Avoiding a Collision in Gamma Knife Radiosurgery : A Modified Mask Fixation Method
Article information
Abstract
Objective
The latest version of the Leksell Gamma Knife IconTM allows for mask- and frame-based fixation. Although mask fixation provides fractionated treatment and immobilization using a noninvasive method, it is not free from collision. The authors investigated the collision problem with a modified mask fixation method.
Methods
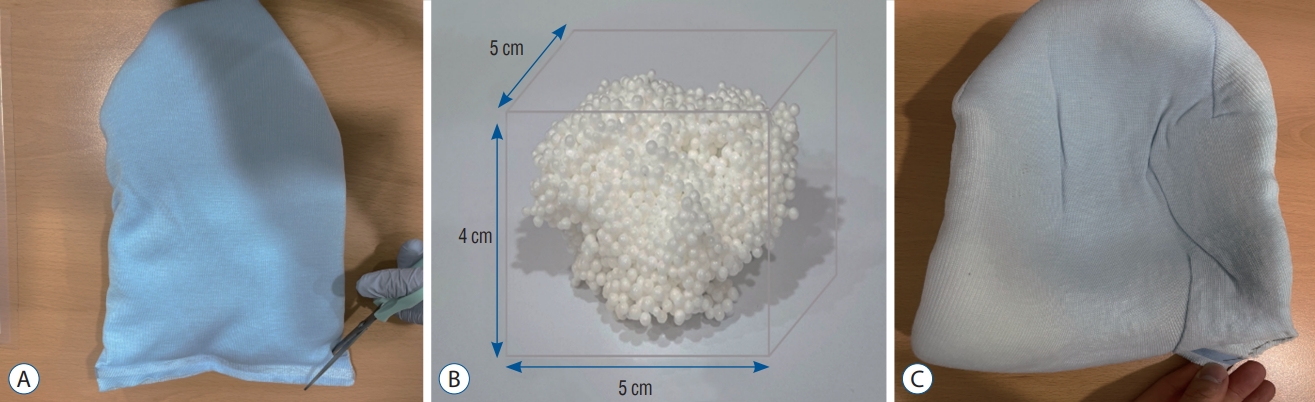
This study presents a case of two meningiomas in the frontal area, where a collision occurs in the occipital area. A modified mask fixation method was introduced to avoid the collision : first, the edges of the head cushion were cut off and polystyrene beads with a diameter of approximately 5 cm were removed. Next, the head cushion was sealed using a stapler. Finally, the head cushion was flattened in the adapter. We compared the shot coordinates, 3-dimensional (3D) error, clearance distance, and vertical depth of the head cushion between the initial and modified mask fixations.
Results
When comparing the initial and modified mask fixations, the difference in the shot coordinates was +10.5 mm along the y-axis, the difference in the 3D error was approximately 18 mm, and the difference in clearance was -10.2 mm. The head cushion was approximately 8 mm deeper in the modified mask fixation.
Conclusion
Based on these findings, we recommend a modified mask fixation method for gamma knife radiosurgery using ICON with a collision.
INTRODUCTION
The Leksell Gamma Knife (LGK) IconTM was introduced in 2016 as an upgrade on the LGK PerfexionTM model from 2006 [16]. It consists of 192 sealed cobalt-60 sources arranged in eight sectors, each containing 24 sources on the same radiation unit as in the previous model. Cone-beam computed tomography (CBCT) has been added to the LGK Icon to provide 3-dimensional (3D) stereotactic coordinates. CBCT can be acquired by either a high signal (computed tomography dose index [CTDI] 6.3 mGy) preset or lower dose (CTDI 2.5 mGy) and registered with the stereotactically defined image set for comparison between patient coordinates at the time of treatment and those at the time of imaging [5]. CBCT imaging and high-definition motion management (HDMM) systems based on infrared light have been introduced to provide submillimeter accuracy for stereotactic radiosurgery (SRS) treatment [2-4]. With the advent of LGK Icon, physicians are able to offer noninvasive mask fixation for SRS treatment to patients either unwilling or unable to undergo invasive frame fixation [6,7]. Infrequently, a treatment plan could be canceled if a planned beam cannot be delivered because of a collision between the collimator helmet and the patient’s skull or frame including the screw [11]. Treatment of lesions with collisions remains a challenge. This is because deeply anterior and inferior target locations can potentially be untreatable due to a collision between the patient and machine. If a collision occurs after frame fixation, then the frame position should be adjusted. However, this is excruciating for patients and stressful for medical staff. It is important to confirm the position of the frame so that the treatment target is located in the center of the frame as close as possible. Unlike frame fixation, no method has been suggested to adjust mask fixation. Current commercial moldable headrests are activated by heat or water and can only be shaped in a limited amount of time, which can make it challenging to place the patient in an optimal treatment position considering the geometrical limitations [1].
