Combined Open Door Laminoplasty with Unilateral Screw Fixation for Unstable Multi-Level Cervical Stenosis : A Preliminary Report
Article information
Abstract
Objective
The authors reviewed their experiences of combined surgery (open door laminoplasty with unilateral screw fixation) for unstable multi-level cervical stenosis, to clarify the situation regarding the surgical approach most appropriate for the treatment of diffuse unstable multi-level cervical stenosis.
Methods
From January 2011 to January 2012, combined surgery was performed for unstable multi-level cervical stenosis by one surgeon at our institution. The subjects of this study were 6 men of mean age 53.7 years (range, 48-71) with a mean follow-up of 9.3 (range, 3-14) months. All imaging studies showed severe multi-level cervical stenosis with spinal cord signal change, and instability or kyphotic deformity. A retrospective review of clinical, radiological, and surgical data was conducted.
Results
Average laminoplasty level was 4.8 and the average screw fixation level was 5.0. Japanese Orthopedic Association score improved from an average of 5.2 to 11.2 points. According to Nurick's grades and Odom's criteria, symptom improvement was statistically significant. On the other hand, Cobb's angle changes were not significant. Average operation time was 5.86 hours with an average blood loss of 460 mL. No significant surgical complication was encountered.
Conclusion
Despite the small cohort and the short follow-up duration, the present study demonstrates that laminoplasty with unilateral screw fixation is a safe and effective treatment for unstable multi-level cervical stenosis.
INTRODUCTION
Multi-level (more than 3 levels) cervical canal stenosis caused by the ossification of posterior longitudinal ligament (OPLL) or degenerative disc disease is not uncommon2). Most patients are asymptomatic, but those with severe spinal cord compression are predisposed to symptoms of cervical radiculopathy or myelopathy14). Surgical treatment is recommended when neurologic symptoms are severe, and the surgical techniques used can be classified as either anterior or posterior.
Posterior approaches, such as, total laminectomy, total laminectomy with screw fixation, and laminoplasty are most commonly used to treat diffuse multi-level cervical stenosis8,16,24,25). However, the appropriate surgical approach for treating diffuse multi-level cervical stenosis, especially with cervical instability or kyphosis, remains controversial, because available surgical techniques have unique advantages and disadvantages.
Recently, combined open door laminoplasty with unilateral screw fixation has been performed in patients with unstable multi-level cervical stenosis because it is considered to provide firm stabilization with fewer complications. Here, we provide a review of our experiences of combined open door laminoplasty with unilateral screw fixation from the clinical, radiological, and surgical perspectives.
MATERIALS AND METHODS
Indication
From January 2011 to January 2012, six patients with diffuse multi-level cervical stenosis underwent combined surgery at our institution.
The indications for combined surgery were as follow. 1) Diffuse multi-level cervical canal stenosis due to OPLL, a herniated disc, or spondylosis refractory to conservative treatment. 2)Signal change of the cervical spinal cord by cervical magnetic resonance imaging (MRI) suggesting spinal cord injury. 3) Apparent preoperative kyphotic deformity, involvement of C2 or C7 during surgery, or cervical spine instability, including spondylolisthesis (anterior-posterior translation >3.5 mm), angulation (>11°), anterior longitudinal ligament (ALL) injury, or posterior ligament injury.
Procedure
A posterior midline approach was used and subperiosteal dissection was performed with the patient prone, the neck in the neutral position, and the head immobilized by a 3-pin Mayfield skull clamp.
Before laminoplasty, we decided on the open and hinged sides based on the severities of symptoms and stenosis by MRI. The more severe side was taken as the open side to enable appropriate foraminotomy.
The first procedure performed was posterior expansive open door laminoplasty using the Hyrabayashi technique7) with titanium miniplates. This technique requires a pneumatic high-speed burr to create a gutter at the junction of the lamina and medial aspect of the lateral mass through outer cancellous bone. The hinged side was thinned without a complete cut. The ligamentum flavum above the cephalic level and below the caudal level of the en bloc were cut with Kerrison rongeurs to facilitate opening the lamina.
