Outcome Analysis of External Neurolysis in Posture-Induced Compressive Peroneal Neuropathy and the Utility of Magnetic Resonance Imaging in the Treatment Process
Article information
Abstract
Objective
We aimed to analyze the effectiveness of external neurolysis on the common peroneal nerve (CPN) in patients with posture-induced compressive peroneal neuropathy (PICPNe). Further, we aimed to examine the utility of magnetic resonance imaging (MRI) in assessing the severity of denervation status and predicting the postoperative prognosis.
Methods
We included 13 patients (eight males and five females) with foot drop who underwent CPN decompression between 2018 and 2020. We designed a grading system for assessing the postoperative functional outcome. Additionally, we performed MRI to evaluate the denervation status of the affected musculature and its effect on postoperative recovery.
Results
The median time to surgery was 3 months. The median preoperative ankle dorsiflexion and eversion grades were both 3, while the average functional grade was 1. Posterior crural intermuscular septum was the most common cause of nerve compression, followed by deep tendinous fascia and anterior crural intermuscular septum. There was a significant postoperative improvement in the median postoperative ankle dorsiflexion and eversion grades and average postoperative functional (4, 5, and 2.38, respectively). Preoperative ankle eversion was significantly correlated with denervation status. Additionally, the devernation status on MRI was positively correlated with the outcome favorability. However, denervation atrophy led to a less favorable outcome.
Conclusion
Among patients with intractable PICPNe despite conservative management, surgical intervention could clinically improve motor function and functional ability. Additionally, MRI examination of the affected muscle could help diagnose CPNe and assess the postoperative prognosis.
INTRODUCTION
Common peroneal neuropathy (CPNe) is a common lowerextremity entrapment neuropathy. The common peroneal nerve (CPN) has a superficial course and is located lateral to the bony structure, fibula, which makes it more vulnerable to external force than other peripheral nerves of the lower extremities [10,12]. Possible causes of CPNe include iatrogenic injury during knee and hip surgery, trauma, compression, and excessive weight loss. Additionally, it may be caused by certain postures, including habitual leg crossing [2,9,10]. The Asian population is especially vulnerable to such posture-induced CPNe (PICPNe) since leg crossing and kneeling are common cultural practices [6,13].
Diagnosis of PICPNe is primarily based on history taking and clinical presentations [13]. Patients with PICPNe present with dropped foot caused by weakness of ankle dorsiflexors and evertors as well as sensory disturbance in the anterolateral aspect of the affected leg. These symptoms have a sudden onset and can occur after prolonged exposure in a specific posture without trauma. Electro-diagnostic studies, including nerve conduction study (NCS) and electromyography (EMG), can be used to confirm this condition and assess CPN regeneration [2,10]. However, they are often uncomfortable and invasive, are influenced by the timing of examination, and can cause pain [11]. Given the need for comfortable and objective diagnostic methods, magnetic resonance imaging (MRI) has been used to detect signal changes in the affected nerve and denervated muscles compared with non-affected structures [1,11]. For PICPNe diagnosis, we examine the enlarged nerve with high-signal intensity and check for swollen or atrophic affected muscles on the anterolateral compartment of the leg. However, it remains unclear whether MRI findings are correlated with the prognosis or severity of PICPNe.
PICPNe can be treated using non-surgical methods, including non-steroidal anti-inflammatory drugs, physiotherapy, and avoiding postures that exert external force on the CPN [9,10]. In case of no improvement, surgery for external neurolysis and decompression at the fibular head may be considered [4,7,10,12]. Most studies on the effectiveness of surgical treatment were based on CPNe caused by trauma and iatrogenic entities. Additionally, surgical outcomes for PICPNe exclusively remain unclear. Therefore, this study aimed to assess the effectiveness of external neurolysis for treating PICPNe and the utility of MRI in predicting surgical outcomes.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Hallym University (IRB 2020-06-005), Chuncheon, Korea.