Herein, we present a case report of two meningiomas treated with single-fraction Gamma Knife radiosurgery (GKRS) with a collision. We introduce a novel mask fixation method to avoid a collision.
MATERIALS AND METHODS
This study protocol was reviewed and approved by the Institutional Review Board (IRB). The IRB waived off the requirement for informed consent due to the retrospective nature of the study. Identifying details (name, birth date, and other information) were not included in this study. This study was conducted ethically in accordance with the World Medical Association Declaration of Helsinki.
Patient population
A 76-year-old man visited our institute in February 2022 because of an incidentally discovered brain tumor. The patient showed dizziness and hearing loss. Initial magnetic resonance imaging (MRI) revealed two meningiomas in the right frontal convexity and right frontal falx. We planned to perform GKRS for the two lesions with mask fixation.
GKRS treatment
The patient underwent planning MRI scans using a 1.5 tesla MR system (Philips Achieva, Best, Netherlands) with a single-channel sense head coil MRI. We obtained T1-weighted, T1-weighted with gadolinium enhancement, and T2-weighted images. The patient was placed on the couch and their head was fixed using the head cushion (MOLDCARE RI II; ALCARE, Tokyo, Japan) and the Nanor® Mask (Elekta Instrument AB, Stockholm, Sweden). The planning CBCT scan of 6.3 mGy was performed while the head was immobilized. The planning CBCT was co-registered with the planning MRI using the Leksell GammaPlan (LGP). Once CBCT-MRI co-registration was complete, the dose distribution was recalculated to adapt to the new coordinate system. Dosimetry planning was performed by neurosurgeons (Y.G.K. and Y.S.D.) and medical physicists (H.C.M. and B.J.M.).
Head cushion adjustment
The LGP indicates the possibility of a collision, which occurs when the distance between the mask and collimator helmet is less than a preset level. The LGP showed unreachable position for both shots in one (at the right frontal falx) of the two lesions in the patient in Fig. 1. The distance was approximately 175 mm from the lesion top to the bottom of a head on the axial T1-weighted image with gadolinium enhancement. The mask had already hardened; therefore, new mask fixation adjustment was devised as follows : 1) before spraying the head cushion, the corner of the cushion was cut to drain the polystyrene beads. The beads were drained to approximately 5 cm in diameter (Fig. 2B). 2) The corner was sutured with a stapler; 3) the head cushion was sprayed with water; 4) the head cushion was fixed to the head support as thin as possible. And 5) the mask was placed on the patient’s face. The details of this method are shown in Fig. 2.