Before opening the laminar door, a drill hole penetrating the cortex of the lateral mass was created at each level for screw insertion. The direction of the lateral mass screw was 20 to 30 degrees laterally and parallel to the adjacent facet, starting 1 mm medial to the exact center of the lateral mass (Magerl's technique11)). At C2 or C7, we adopted the transpedicular screw insertion technique. The depth of the drill hole was measured, and then a small (3.5 mm diameter) Vertex screw® (Medtronic Sofamor Danek, Memphis, TN, USA) of proper length was selected and inserted.
"Greenstick osteotomy" was performed by carefully displacing the spinous processes toward the closing osteotomy side and elevating the opening side of the lamina with a nerve hook. Each level was then stabilized using a Centerpiece® (Medtronic Sofamor Danek, Memphis, TN, USA).
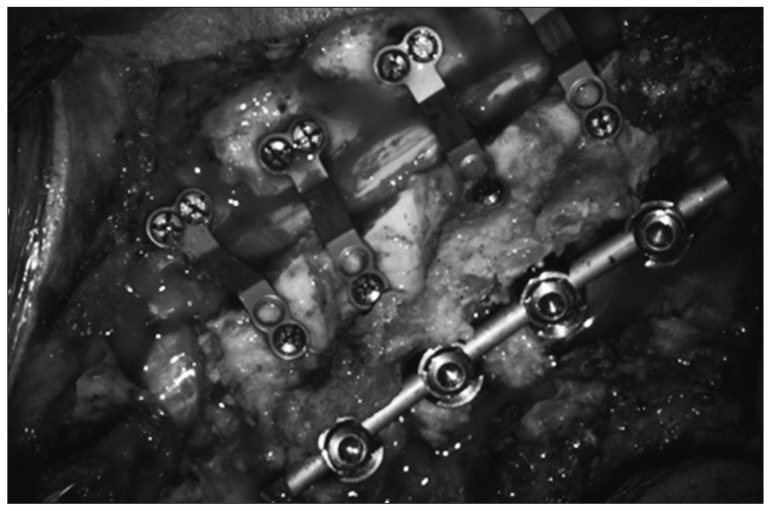
Finally, the rod was contoured to the sagittal contour desired and passed through all screw heads. Locking nuts were then inserted to fix the rod to the screws. Compression or distraction was applied to gain further correction (Fig. 1). A mixture of bone chips collected during pervious decompression and allograft bone chips were applied to the gutter of the hinged side to facilitate bone fusion.
Outcome parameters
Clinical outcomes were assessed using the Japanese Orthopedic Association (JOA) scoring system, Nurick's grades, and Odom's criteria. Cervical MRI, cervical computed tomography (CT), and dynamic radiography were performed prior to surgery and cervical CT immediately after surgery. In addition, dynamic radiography was performed at each follow-up visit. Cobb's angle was used to evaluate lordosis of the cervical spine using lateral X-rays in a neutral position preoperatively and last follow-up visits (Fig. 2).
