Postoperative Clinical Outcome and Risk Factors for Poor Outcome of Foraminal and Extraforaminal Lumbar Disc Herniation
Article information
Abstract
Objective
We evaluated postoperative outcomes in patients who have lumbar foraminal or extraforaminal disc herniation (FELDH) and suggested the risk factors for poor outcomes.
Methods
A total of 234 patients were selected for this study. Pre- and post-operative Visual Analogue Scale (VAS) and Korean version Oswestry Disability Index (KODI) were evaluated and the changes of both score were calculated. Outcome was defined as excellent, good, fair, and poor based on Mcnab classification. The percentage of superior facetectomy was calculated by using the Maro-view 5.4 Picture Archiving Communication System (PACS).
Results
Paramedian lumbar discectomy was performed in 180 patients and combined lumbar discectomy was performed in 54 patients. Paramedian lumbar discectomy group showed better outcome compared with combined discectomy group. p value of VAS change was 0.009 and KODI was 0.013. The average percentage of superior facetectomy was 33% (range, 0–79%) and it showed negative correlation with VAS and KODI changes (Pearson coefficient : -0.446 and -0.498, respectively). Excellent or good outcome cases (Group I) were 136 (58.1%) and fair or poor outcome cases (Group II) were 98 (41.9%). The percentage of superior facetectomy was 26.5% at Group I and 42.5% at Group II. There was significant difference in superior facetectomy percentage between Group I and II (p=0.000).
Conclusion
This study demonstrated that paramedian lumbar discectomy with preservation of facet joints is an effective and good procedure for FELDH. At least 60% of facet should be preserved for excellent or good outcomes.
INTRODUCTION
There are several types of lumbar disc herniation. The most common type is that protrudes mediolaterally into the spinal canal (intracanalicular type), and others are types of foraminal and extraforaminal disc herniation. Some patients present with combined type of lumbar disc herniation, intracanalicular with foraminal or extraforaminal disc herniation. Foraminal or extraforaminal lumbar disc herniations (FELDH) were first described by Abdullah et al.1) in 1974. The overall incidence rates of FELDH ranges from 3% to 11%79). The studies about intracanalicular lumbar disc herniation have been performed by many authors, but a few studies about FELDH have been reported. In addition there have been some studies about postoperative outcome for FELDH. Ryang et al.18) found excellent or good outcomes in 57% of 48 patients, Donaldson et al.6) documented 72%, and Marquardt et al.13) presented 94.3% excellent or good outcomes. Until now, many surgical approaches have been introduced for FELDH, they can be classified as total facetectomy with or without fusion, and facet preserving microdiscectomy4). Especially, a paramedian microdiscectomy technique permits the direct access to far lateral lesions, minimizing violation of the facet joint20), so paramedian microdiscectomy has been accepted as the most useful technique for FELDH, in case of no preoperative instability. But, even though this technique is minimally invasive approach for far lateral lesions, mostly it requires partial removal of facet which can affect postoperative outcomes. The purpose of this study was to evaluate the postoperative outcomes of FELDH following surgery and identify the radiologic and operative risk factors related with poor outcomes.
MATERIALS AND METHODS
The clinical data of patients who underwent operation for FELDH between January 2009 and June 2012 were retrospectively reviewed. The indications for surgery was intractable leg pain resistant to conservative treatment which was confirmed by computed tomogram (CT) and magnetic resonance imaging (MRI) as FELDH. Revision operation, multilevel surgeries, fusion operation, greater than grade I spondylolisthesis, spinal infection, and systemic diseases affecting bone and joint were excluded.
Preoperative evaluations
Based on the chart review, we checked preoperative symptoms, neurologic examination, Visual Analogue Scale (VAS), and Korean version Oswestry Disability Index (K-ODI)10). Preoperative X-ray image, CT and MRI were obtained from all the patients. To determine the presence/absence of spondylolisthesis and wedging of index level, anterior-posterior and flexion-extension lumbar radiographs were checked.