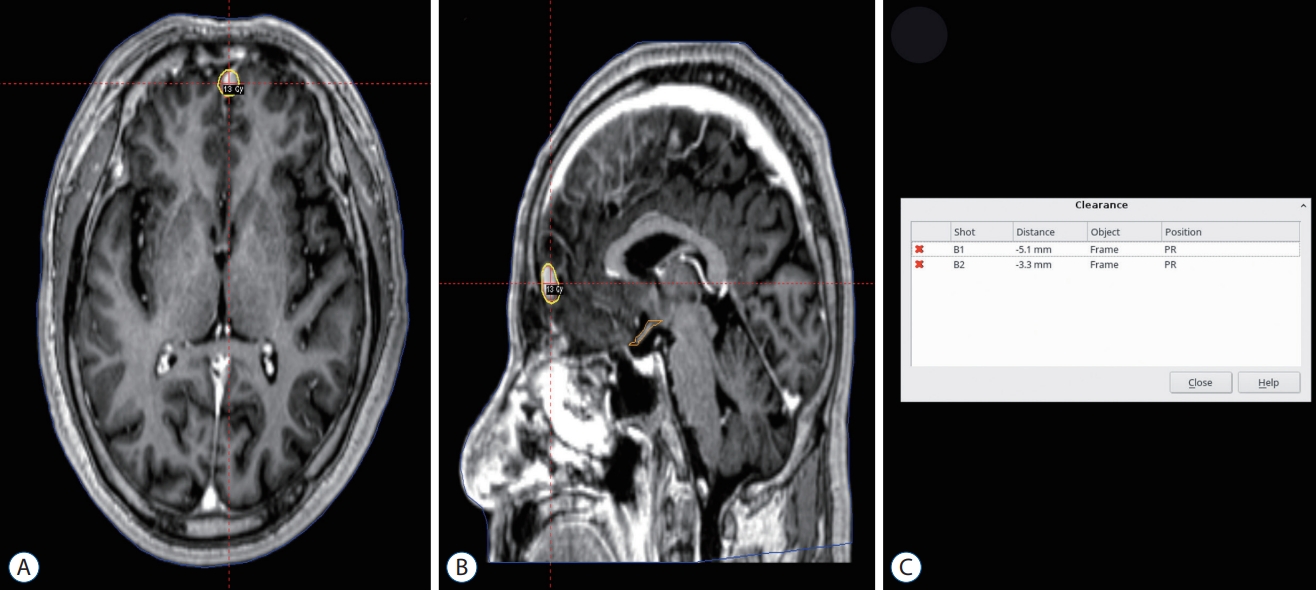
The Leksell GammaPlan showed the unreachable position for both shots in the right frontal falx. The yellow circle indicates the treatment dose of 13 Gy shot isocenter (50% isodose). Snapshot view of gamma knife dose planning on the axial plane (A), sagittal plane (B), and clearance (C).
Evaluation of clearance-warning coordinates
To confirm the appropriate mask placement to the target in the right frontal falx lesion, we investigated the differences in the coordinates of shots and clearance distance using LGP. The difference in shot coordinates is defined as follows [9] : ∆x = x-axis coordinate in initial planning CBCT – x-axis coordinate in planning CBCT after adjusting the head cushion; ∆y = y-axis coordinate in initial planning CBCT – y-axis coordinate in planning CBCT after adjusting the head cushion; ∆z = z-axis coordinate in initial planning CBCT – z-axis coordinate in planning CBCT after adjusting head cushion. Furthermore, the 3D error (∆r) is defined as the localization error using the following formula : ∆r = v(∆x2 + ∆y2 + ∆z2).
RESULTS
Execute GKRS with a modified mask fixation
A modified mask fixation was successfully performed, and GKRS was performed without a collision. A collision was resolved by removing approximately 50 mL of beads from the head cushion. The depth of the head cushion was also measured. The vertical depth of the initial head cushion was approximately 4 cm and that of the modified head cushion was approximately 4.8 cm. A comparison of the vertical depths is shown in Fig. 3.
Coordinates comparison
The coordinates of the shots were compared for the initial and modified mask fixations. The difference in the x, y, and z-axis coordinates was approximately ±0.2 mm, +10.5 mm, and -14 mm, respectively. The difference in the 3D error was approximately 18 mm. The data are presented in Table 1.
Clearance distance comparison
The clearance distances of the shots were compared for the initial and modified mask fixations. For both shots (shot1, shot2), the difference in clearance distance was -10.2 mm.