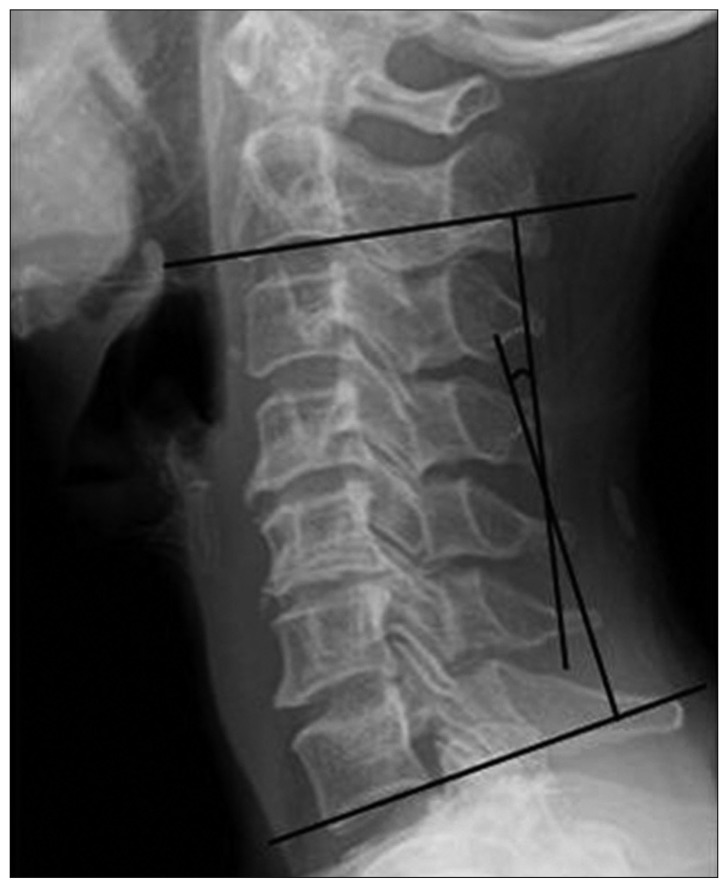
Cobb's method for measuring cervical lordosis. Cervical lordotic angles are measured by joining perpendiculars to lines drawn parallel to the inferior end plates of C2 and C7. When the C7 vertebra was not well visualized on lateral film, the inferior plate of C6 was used.
Surgical outcomes were evaluated using estimated blood losses (EBL), operation times, durations of postoperative bed rest, and surgical complications, such as, neurologic deterioration and wound infection.
Wilcoxon's rank sum test in SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used for the analysis, and statistical significance was accepted for p values of <0.05.
RESULTS
Demographics
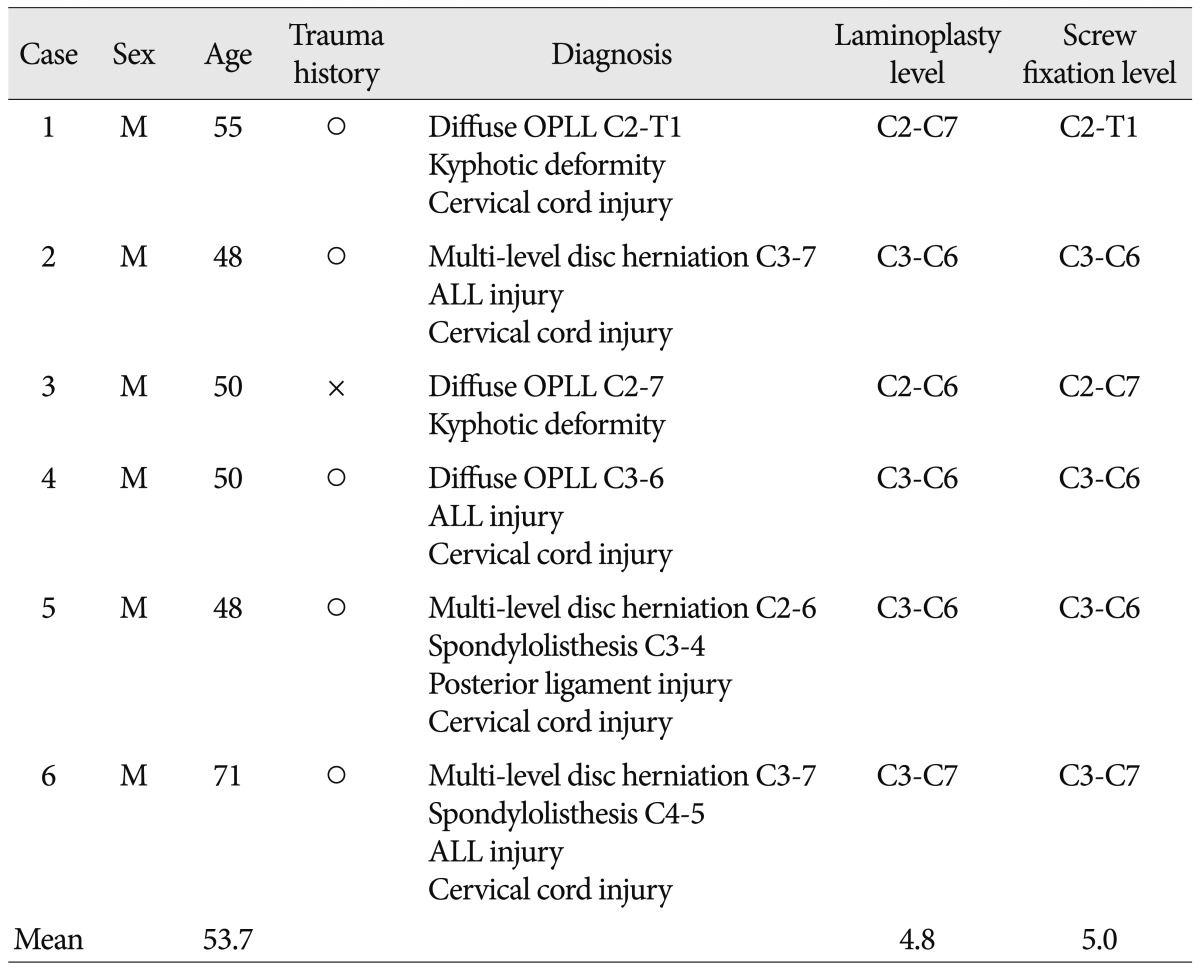
All patients were male, and average patient age was 53.7 years (range, 48-71). Average symptom duration was 18.3 days (range, 5-30), and average follow-up period after surgery was 9.3 months (range, 3-14). The mean laminoplasty level was 4.8 (range, 4-7) and the mean screw fixation level was 5.0 (range, 4-7).