Patient selection and data
A total of 44 patients were diagnosed with CPNe between 2018 and 2020. We excluded patients with non-posture-induced etiologies and those who did not undergo surgery. Additionally, we excluded one patient with sensory disturbance only, who completely recovered after CPN decompression. Finally, we included 13 patients (eight males and five females). Most patients were diagnosed using electrodiagnostic studies and MRI. We collected the following baseline characteristics from the medical records : sex; age; comorbidities, especially diabetes mellitus; time from onset of dropped foot to surgery (time to surgery); follow-up duration; and preoperative and postoperative Medical Research Council (MRC) grades of ankle dorsiflexion and eversion.
Assessment of surgical outcomes
To analyze the postoperative functional outcomes regarding walking, we designed a simple grading system for active movement. Since gait disturbance caused by dropped foot primarily results from weakening of the weakened ankle dorsiflexor, the grading system primarily focused on the ankle dorsiflexion motion in order to evaluate the ability to effectively push the ground and continue propulsion. To ensure that the ankle joint was in a neutral position, the patients were seated on the bed with their legs and feet relaxed and lifted from the floor. Subsequently, the physicians confirmed that there was no contracture in the affected ankle joint. Next, the patients were instructed to extensively dorsiflex the ankle on the affected leg and were assigned grades ranging from 0 to 3. Grade 0 was defined as the lack of an active range of motion. Grade 1 was assigned if the patient could dorsiflex the ankle but could not raise it to 0 degrees. Grade 2 was assigned if the ankle could be raised up to 0 degrees but the full range of passive movement could not be achieved. Grade 3 was assigned if the patient could dorsiflex the ankle through the full range of passive movement. The preoperative and postoperative functional grades were obtained and compared (Fig. 1).
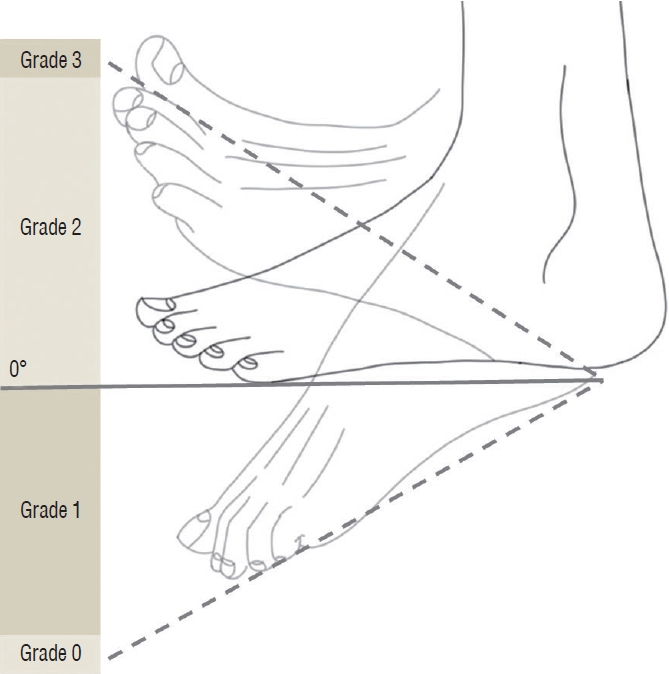
The functional grade of the common peroneal nerve. Grade 1 was assigned if the patient could dorsiflex the ankle but could not raise it up to 0 degrees. Grade 2 was assigned if the ankle could be raised up to 0 degree but the full range of passive movement could not be achieved. Grade 3 was assigned if the patient could dorsiflex the ankle through the full range of passive movement. The preoperative and postoperative functional grades were obtained and compared. Authors modified an original artwork from "WIKIMEDIA COMMONS".