DISCUSSION
In this case study, we recommend a modified mask fixation method to avoid a collision. The mask fixation method has been used for noninvasive head immobilization in neurosurgery [12]. Mask fixation has a similar outcome and toxicity to the frame fixation [6]. If collisions do not occur under mask fixation, it can be used for GKRS. Whenever the distance between the frame/post/screw/mask and collimator helmet is less than a preset level, LGP informs the possibility of a collision by a collision warning. Frame fixation occasionally requires shifting in anticipation of potential collisions. Unlike frame fixation, mask fixation can only be employed by adjusting the head cushion. For proposed mask fixation method, removing polystyrene beads from the head cushion and mask fixation is recommended.
Complications of GKRS have been reported in the form of pin site infections, scarring, numbness, and pain [14]. Mask fixation is a noninvasive method that requires no local anesthesia, skin incision, or skull depression. Moreover, mask fixation can be safely used in cases where it is difficult to fix the frame in patients that are younger than 2 years old and children who have undergone craniotomy [15]. Because there are no frame complications during mask fixation, psychological stress is reduced by determining the patient positioning without a collision. Conversely, it can also be used for children with small heads by raising their head cushion.
Despite the many benefits of mask fixation in GKRS, recent studies have suggested that mask-based immobilization may be related to increased motion errors during treatment [3,10], which may lower accuracy compared to frame fixation. Carminucci et al. [3] suggested that variability in motion error associated with mask fixation must be considered when planning for small lesions or eloquent areas. Treatment accuracy is related to the immobilization of patients in stereotactic space. Frame fixation has been consistently shown to maintain submillimeter accuracy during treatments [8,13,14]. With careful frame fixation, the GKRS can reach almost any part of the brain. If the lesions are located in the periphery of the brain, it is important to pay attention to the frame placement to avoid collisions. Nakazawa et al. [11] reported that the clearance map was helpful in simulating appropriate skull frame placement without a collision. The clearance map is created in the form of a curve according to the x, y, and z coordinates [11]. In our case, we confirmed that the minimum distance without a collision warning was approximately over 155 mm (lateral) to 165 mm (midline) on the T1-weighted image with gadolinium enhancement. If the minimum distance from the target to the bottom (or top, in case of target is located at the occipital area) of a head on the axial MR image is over 155 mm considering the laterality of the lesion, it is recommended to consider the possibility of removing beads. This will allow the beads to be removed prior to head cushion hardening and prevent further wasting of the head cushion. A more suitable distance value may be confirmed through further studies.
The outcome of our study shows that a collision can be resolved without any complications using the modified mask fixation method in a simple manner. A collision can be avoided because there was an allowance of approximately 10 mm along the y-axis. In our study, removing the material from the head cushion and mask fixation did not seem to affect the immobilization status when the HDMM values were monitored. The head cushion could be replaced with other materials, but the materials should play a role in restraining the movement of the patient. Although no study has been conducted, mask fixation without a head cushion should be carefully considered because it is very difficult to fix. If a collision occurs, even with our proposed modified mask fixation, it would be better to use frame fixation.
This study has several limitations. This method was performed in only one case and was analyzed retrospectively. The clearance distance within -5.1 mm can resolve a collision by removing the beads. However, if the clearance distance over -5.1 mm or more occurs, it is necessary to confirm how many beads can be removed without a collision while maintaining the function of the head cushion in future studies.
CONCLUSION
In conclusion, we recommend a modified mask fixation method for a collision. We find that a collision could be avoided by increasing the vertical depth of the head cushion.
Notes
Conflicts of interest
The authors report no conflicts of interest related to this work.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : HCM, DL; Data curation : HCM, DL, YSD; Formal analysis : HCM, DL, BJM; Funding acquisition : YSD; Methodology : HCM, DL, YGK; Project administration : YSD; Visualization : HCM, YSD; Writing - original draft : HCM, DL; Writing - review & editing : YSD
Data sharing
None
Preprint
None
Acknowledgements
This research was supported by Chungbuk National University Korea National University Development Project (2022).