level DAH - used cage height |
0.1±2.3 |
-0.3±1.6 |
0.56 |
|
Fusion grade |
1.8±0.4 |
1.7±0.5 |
0.67 |
|
Subsidence rate |
14 (0) |
15 (2) |
0.16 |
Table 8.
Variables associated with mean cage obliquity angle of 15 degrees after L4-L5 OLIf
|
Variable |
Univariate analysis
|
Multivariate analysis
|
|
OR (95% CI) |
p-value |
OR (95% CI) |
p-value |
|
DIAPM |
0.806 (0.665-0.978) |
0.029 |
|
|
|
APCVD |
1.175 (1.010-1.366) |
0.036 |
1.420 (1.035-1.947) |
0.03 |
|
Iliac crest height |
1.109 (1.011-1.217) |
0.029 |
|
|
References
1. Allain J, Dufour T : Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop Traumatol Surg Res 106 : S149-S157, 2020   2. Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K : Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976) 20 : 1410-1418, 1995  3. Chung NS, Lee HD, Jeon CH : Accuracy of the lateral cage placement under intraoperative C-arm fluoroscopy in oblique lateral interbody fusion. J Orthop Sci 23 : 918-922, 2018   4. Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B, et al : Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine 21 : 785-793, 2014   5. Fontes RB, Traynelis VC : Iliac crest osteotomy to enhance exposure of the L4-5 interspace in minimally invasive lateral transpsoas interbody fusion: a cadaveric feasibility study. J Neurosurg Spine 18 : 13-17, 2013   6. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S : Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976) 40 : E175-E182, 2015   7. Hwang SH, Park SW, Kim YB : Risk factors for symptomatic contralateral foraminal stenosis after unilateral transforaminal lumbar interbody fusion. World Neurosurg 133 : e452-e458, 2020   8. Jung JM, Chung CK, Kim CH, Yang SH, Won YI, Choi Y : Effects of total psoas area index on surgical outcomes of single-level lateral lumbar interbody fusion. World Neurosurg 154 : e838-e845, 2021   10. Lee YS, Park SW, Kim YB : Direct lateral lumbar interbody fusion: clinical and radiological outcomes. J Korean Neurosurg Soc 55 : 248-254, 2014    12. Liang Y, Zhao Y, Xu S, Zhu Z, Liu H, Mao K : Effects of different orientations of cage implantation on lumbar interbody fusion. World Neurosurg 140 : e97-e104, 2020   13. Lovecchio FC, Vaishnav AS, Steinhaus ME, Othman YA, Gang CH, Iyer S, et al : Does interbody cage lordosis impact actual segmental lordosis achieved in minimally invasive lumbar spine fusion? Neurosurg Focus 49 : E17, 2020  14. Mahatthanatrakul A, Kotheeranurak V, Lin GX, Hur JW, Chung HJ, Lokanath YK, et al : Do obliquity and position of the oblique lumbar interbody fusion cage influence the degree of indirect decompression of foraminal stenosis? J Korean Neurosurg Soc 65 : 74-83, 2022    15. Mayer HM : A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976) 22 : 691-699; discussion 700, 1997   16. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ : Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1 : 2-18, 2015   17. Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE : A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab 33 : 997-1006, 2008   18. Ozgur BM, Aryan HE, Pimenta L, Taylor WR : Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J 6 : 435-443, 2006   19. Parikh NP, Jhala AC : Contralateral lower limb radiculopathy following minimally invasive oblique lumbar interbody fusion in treatment of degenerative lumbar spine disease. J Minim Invasive Spine Surg Tech 6 : 109-114, 2021
20. Park KH, Chung HW, Lee HD, Jeon CH, Koh JH, Chung NS : Cage obliquity and radiological outcomes in oblique lateral interbody fusion. Spine (Phila Pa 1976) 48 : 1611-1616, 2023   21. Park SJ, Lee CS, Chung SS, Kang SS, Park HJ, Kim SH : The ideal cage position for achieving both indirect neural decompression and segmental angle restoration in lateral lumbar interbody fusion (LLIF). Clin Spine Surg 30 : E784-E790, 2017   22. Regev GJ, Haloman S, Chen L, Dhawan M, Lee YP, Garfin SR, et al : Incidence and prevention of intervertebral cage overhang with minimally invasive lateral approach fusions. Spine (Phila Pa 1976) 35 : 1406-1411, 2010  
|
|