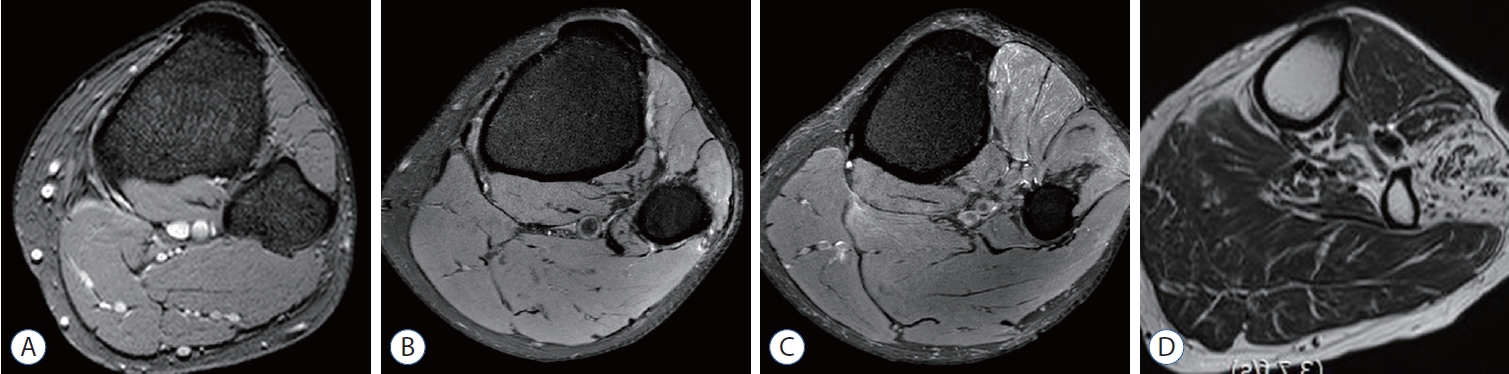
Analysis of MRI findings at the anterolateral muscle compartment
Patients underwent an axial MRI using a 1.5 Tesla scanner (Gyroscan Intera; Philips Medical Systems, Best, the Netherlands) from the apex of the popliteal fossa to 20 cm distal to the fibular head. MRI findings were classified to reflect the time course of muscle denervation at the level of the fibular tunnel (Fig. 2). An MRI finding of only edema (increased water signal) in the affected muscles was classified as type 1. An MRI finding of fatty infiltration within the muscles, with or without edema, was classified as type 2. Finally, an MRI finding of apparent muscle atrophy was classified as type 3. Fig. 3 shows examples of the aforementioned MRI findings. Muscle appearance (peroneus longus, extensor digitorum longus, and tibialis anterior) on the MRI was cross-checked by two clinicians (a radiologist and neurosurgeon).
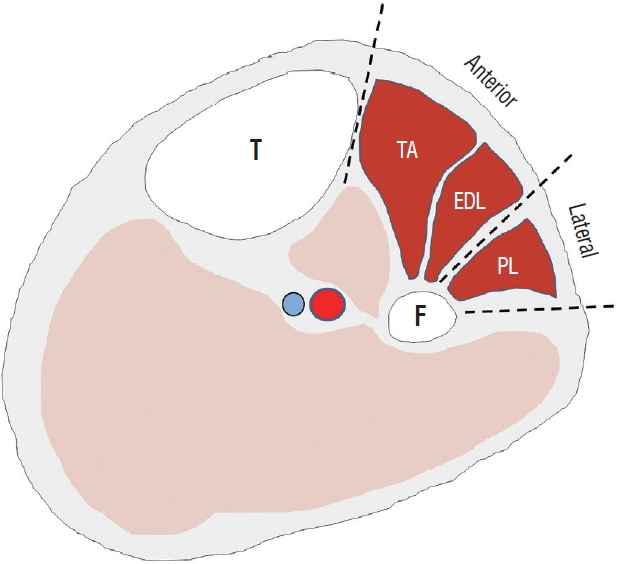
Schematic description of the right knee muscles and compartments for diagnosis of common peroneal neuropathy. We focused on the appearances of these three muscle (TA, EDL, and PL). Reprinted with permission from The Nerve (2021, Choi et al.). T : tibia, anterior : anterior compartment, TA : tibialis anterior muscle, EDL : extensor digitorum longus muscle, lateral : lateral compartment, PL : peroneus longus muscle, F : fibular.
