Short Segment Fixation for Thoracolumbar Burst Fracture Accompanying Osteopenia : A Comparative Study
Article information
Abstract
Objective
The purpose of this study was to compare the results of three types of short segment screw fixation for thoracolumbar burst fracture accompanying osteopenia.
Methods
The records of 70 patients who underwent short segment screw fixation for a thoracolumbar burst fracture accompanying osteopenia (-2.5< mean T score by bone mineral densitometry <-1.0) from January 2005 to January 2008 were reviewed. Patients were divided into three groups based on whether or not bone fusion and bone cement augmentation procedure 1) Group I (n=26) : short segment fixation with posterolateral bone fusion; 2) Group II (n=23) : bone cement augmented short segment fixation with posterolateral bone fusion; 3) Group III (n=21) : bone cement augmented, short segment percutaneous screw fixation without bone fusion. Clinical outcomes were assessed using a visual analogue scale and modified MacNab's criteria. Radiological findings, including kyphotic angle and vertebral height, and procedure-related complications, such as screw loosening or pull-out, were analyzed.
Results
No significant difference in radiographic or clinical outcomes was noted between patients managed using the three different techniques at last follow up. However, Group I showed more correction loss of kyphotic deformities and vertebral height loss at final follow-up, and Group I had higher screw loosening and implant failure rates than Group II or III.
Conclusion
Bone cement augmented procedure can be an efficient and safe surgical techniques in terms of achieving better outcomes with minimal complications for thoracolumbar burst fracture accompanying osteopenia.
INTRODUCTION
The goals of surgical treatment for thoracolumbar burst fractures are to restore vertebral column stability and to decompress neural elements4). Due to several problems associated with extensive long-level instrumentation, posterior short-segment instrumentation has been recently preferred for the treatment of thoracolumbar burst fractures in cases mild communition or load sharing score5). Because, a fracture with mild communition or load sharing score indicates adequate sharing of load through the injured vertebral body itself along with the implant to permit short segment instrumentation and fusion5). Short-segment instrumentation (that is, pedicle screw instrumentation at the fracture level and the levels above and below) is being selected among warrant surgical interventions. Pedicle screw insertion makes it possible to maintain vertebral column stability until the desired alignment is achieved, and simultaneously restores canal dimensions and vertebral body height6). Furthermore, it has been assumed to facilitate early painless mobilization by providing substantial stabilization of the fractured vertebra. Some authors have hypothesized that bone grafting may be unnecessary in combination with short-segment fixation for the treatment of thoracolumbar burst fractures8). Moreover, recent reports have demonstrated the efficacy of vertebral augmentation procedures in terms of preventing implant failure in osteoporotic patients1). In addition, to minimize the negative consequences of traditional open surgery, such as, muscular denervation and atrophy, screw fixation via percuaneous technique has been proposed and applied. We conducted this study to compare and evaluate the efficacies of bone cement augmentation and bone fusion procedure for the treatment of thoracolumbar burst fractures accompanying osteopenia.