Postoperative evaluations
Postoperative VAS and KODI were checked. We calculated postoperative change of VAS and KODI which were used to evaluate the risk factors associated with poor outcomes. Subjective satisfaction with the result of operation was classified as excellent, good, fair, and poor based on Macnab classification12). We reviewed surgical records to assess the type of surgeries (paramedian only or intracanalicular and paraisthmic combined approach) and the occurrence of intraoperative complications. The radiologist hired in our institute reviewed post-operative radiologic images including X-ray and MRI in order to evaluate whether the nerve root had been decompressed completely or not.
Surgical technique
Minimally invasive paramedian approach was used. Incision line was marked at the midpoint of lateral isthmus under fluoroscopic guidance before draping. Following a 3 cm paramedian vertical skin incision, fascia was incised longitudinally. After separation of multifidus and longissimus muscles, we confirmed lateral border of isthmus and self-retaining retractor was applied. Under the surgical microscope, we check lateral facet joint, isthmus and transverse process. To remove inter transverse ligament, superior lateral part of superior facet and upper border of the lower transverse process were drilled out. In the case of L5–S1 level, drilling the lateral border of isthmus was needed at L5 level to open the inter transverse and foraminal ligaments because the L5 isthmus was so wide that it covered intervertebral foramen entirely. But we tried to preserve isthmus more than 5 mm, not to cause post-surgical spondylolysis as mentioned by MacNab12).
After removal of inter transverse and foraminal ligament, we checked the upper pedicle and confirmed the exiting nerve root lying just beneath the pedicle. Typically, the nerve root was displaced cranially by the herniated disc. During the removal of herniated disc by pituitary forceps, we did not use nerve root retractor to avoid injury of the dorsal root ganglion. In the case of double disc herniation (combination of intracanalicular disc herniation at the same level), intracanalicular discectomy was performed simultaneously.
Revision surgeries
We investigated the causes of revision surgeries and duration between first operation and revision surgeries. Types of revision surgeries were classified through chart review and postoperative radiologic study. The disc herniation of contralateral side at the previous operation level was also included in the indication for revision surgery.
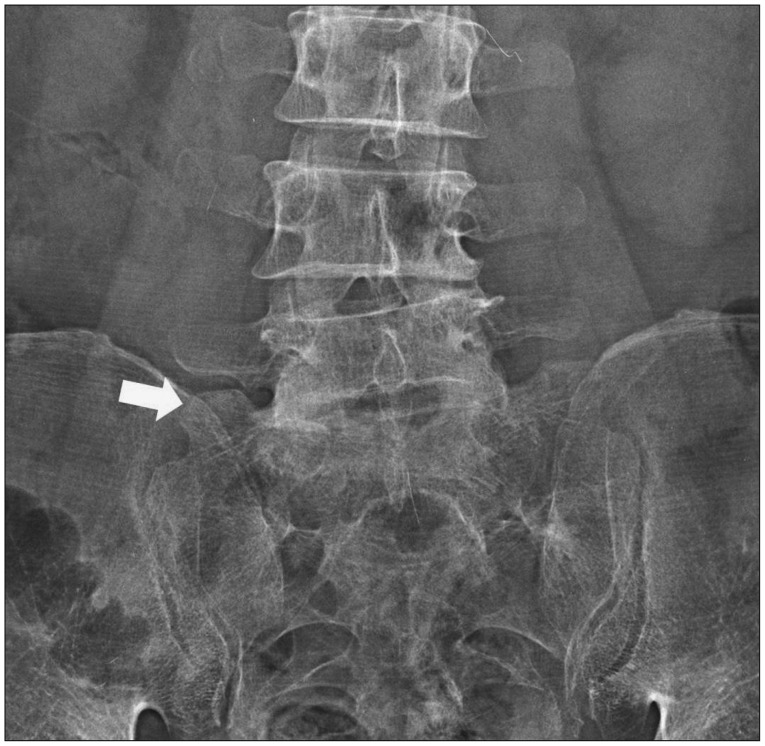
Facetectomy
To remove inter transverse ligament and open intervertebral foramen, partial resection of superior lateral aspect of facet joint was needed, generally. But too large resection of facet joint can cause severe disc space narrowing and segmental instability resulting in poor outcome. We surveyed the percentage of facetectomy using Maro-view 5.4 Picture Archiving Communication System (PACS) and analyzed correlation between the amount of facetectomy and poor outcome. We measured cross sectional area of facet between 3 lines (lower endplate of upper vertebra body, disc space, and upper endplate of lower vertebra body) (Fig. 1, 2). The sum of three cross sectional area of facet was calculated and the differences between pre and post-operative total facet cross sectional area were defined as the percentage of facetectomy.