Surgical techniques
Patients were placed under general anesthesia and in the supine position, with their knees on the affected side flexed by 60°. If possible, the CPN was palpated; otherwise, it was preoperatively located using a musculoskeletal ultra-sonogram. We made a curved incision just below the lateral aspect of the fibula head. The subcutaneous tissues were dissected to distally expose the CPN in order to determine the entrapment or compression sites responsible for dropped foot. We carefully examined hypertrophy of deep tendinous fascia as well as anterior and posterior crural intermuscular septum. Additionally, we examined the growth of adhesion tissues around the CPN course. After determining the appropriate target for septum resection, external neurolysis was performed. In case there was appropriate decompression, an anti-adhesion barrier agent was applied in the operative field. Subsequently, the surgical wound was closed layer-by-layer.
Statistical analysis
Given the small sample size, the normality of distribution was first checked using the Shapiro-Wilk test. Some variables, including the time to surgery as well as the preoperative and postoperative functional grades, showed a non-normal distribution. The Wilcoxon signed-rank test was performed to compare the preoperative and postoperative motor/functional grades. Additionally, we performed Pearson’s correlation analysis to examine the relationship of preoperative MRI appearances with preoperative motor and functional grades and the time to surgery. For normally distributed variables, we performed a one-way analysis of variance (ANOVA) to observe whether the time to surgery, as well as preoperative and postoperative motor and functional grades, showed certain tendencies according to the time course of muscle denervation shown on MRI. Subsequently, we performed the nonparametric Kruskal-Wallis test given the small sample size. A paired t-test and Mann-Whitney U test were used to examine the influence of muscle denervation on the variables. Statistical significance was set at p<0.05. Statistical analyses were performed using SPSS Statistics, version 27 (IBM Corporation, Armonk, NY, USA).
RESULTS
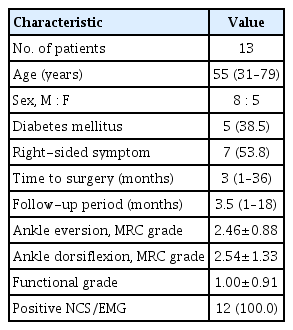
Baseline characteristics
Table 1 summarizes the baseline characteristics of the included patients. The median age was 55 years (31–79). Further, seven and six patients experienced right-sided and left-sided foot drop, respectively. Five patients had underlying diabetes mellitus. The median time to surgery and postoperative follow-up period were 3 months (1–36) and 3.5 months (1–18), respectively. The median preoperative MRC grades of ankle eversion and dorsiflexion were both 3, while the average values were 2.46 and 2.54, respectively. The average preoperative functional grade was 1. All patients who underwent NCS/ EMG showed positive findings, including positive sharp waves and fibrillation.
Intraoperative findings
The most common cause of PICPNe was hypertrophied posterior crural intermuscular septum and comorbid adhesion to the CPN (92.3%). Compression of deep tendinous fascia was observed in six patients (46.2%). Four patients (30.8%) showed hypertrophy of anterior crural intermuscular septum while two patients showed thickened intermuscular septum between extensor digitorum longus muscle and tibialis anterior muscle. These results for each patient are described in Table 2.