MATERIALS AND METHODS
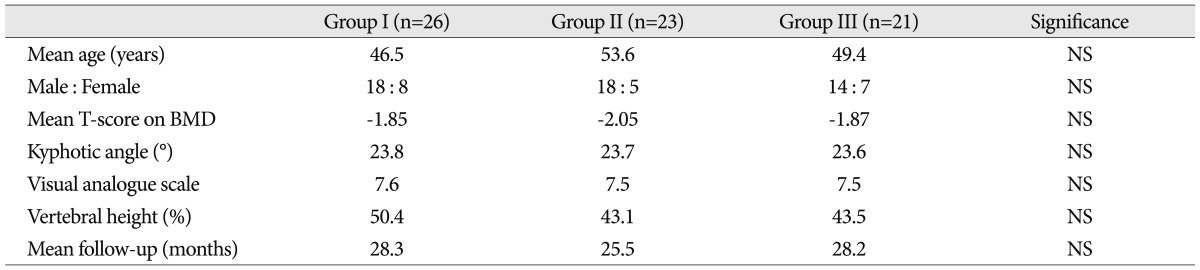
This retrospective study included 70 patients (47 males and 23 females) with thoracolumbar burst fractures with osteopenia treated at our institute from January 2005 to January 2008. All patients sustained a thoracolumbar burst fracture (T10-L2). Study inclusion criteria limited enrollment to single level thoracolumbar burst fractures with; 1) a neurologically intact status, despite severe canal encroachment, 2) patients with osteopenia (-2.5< mean T-score by bone mineral densitometry <-1.0), 3) a loss of anterior body height exceeding 40% or more than 30° of sagittal angulation, and 4) intact bilateral pedicles, enabling screw insertion at the fractured vertebra. The exclusion criteria were major neurological deficits that required open decompression due to severe canal compromise and an accompanying pedicle fracture preventing screw insertion at the fracture level. The 70 patients were divided into three groups by operation technique : 1) Group I (n=26) : short segment fixation with posterolateral bone fusion, 2) Group II (n=23) : bone cement augmented short segment fixation with posterolateral bone fusion, 3) Group III (n=21) : bone cement augmented short segment percutaneous screw fixation without bone fusion (Fig. 1). All procedures were performed by the same surgeon. Clinical outcomes were assessed using a visual analogue scale (VAS) and modified Mac Nab's criteria. The effects of the procedures were analyzed preoperatively, 10 days postoperatively, and at final follow-up. Radiological findings, including height restoration, kyphotic angle, and other systemic complications, were analyzed. Extent of vertebral body collapse was determined using vertebral heights at the point of maximal collapse on lateral radiographs or on midsagittal computed tomography scans. Vertebral heights are reported as fractions of referenced height. Kyphotic angle was measured by drawing a straight line from the superior endplate of the vertebra one level above the fractured body and a straight line from the inferior endplate of the vertebra one level below the fractured body. Patients' characteristics are summarized in Table 1. The three groups were compared with respect to age, gender, mean T-score, kyphotic angle, preoperative degree of pain, and vertebral height. All data presented in the Table 1 are median values. Preoperative group differences were evaluated using the Student's t-test for unpaired data, and intra-group changes associated with the procedure were evaluated using the Student's t-test for paired data. p values of <0.05 were considered statistically significant.
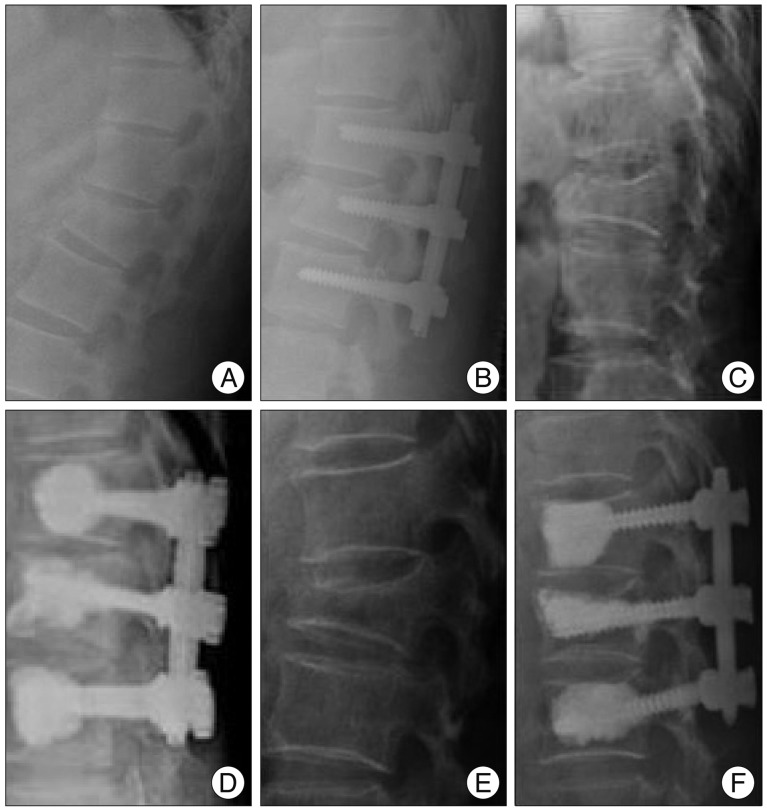
Three representative cases of each group. A and B : Short segment screw fixation with posterolateral bone fusioin (Group I). C and D : Bone cement augmented short segment fixation with posterolateral bone fusioin (Group II). E and F : Bone cement augmented short segment percutaneous screw fixation without bone fusioin (Group III).