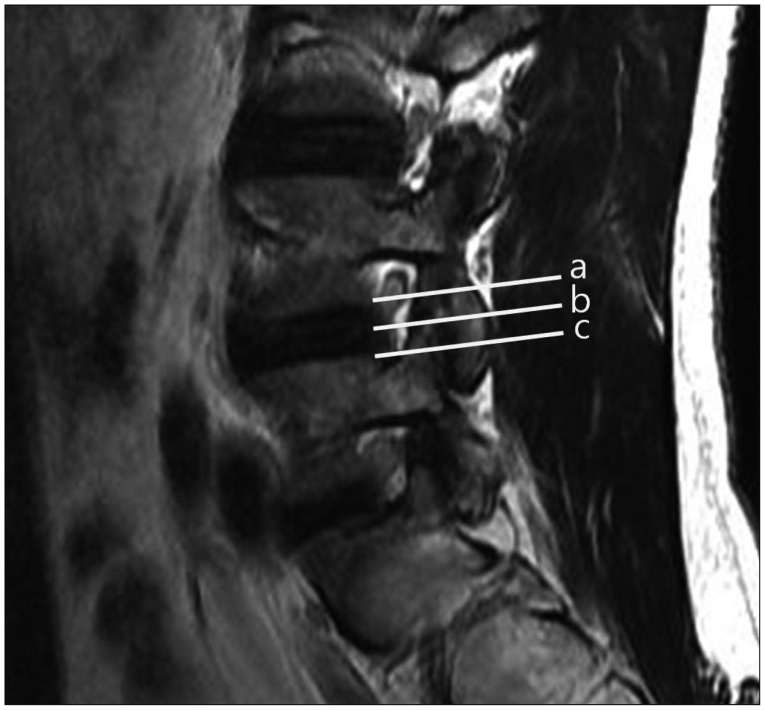
Cross sectional areas of facet joint were check between three lines (a : upper endplate, b : disc space, c : lower endplate).
Statistical analysis
The statistical analyses were conducted using SPSS 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Student's t-test and Pearson correlation coefficients values were calculated. Null hypotheses of no difference were rejected if p-value were less than 0.05.
RESULTS
A total of 234 patients were included in this study. The patients' group was composed of 96 (41%) males and 138 (59%) females. The mean age of patients was 61.8 (range, 18–92 year) years old. The number of patients at each level were 4 (1.7%) at L2–3, 23 (9.8%) at L3–4, 86 (36.8%) at L4–5, and 121 (51.7%) at L5–S1. Preoperative total VAS and KODI were 7.5 (range, 2–10) and 30.2% (range, 11–54%). Postoperative VAS and KODI were 3.6 (range, 0–9) and 20.3% (range, 2–52%). The changes of VAS and KODI were 3.9 (-5–10) and 9.9% (-35–44%). Total follow-up period was 33.0 months (range, 11.1–70.0).
Wedging and spondylolisthesis
Fifty patients (21.4%) showed lateral wedging or less than grade I spondylolisthesis on preoperative radiograph. The changes of VAS and KODI between pre and post operation were 3.6 (range, -3–10) and 7.9% (range, -20–36%) in the lateral wedging or spondylolisthesis group. The rest of them (184 patients, 78.6%) showed no lateral wedging and spondylolisthesis, the changes of VAS and KODI were 4.0 (range, -5–10) and 10.4% (range, -35–44%). There were no significant differences of VAS and KODI postoperative changes between two groups (p=0.308 and 0.201, respectively).