Five of the six patients had of trauma history. In three of these patients with a trauma history, imaging showed cervical instability and multi-level disc herniation with cord injury. In another, imaging showed multi-level OPLL with kyphotic deformity, and in the remaining patient, imaging showed multi-level OPLL with ALL injury. In the patient without a trauma history, cervical MRI showed multi-level OPLL with kyphotic deformity and spinal cord signal change (Table 1).
Clinical outcomes
The mean preoperative JOA score was 5.2 (range, 3-8), and this increased to 9.0 (range, 5-12) at 1-month and to 11.2 (range, 8-14) at final follow-up (Fig. 3). Nurick's grade also improved from 4.5 (range, 3-5) preoperatively to 3.0 (range, 2-4) at 1-month and 1.8 (range, 0-3) at final follow-up (Fig. 4). JOA score and Nurick's grade improved in all patients after surgery with statistical significance and these improvements were maintained during follow-up (p<0.05).

Graph showing JOA scores before surgery and during follow-up. JOA scores recovered by a mean of 6.0 points (from 5.2 to 11.2; p<0.05) at last follow-up. f/u : follow-up, JOA : Japanese Orthopedic Association, pre-op : pre-operation.

Graph showing Nurick's grades before surgery and during follow-up. Nurick' s grade recovered by a mean of 2.3 (from 4.5 to 1.8; p<0.05) at last follow-up. f/u : follow-up, pre-op : pre-operation.
