Chondrosarcoma Apoplexy in Thoracic Spine
Article information
Abstract
Chondrosarcoma is a very uncommon malignant primary bone tumor, especially, it occurs extremely rare in the spine. A 52-year-old man was admitted to the emergency room with sudden paraplegia. Twelve hours prior to a paraplegic event, he visited an outpatient clinic with discomfort and tenderness around the medial border of the right scapular, and his neurologic status was absolutely intact. Magnetic resonance imaging showed a lobulated soft tissue mass from T3 to T5, which extended to the epidural space. Computed tomography scans showed soft tissue mass on the spinal posterior arch and osteolytic change of the adjacent bony structures. Emergent surgery was performed and the lesion was removed. Dark reddish blood and gel-like material were encountered around the dura and posterior arch during the operation. Multiple pulmonary nodules were found on a chest CT scan and a biopsy of one of them had been proven to be a metastasis of chondrosarcoma. The histologic examination showed dedifferentiated chondrosarcoma. The patient's neurologic deficit was improved slowly from ASIA A to ASIA D. Chondrosarcoma in the spine is extremely rare, even more with acute hemorrhage and sudden expansion into the epidural space. We named it chondrosarcoma apoplexy. We should consider the possibility of a hemorrhagic event when the patient's neurologic deficit worsens suddenly with spinal bone tumor.
INTRODUCTION
Spinal chondrosarcoma is an extremely rare malignant tumor, characterized by cartilage-forming9). Chondrosarcomas compose 7% to 12% of all primary spine tumors and one forth of primary malignant spine tumors2). In the spine, the common site of chondrosarcoma is the thoracic spine, followed by lumbar and cervical spine3). Growth pattern of chondrosarcoma is usually indolent, and the most common presenting symptom is focal pain6,15). There is no previous reported case of spinal chondrosarcoma, which is presented with sudden progressive paraplegia, due to acute hemorrhage and exophytic expansion into the epidural space. We named it chondrosarcoma apoplexy because it is a similar condition with that of the pituitary apoplexy, which causes neurological problems, such as visual loss.
CASE REPORT
A 52-year-old man was admitted to the emergency room with sudden paraplegia. Twelve hours prior to such paraplegic event, he visited an outpatient clinic. At that time, he just complained of discomfort and tenderness around the medial border of the right scapular, and his neurologic statue was absolutely intact. He had no special past medical history. As such, he wanted to make another visit later when he would develop aggravated pain. There was no evidence of increased uptake on the PET-CT scan that he has checked two years ago. Magnetic resonance imaging (MRI) checked at the emergency room showed a lobulated soft tissue mass from T3 to T5, which extended to the epidural space (Fig. 1). Computed tomography scans showed soft tissue mass on the spinal posterior arch and osteolytic change of the adjacent bony structures (Fig. 2). Emergent surgery was performed, and the lesion was removed. Dark reddish blood and gel-like material were encountered around the dura and posterior arch during the operation. The histologic examination showed findings conformed to dedifferentiated chondrosarcoma (Fig. 3). The results of immunohistochemical stains for the high grade spindle cells were focal (+) for smooth muscle actin antibody, but (-) for desmin, cytokeratin, CD34 and S-100 protein. Multiple pulmonary nodules were found on chest CT scan, and biopsy of one of them had proven to be a metastasis of chondrosarcoma. The patient's neurologic deficit was improved slowly from ASIA A to ASIA D.
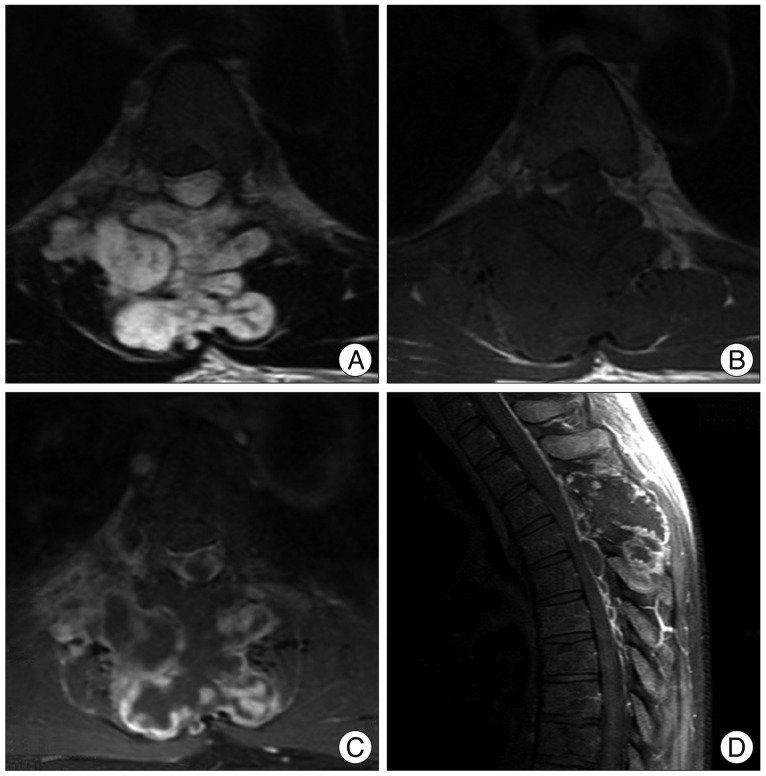
MR imagings show a lobulated soft tissue mass from T3 to T5 which extended to the epidural space. There are destructive changes around adjacent bony structures by this mass (A : T2 weighted image, B : T1 weighted image, C and D : Gd-enhanced image).