Paramedian versus combined discectomy
180 (76.9%) patients were given paramedian discectomy and combined discectomy was performed in 54 (23.1%) patients. It revealed that the changes of VAS and KODI between pre and post-operative surgeries were 4.2 (range, -3–10) and 11.0% (range, -35–40%) respectively in paramedian discectomy group. The combined discectomy group showed that the changes of VAS and KODI were 3.1 (range, -5–10) and 6.3% (-13–44%). There were significant differences of VAS and KODI changes between paramedian and combined discectomy groups (p=0.009 and 0.013, respectively). In the paramedian discectomy group, there were 113 (62.8%) patients showing excellent or good outcome and 67 (37.2%) patients showing fair or poor outcome. Among the combined discectomy group, 23 (42.6%) patients showed excellent or good outcome and 31 (57.4%) patients showed fair or poor outcome.
Revision surgeries
Thirteen (5.6%) patients required revision surgeries due to recurrent leg pain. The mean interval between primary and revision surgery was 7.4 months (range, 1–36 months). Revision surgeries were performed at L5–S1 level in 10 (77%) cases and L4–5 level in 3 (23%) cases respectively. The reasons of revision surgeries were recurrent foraminal disc herniation at 6 patients, contralateral disc herniation at 1 patient, foraminal stenosis at 2 patients, and extraforaminal stenosis at 4 patients. The summary of revision cases was described at Table 1.
Facetectomy
The mean percentage of facetectomy was 33% (range, 0–79%). It showed negative correlation with VAS and KODI changes (Pearson coefficient with VAS change : -0.446, p=0.000 and KODI change : -0.498, p=0.000). The more facetectomy was done, the worse outcomes were presented.
Outcomes
The outcomes were measured by using Macnab criteria12), which contains considerations of primarily back pain and radicular pain, activity as major variables, and neurologic deficits. Of the 234 patients, there were excellent outcomes in 22 (9.4%) patients, good in 114 (48.7%), fair in 46 (19.7%), and poor in 52 (22.2%) patients respectively in this study. According to the levels, there were excellent or good outcomes in 3 (75%) of 4 patients at L2–3 level, in 15 (65.2%) of 23 at L2–3 level, in 56 (65.1%) of 86 at L4–5 level, and in 64 (52.9%) of 121 at L5–S1 level respectively. Total 136 (58.1%) of 234 patients presented excellent or good postoperative outcomes. The group with excellent or good outcomes revealed that their mean percentage of facetectomy was 26.5%. Otherwise, the mean percentage of facetectomy was 42.5% in the group with fair or poor outcomes. There was significant difference in facetectomy percentage between the two groups (p=0.000).
DISCUSSION
FELDH is a rather uncommon pathology of nerve root entrapment in which the incidence ranges from 1 to 10%2681017). The radicular pain caused by FELDH is frightfully severe and sometimes even excruciating. More often than not, some patients should use wheelchairs for hospital visits. This striking feature is caused by a direct compression of dorsal root ganglion. Weinstein22) has described the dorsal root ganglion as the brain of the spinal motion segment. Important sensory synapse and many chemical mediators of pain lie within the ganglion. Many patients with FELDH can't bear weight on the affected limb, making you consider hip or pelvic fracture, otherwise coughing and sneezing do not often increase the pain because the lesion lies beyond the nerve root sheath5). To further confuse the clinical presentation, patients often present inguinal pain. It is because that disc herniation lies close to the psoas, causing referred inguinal pain14).