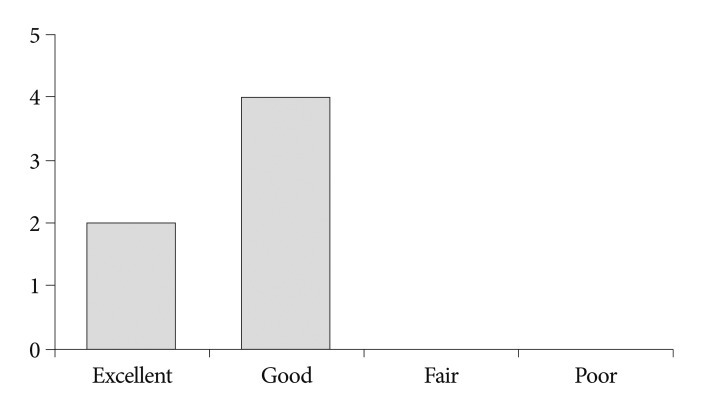
According to Odom's criteria, results were excellent in 2 (33.3%) and good in 4 (66.7%) at last follow-up (Fig. 5).
Radiological outcomes
MRI signal changes in the cervical spinal cord were observed in all patients, and two patients showed kyphotic deformity. Mean Cobb's angle increased from 6.5° (range, -10.6-23.3) preoperatively to 13.2° (range, -10.5-33.4) at last follow-up, but this improvement was not statistically significant (Fig. 4).
No patient showed postoperative kyphotic change, cervical instability, instrument breakdown, or fusion failure during follow-up (Fig. 6, 7, 8).
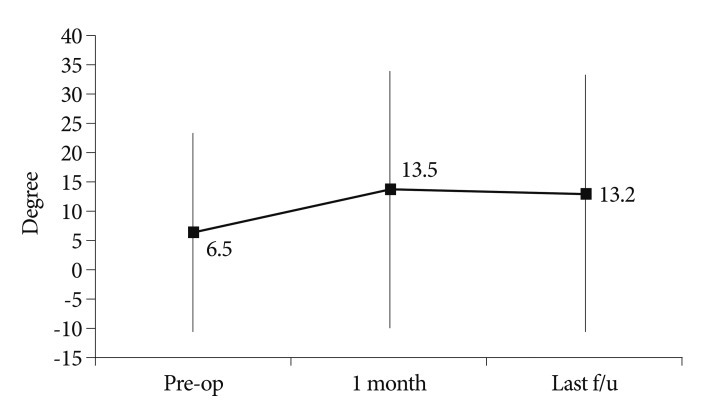
Graph showing Cobb's angle before surgery and during follow-up. The improvements observed at last follow-up visits were not significant. f/u : follow-up, pre-op : pre-operation.

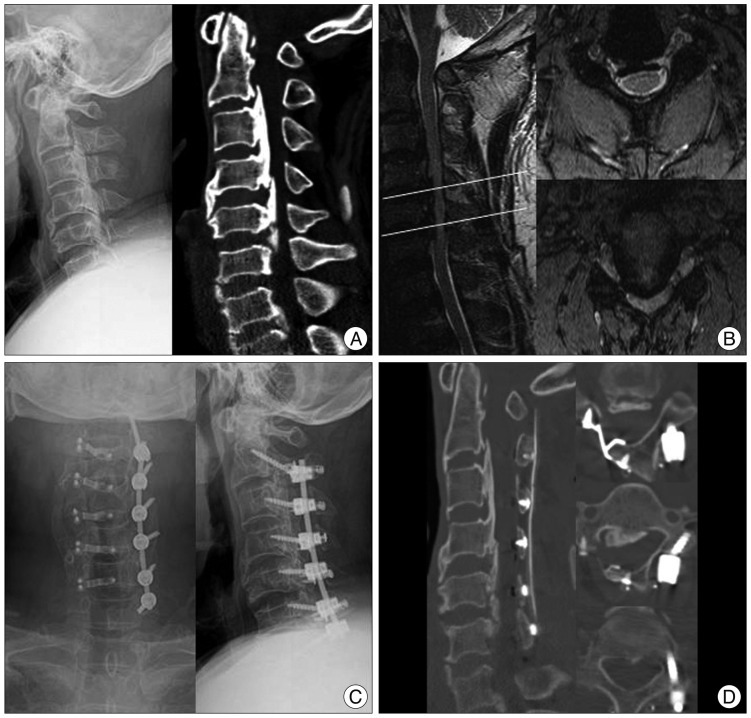
A 71-year-old man presented with quadriparesis after a slip down. A : Preoperative cervical radiography and CT showed cervical degenerative spondylosis with loss of cervical lordosis and a teardrop fracture of the C4 body with spondylolisthesis at C4-C5 and C5-C6. B : Preoperative cervical MRI demonstrated severe spinal cord compression at C3-C6 with high signal change in T2-weighted images. We suspected an ALL injury based on the signal change observed in pre-vertebral soft tissue. C : Left side open door laminoplasty at C3-C7 with lateral mass screw fixation at C3-C6 and transpedicular screw fixation at C7 were performed. D : Postoperative cervical CT showed an efficiently expanded spinal canal and corrected cervical alignment. ALL : anterior longitudinal ligament, CT : computed tomography, MRI : magnetic resonance image.