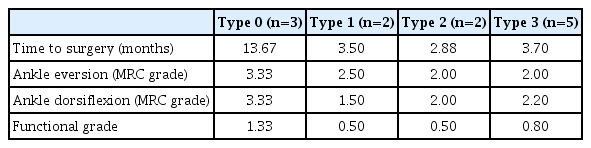
MRI findings
MRI scans were obtained from 12 patients. One patient did not consent to an MRI scan that was not covered by health insurance. In three patients (25%), muscles usually affected by PICPNe showed normal signal intensity. Nine patients (75%) showed muscle denervation; among them, two (22.2%), two (22.2%), and five patients (55.6%) showed type 1, 2, and 3 findings, respectively. Table 3 summarizes the descriptive statistics for the 12 patients stratified according to MRI findings.
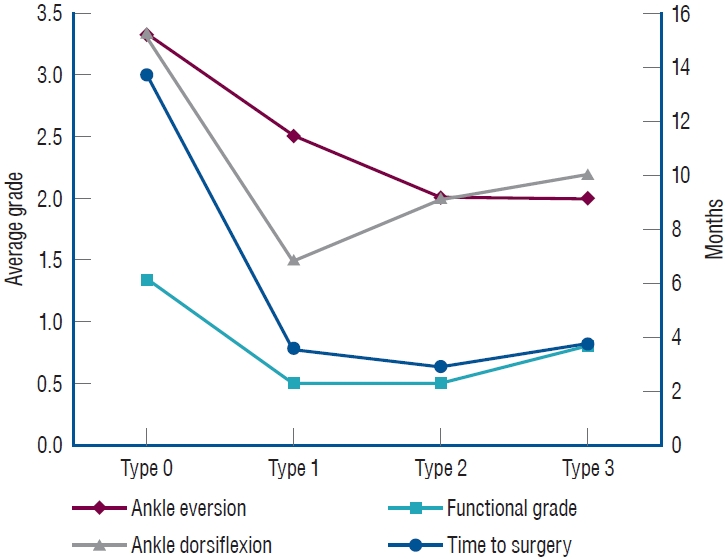
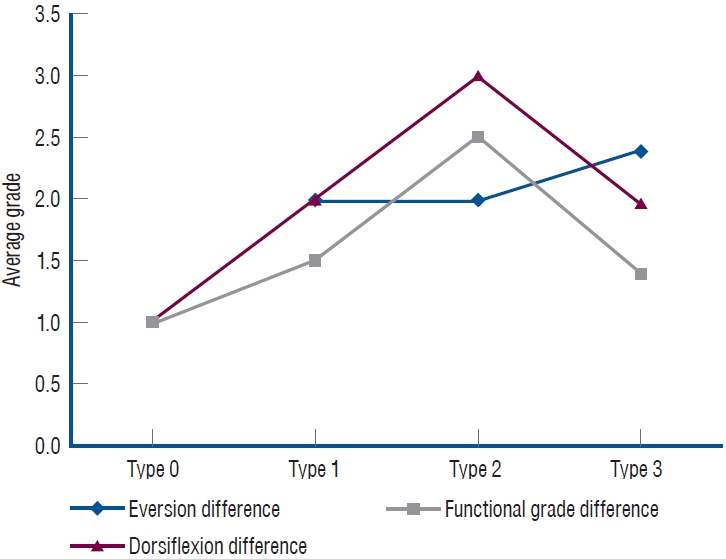
Pearson correlation analysis revealed a significant correlation of the preoperative ankle eversion grade with the type of MRI findings (correlation coefficient, -0.608; p<0.05). The time to surgery, preoperative grades of ankle dorsiflexion, and preoperative functional grades showed a non-significant negative trend according to the time course of muscle denervation (correlation coefficients : -0.371 [p=0.235], -0.306 [p=0.334], and -0.246 [p=0.441], respectively). There were no significant differences in the time to surgery as well as preoperative motor and functional grades according to the type of MRI findings. Similar findings were obtained after data stratification according to the presence of muscle denervation on MRI. There was no significant effect of muscle denervation on preoperative motor and functional grades. However, the average grades tended to decrease upon detection of muscle denervation as shown in Fig. 4.