Computed tomography scans show soft tissue mass on the spinal posterior arch and osteolytic change of the adjacent bony structures.
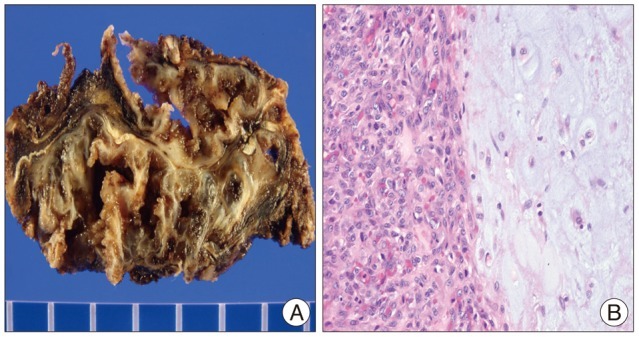
A : Gross finding. The resected specimen shows lobulated grayish-white cartilaginous mass with myxoid and cystic change. B : Microscopic finding. The tumor shows bimorphic pattern consisting of low grade chondrosarcoma (on the right) juxataposed of high-grade spindle cell sarcoma (on the left) (hematoxylin eosin stain, ×200).
DISCUSSION
Spinal chondrosarcomas are uncommon disorders, characterized by malignant cartilage-forming and most commonly arise in the thoracic region3,9,10). Chondrosarcomas compose 7% to 12% of all primary spinal bone tumors and one forth of primary malignant spine tumors2). Affected ages are usually forth to sixth decades2). The male to female gender ratio is up to 4 : 12,10). Growth pattern of chondrosarcomas is usually indolent. Although the most common presenting symptom is focal pain, neurologic deficits are also common3,8,10,15). Plain radiography, CT scan and MRI are useful to assess the location and characteristics of the tumor. CT scan typically demonstrates a lytic, destructive lesion of various densities, with or without focal bony expansion6,13). CT findings are various with the type of chondrosarcomas8). Cortical thickening with extension to the soft tissue can be seen in peripheral chondrosarcoma, a round lytic lesion with surrounding sclerosis is observed in a clear cell chondrosarcoma4). Dedifferentiated and mesenchymal types may demonstrate local bony destruction1,14). The most common MRI patterns are low signal intensity with T1 and high signal intensity lesion with T2 weighted images, peripheral or heterogeneous enhancement with gadolinium6). Histologically, chondrosarcomas are defined as mesenchymal, non-meningothelial tumors. Chondrosarcomas are classified into several subtypes, which include the conventional, clear cell, mesenchymal and dedifferentiated types6,8,9,11). According to the pathology, conventional chondrosarcomas are mostly benign and dedifferentiated chondrosarcomas are aggressive and frequently metastasize to other sites12). Chondromas and other sarcomas, including osteosarcoma, leiomyosarcoma, and rhabdomyosarcoma, should be considered as differential diagnosis3). The goal of the treatment is to excise the lesion as completely as possible15). Although these tumors are resistant to adjuvant chemotherapy and radiotherapy, hypofractionated stereotactic radiation therapy may be useful for tumor recurrence and palliation5-7,11).
In our case, the mass was located mainly in the posterior arch of T3 and T4, T5 and extended to the epidural space. It was composed of multi-lobulated mass, combined with hemorrhage. There is no previous reported case of spinal chondrosarcoma that is presented with sudden progressive paraplegia, due to acute hemorrhage and exophytic expansion into the epidural space. We named it chondrosarcoma apoplexy because it is a similar condition with pituitary apoplexy that causes acute visual loss.
CONCLUSION
Chondrosarcoma is an uncommon disorder that rarely involves the spine and previously has never been associated with sudden paraplegia with acute hemorrhage and expansion into the epidural space. When radiologic studies show a lobulated mass with extension into the surrounding tissue and osteolytic change, chondrosarcoma should be included in the differential diagnosis of primary spinal bone tumor, although its occurrence at this site is extremely rare. Furthermore, we should realize the possibility of hemorrhage and sudden expansion when the patient's neurologic deficit developed suddenly.