A 50-year-old man presented with a radiating pain in both arms and progressive gait disturbance. A : Preoperative cervical radiography and CT revealed degenerative spondylosis, loss of lordosis, and diffuse OPLL at C2-C6. B : Preoperative cervical MRI revealed severe spinal cord compression at C2-C6 with high signal change on T2 weighted images. C : Right side open door laminoplasty at C2-C6 with lateral mass screw fixation at C3-C6 and transpedicular screw fixation at C2 and C7 were performed. D : Postoperative cervical CT showed an efficiently expanded spinal canal and appropriately inserted screws. OPLL : ossification of posterior longitudinal ligament, CT : computed tomography, MRI : magnetic resonance image.
Surgical outcomes
Mean operation time was 5.86 hours (range, 4.5-6.5), mean EBL was 460 mL (range, 300-500), mean transfusion amount was 0.8 packs (range, 0-1), and mean bed rest duration was 2.0 days (range, 1-5). No major surgical complication, such as, aggravation of neurological symptoms by cord injury, C5 nerve palsy, cerebrospinal fluid leakage, or wound infection was encountered. Furthermore, there was no perioperative morbidity related to general anesthesia, such as, a cardiopulmonary problem or deep vein thrombosis.
DISCUSSION
Controversy exists regarding the appropriate surgical method for treating multi-level cervical stenosis due to cervical OPLL, a herniated disc, or spondylosis. Theoretically, an anterior approach is optimal for direct lesion removal. However, in cases of multi-level stenosis involving more than 3 levels, an anterior approach is unsatisfactory because of high rates of complications, such as, graft extrusion, subsidence, fracture, pseudoarthrosis, and failure of fusion27). Furthermore, the anterior approach in multi-level stenosis may require longer surgical times, and cause injury to the recurrent laryngeal nerve, esophagus, or great vessels due to prolonged traction28). In addition, removal of high-level lesions, such as, at lesions at C2 or C3, is technically difficult using an anterior approach19).
Thus, in multi-level cervical stenosis, a posterior approach is preferred4,7,20). This approach includes total laminectomy, laminectomy with fusion, laminoplasty, or combined anterior and posterior surgery. The selection of an appropriate approach depends on numerous factors, including cervical alignment and contour, patient's symptoms and metabolic factors, and the surgeon's experience with various surgical techniques. The most important factors in patient selection for a particular procedure are clinical symptoms, and radiographic alignment of the spine21,33).
Total laminectomy has been widely used for complete decompression of cervical canal stenosis29). However, after total laminectomy, a buckling-type alignment or kyphotic deformity may occur because of destruction of the posterior structure, which can cause delayed neurological deterioration due to impingement of the spinal cord at the apex of the cervical curvature8,22,24,25).