Outcome analysis of motor weakness
The median postoperative MRC grades of ankle eversion and ankle dorsiflexion were 4 and 5, respectively, while the corresponding average values were 4.38 and 4.23. The median and average functional grades were 3 and 2.38, respectively. There was a significant postoperative improvement in ankle eversion, ankle dorsif lexion, and our designated grading (p<0.01 in all cases). Age and the presence of diabetes mellitus were not significantly correlated with the preoperative and postoperative motor and functional grades. Additionally, there was no correlation of the time to surgery with the preoperative motor and functional grade. Further, the time to surgery showed a non-significant negative correlation with the postoperative improvement in the motor and functional grades.
Additionally, we analyzed the effect of the preoperative presence of muscle denervation on surgical outcomes. The average postoperative ankle eversion grades were 4.33, 4.50, 4.00, and 4.40 for types 0, 1, 2, and 3, respectively. The average postoperative ankle dorsiflexion grades were 4.33, 3.50, 5.00, and 4.17 for types 0, 1, 2, and 3, respectively. The average preoperative functional grades were 2.33, 2.00, 3.00, and 2.20 for types 0, 1, 2, and 3, respectively. Postoperative changes in the ankle dorsiflexion and functional grades increased from type 0 to 2 but decreased at type 3. Postoperative changes in the ankle eversion grades gradually increased from type 0 to 3. These findings are graphically represented in Fig. 5. However, ANOVA or Kruskal-Wallis test did not reveal statistical significance. Similar results were obtained through stratification according to the presence of muscle denervation using the Mann-Whitney U test.
DISCUSSION
There have been few studies on PICPNe. Certain postures, including habitual leg crossing and squatting, have been shown to induce CPNe; however, there have been no studies on peroneal neuropathy exclusively caused by such postures. Yu et al. [13] and Kishi et al. [6] Have demonstrated the significance of PICPNe within the Asian population due to cultural factors. Specifically, although traditional eastern culture has been continuously replaced by western culture, poses such as kneeling on the floor and cross-legging remain widespread. This makes the Asian population more susceptible to CPNe. This is the first study to describe the effectiveness of surgical treatment in patients with PICPNe showing dropped foot.
Previously reported cases of idiopathic CPNe might comprise cases of PICPNe. Maalla et al. [7] reported the surgical outcomes of 15 patients with entrapment syndrome of the CPN; among them, 10 patients had idiopathic etiology, with nine showing favorable outcomes based on motor improvement and sensory changes. Wilson et al. [12] examined 21 patients with CPNe; among them, 15 patients had an idiopathic etiology. An excellent outcome was observed in 71.4% of the patients; moreover, no specific etiology was associated with poor outcome [12]. Humphreys et al. [4] reported the outcome of CPN decompressions in 48 patients, including 12 with idiopathic etiology. Among 47 patients with motor weakness, 40 showed significant post-compression improvement; however, they did not perform stratification according to etiology [4].
These previous findings are consistent with our findings. We observed significant improvement in motor weakness and functional status after external neurolysis and CPN decompression in patients with PICPNe. Only two patients did not show postoperative improvement in their functional grades (preoperative functional grades were 2 and 3; ankle dorsiflexion grades were 4 and 5; and ankle eversion grades were 4 and 3). Postoperatively, the MRC grades of ankle dorsiflexion were the same. However, the patient with grade 3 ankle eversion showed postoperative improvement to grade 5. The other patient showed the longest time to surgery (36 months). This suggests that the longer the time to surgery, the less favorable the outcome. Some studies have recommended surgical interventions if the dropped foot persists despite 3–6 months of conservative management, which is consistent with our findings.