There are various surgical approaches to the excision of FELDH such as traditional interlaminar midline approaches with hemilaminectomy, the midline submuscular dissection expanded to go lateral to the pars interarticularis, the paraspinal/paraisthmic (paramedian) approach, the posterolateral approach, the retroperitoneal approach and endoscopic approach14). The paramedian approach has been used in our patients. This approach is safer and more minimally invasive than other procedures. Although it is minimally invasive method, during the procedure partial facetectomy is needed especially at L4–5, L5–S1 levels. Excessive facetectomy can cause segmental instability and asymmetrical disc space collapse, leading to postoperative foraminal stenosis and recurrent disc herniation. Lots of authors mentioned that 50% of the facet joint had to remain as a minimum requirement for segmental stabilization47). Our data showed that negative correlation between the amount of facetectomy and clinical outcomes. In addition, the mean percentage of facetectomy was 42.5% in the group with fair and poor outcomes. These results mean that at least 60% of facet joint should be preserved during the operation for FELDH. To the best of our knowledge, it is the first paper to propose the acceptable percentage of facetectomy by method for calculating cross sectional area of facet joint.
Intracanalicular approach combined with paraisthmic approach was effective for double disc herniation and bony foraminal stenosis3911). The incidence of double disc herniation was 23% in this study. It was slightly higher rate than that of other studies24). There would be high possibility of excessive facetectomy which can cause poor outcomes in the combined approach. Chang et al.4) presented that the patients with double disc herniation were almost three times more likely to have remaining or recurrent leg pain. In our cases, intracanalicular approach combined with paraisthmic approach showed poor outcome, also. The reason for poor outcome was that combined discectomy made greater facet and annular removal which could cause segmental instability and disc space collapse, even we tried to preserve the isthmus at least 5 mm, not to cause post-surgical spondylolysis as mentioned by MacNab12). And the things which we included less than grade I spondylolisthesis and lateral wedging cases could be the another reason for the poor outcome, even these conditions didn't show statistical significance.
In our several combined disc herniation patients who were not included in present study, we performed posterolateral side approach to preserve facet and lateral isthmus as much as possible. This approach started with skin incision which was about 7 cm off the midline and we approached the foraminal area with about 30 degree inclination to see foramen directly without removal of facet and lateral isthmus, especially in L4–5 and L5–S1 levels. Through this approach, we have gotten good results in current several cases. Of course we have to stipulate the usefulness and validity of posterolateral approach, we just suggest this approach can be one of ways to preserve facet and lateral isthmus.
In our series, there were thirteen (5.6%) revision surgeries at L4–5 (23%) and L5–S1 (76%) levels. These results were comparable to those of other studies51316). Among the L5–S1 group, 4 (36%) cases showed extraforaminal stenosis. The cause of extraforaminal stenosis at L5–S1 level was L5 nerve root impingement between ala transverse process and extraforaminal bulged disc (Fig. 3). After the discectomy of foraminal lesion, disc height collapsed and lateral side disc bulged simultaneously. And the ala transverse process, especially superior lateral part, in these patients was found to be larger than those of other levels, so L5 nerve root was compressed easily (Fig. 4). This means that enough partial removal of alar transverse process is needed when we perform the operation for FELDH at L5–S1 level in order to prevent the postoperative extraforaminal stenosis. So we recommend that foraminal or coronal view MRI of L5–S1 level should be checked preoperatively to predict the possibility of L5 nerve root impingement between bulged disc and alar transverse process (Fig. 5).
Our series showed excellent or good outcomes in 58.1% patients. Otherwise, previous studies presented higher rates of excellent or good outcomes compared to our series461316181921). This reason was assumed that in our patients' group, there was higher rate of combined discectomy (23%) causing poor outcome and the mean age of the patients in this study was relatively older than those of the patients in previous studies.
There were some limitations. This was a retrospective study, so the level of evidence was low. And other factors, such as body mass index, occupations, smoking and alcoholic histories, affecting the outcomes were not evaluated. These factors should have been controlled for more statistically meaningful results. In the aspect of facetectomy percentage, we used cross sectional areas. But this method was not based on volumetric calculation. So, there could be a slight differences between our calculation results and real values.
CONCLUSION
Facet preserving minimally paramedian lumbar discectomy is an effective and good procedure for FELDH. At least 60% of facet should be preserved for excellent or good outcomes. Especially in the cases of combined lumbar discectomy, minimal facetectomy is needed. In the future, well controlled prospective randomized studies will be required.