Generally, posterior cervical screw fixation may be necessary to avoid the development of a kyphotic deformity after laminectomy alone. The main goal of laminectomy with fusion is to provide efficient decompression of the spinal cord and to maintain stability simultaneously. Furthermore, this technique is useful for the treatment of multi-level stenosis with straightened cervical spines or with cervical instability16). However, aggravation of neurologic symptoms due to the formation of a posterior scar band or C5 nerve root palsy may occur after this procedure1,9).
Nowdays, laminoplasty is the usual treatment of choice for multi-level cervical stenosis8,16,25). The main goal of laminoplasty is to provide multi-level decompression of the spinal cord by widening the spinal canal, while preventing scar in-growth and preserving range of motion5,15,30).
Many laminoplasty techniques including open door, French door, and Z-plasty have been described7,8,12,22,31). Some authors have reported the decompressive effect of laminoplasty is no different to that of laminectomy, and concluded that post-laminoplasty cervical stability is superior to that after laminectomy6,18,29).
However, laminoplasty may not provide spinal stability or correct alignment of the cervical spine. When preoperative instability is encountered, such as, traumatic spondylolisthesis, segmental instability, or ligament injury, laminoplasty alone is insufficient to achieve stability or to correct alignment. Furthermore, kyphotic changes are observed in some cases, such as, the presence of preoperative cervical straightening or kyphosis, or the involvement of C2 or C7 during operation3,13,32). Some authors have reported that 8-30% of patients developed progressive kyphosis over a period of 10 years after laminoplasty8,13,24). Postoperative spinal instability or kyphosis can cause progressive radiculomyelopathy, C5 nerve root palsy, limitation of motion, and neck pain, and thus, this procedure may be insufficient to treat multi-level stenosis in such cases10,23,33).
Previously, to reinforce cervical stability, laminoplasty was combined with other procedures, such as, with anterior fusion or on-lay allografted or autografted bone in the lateral grooves2,17,26). However, immediate stability cannot be achieved when an on-lay bone graft in the lateral grooves, and for anterior fusion, additional surgery and prolonged operation times are a burden to patients.
We used additional screw fixation to reinforce stability or to correct alignment during laminoplasty. This combined surgical technique allows immediate internal fixation enabling early ambulation and subsequent long-term stabilization by bony fusion. In addition, this single-stage surgery may facilitate additional anterior fusion surgery for the maintenance of stability. Furthermore, as compared to laminectomy with fusion, this combined surgery has the advantage of preventing postoperative scar formation.
As mentioned above, for simultaneous decompression and stabilization, this single-stage combined open door laminoplasty with unilateral screw fixation is indicated in selected patients with multi-level cervical stenosis associated with preoperative kyphosis, C2 or C7 involvement during laminoplasty, and cervical instability (e.g., spondylolisthesis, segmental angulation, or a ligamentous structure injury).
In the present study, with regard to clinical outcomes, changes in JOA scores, Nurick's grades, and patient satisfaction according to Odom's criteria were all favorable. Furthermore, although without statistical significance, cervical lordosis was improved. This means that the correction of malalignment was favorable after surgery. In addition, no patient developed kyphotic change, instability, or fusion failure during follow-up.
Operation time and blood loss were slightly greater for combined surgery than for laminoplasty alone. However, we believe these increases are acceptable because both procedures were performed in a single-stage and no serious postoperative complication related to operation time or blood loss was encountered.
Despite our findings, this study has several limitations. In particular, the number of patients was small and the follow-up period was too short to allow generalizations of results. Additional study is required to compare laminectomy plus fusion or laminoplasty alone with this combined surgical technique in cases with identical operative indications.
CONCLUSION
Despite a small cohort and a short follow-up, the present study demonstrates that combined surgery is both safe and effective for treating unstable multi-level cervical stenosis. We suggest that single-stage combined open door laminoplasty with unilateral screw fixation be considered in selected patients with multi-level cervical stenosis associated with preoperative kyphosis, involvement of C2 or C7, or cervical instability.