Posterior crural intermuscular septum was the most frequent area of compression and CPN adhesion. Dellon et al. [3] reported that the fascial band distal to the superficial head of the peroneus longus muscle was the most vulnerable compression site in CPNe (incidence rate of 78.5% among 65 patients). In our study, the most common abnormality was hypertrophied posterior crural intermuscular septum with nearby adhesion around the CPN (92.3%), followed by hypertrophied deep tendinous fascia (46.2%). Contrastingly, Dellon et al. [3] reported only 6% of the patients showed fascial band compression between the soleus and peroneus longus muscles [5]. Compared with CPNe of other etiologies, PICPNe could show a higher frequency of hypertrophy of the deep tendinous; however, further research is warranted. In our study, the least common abnormality was hypertrophy of anterior crural intermuscular septum; contrastingly, it was the second most common abnormality (20%) in the study by Dellon et al. [3]. Taken together, when performing external neurolysis and decompression, it is important to investigate the aforementioned structures in order to allow maximal decompression, which is crucial for patient recovery.
The use of MRI in the diagnosis and treatment processes of CPNe has not been reported. Instead, NCS and EMG have been used to confirm the diagnosis and assess the re-innervation status [1,2,10,11]. However, there have been radiology studies seeking to replace these standard tools in compressive neuropathy given their invasiveness, practitioner-dependency, and induced pain. Viddeleer et al. [11] reported that the Short Tau Inversion Recovery (STIR) sequence was mainly used to monitor changes in the signal intensity of denervated muscles after treatment of treating traumatic nerve transection in patients with traumatic ulnar or median nerve injury. During a 12-month follow-up period, the signal intensity of the good and poor recovery groups normalized and remained high, respectively. These findings suggested that MRI can be harnessed to monitor the nerve regeneration status [11].
We investigated the utility of MRI in predicting prognosis and the correlation of denervation status with the severity of dropped foot. The duration until denervation was positively correlated with the severity of motor weakness. Additionally, type 1 or 2 MRI findings were associated with significant postoperative improvement in the motor grade. Furthermore, atrophic changes in the affected muscles indicated a poor prognosis. Although these findings were not statistically significant, the observed trend was consistent with our hypotheses. Further studies with larger sample sizes are warranted to test our hypotheses. Additionally, unlike Viddeleer et al. [11], we did not perform follow-up MRI examinations to confirm signal intensity normalization and its correlation with favorable outcomes. Further studies on CPNe are warranted to confirm our findings.
Besides the MRC grading system, there is no other grading scale for assessing functional disability from foot drop. Patients with dropped foot cannot comfortably maintain normal gait since the affected foot cannot effectively push the ground or sometimes hits the ground with the dorsum of the foot. To effectively assess patients with foot drop, functional evaluation along with MRC grading of the anterolateral compartment of the lower leg is necessary. Ninković and Ninković [8] proposed a grading scale for assessing functional outcomes after neuromusculotendinous transfer for peroneal neuropathy. However, Ninkovic grading requires clinicians to perform EMG and to evaluate ankle dorsiflexion and plantarflexion, active range of motion of the ankle, joint motion, and walking. Therefore, the evaluation process is time-consuming. Functional disability could be mainly attributed to weakened ankle dorsiflexion; therefore, we designed a scale focused on examining the ability to actively dorsiflex the ankle rather than all CPN motor functions, which allowed more concise functional outcome analysis.
A potential limitation of this study is its retrospective nature. Moreover, the small sample size impeded us from obtaining strongly significant results in the analyses regarding the types of MRI findings.
CONCLUSION
External neurolysis and decompression can effectively treat patients with PICPNe intractable to conservative management. Moreover, MRI examination of the denervated muscle could facilitate CPNe diagnosis and prognosis assessment.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Author contributions
Conceptualization : JY, YC; Data curation : JK, SK; Formal analysis : JJ; Funding acquisition : JY; Methodology : JY, HC; Project administration : HC, SK; Visualization : JK, JY; Writing - original draft : JK, JY; Writing - review & editing : JY, YC
Data sharing
None
Preprint
None
Acknowledgements
We would like to thank Editage (www.editage.co.kr) for English language editing.