RESULTS
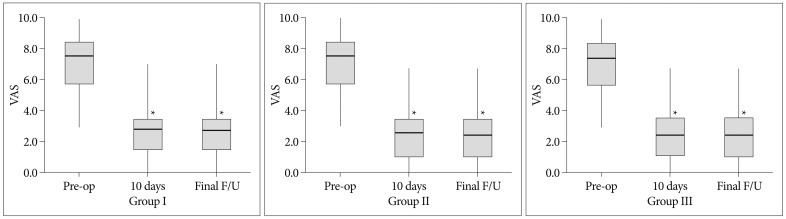
Group demographics, that is, age, gender, pain, vertebral height, mean T-score, mean follow-up period, and mean kyphotic angle were not significantly different. Significant pain relief was achieved in all three groups at last follow-up (p<0.01).
For Group I, mean VAS scores were; 7.6 before surgery, 3.0 at 10 days after surgery, and 3.0 at last follow-up. For Group II, mean VAS scores were; 7.5 before surgery, 2.7 at 10 days after surgery, and 2.5 at last follow-up. For Group III, mean VAS scores were; 7.5 before surgery, 2.5 at 10 days after surgery, and 2.6 at last follow-up (Fig. 1). Most patients achieved an 'excellent' or 'good' result at final follow-up according to modified MacNab's criteria.
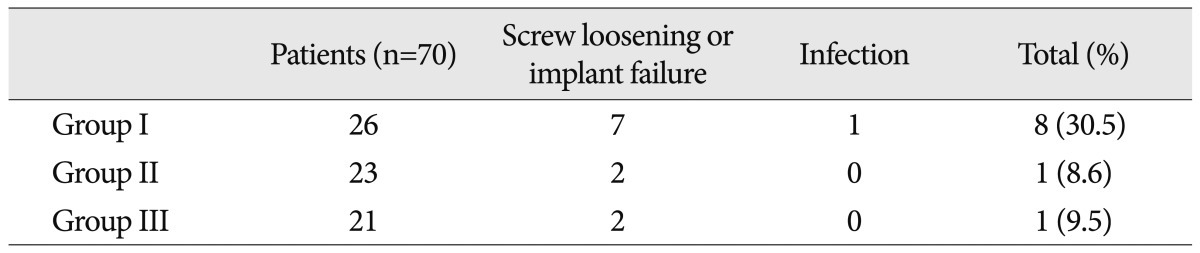
However, patients that underwent short segment screw fixation with bone fusion (Group I) showed higher complication rates for screw loosening and implant failure after the procedure than patients in Group II or III (p=0.002). The inter-group pairwise comparisons of complications revealed no significant difference between Group II and III (p=0.279) (Table 2).
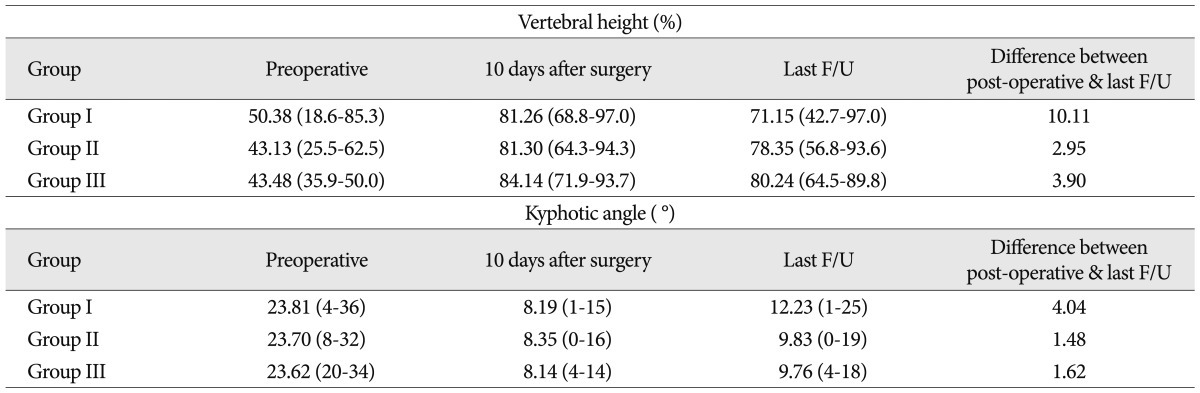
Screw loosening or implant failure was detected in 7 Group I patients (26.9%), 2 Group II patients (8.6%), and 2 Group III patients (9.5%) during the follow-up period (Fig. 3, 4). In Group I, one male patient developed symptomatic infectious spondylitis that needed revision surgery at six months after screw fixation. No major complications related to bone cement, such as, pulmonary embolism or epidural leakage, were encountered in Group II or III, although asymptomatic cement leakage occurred into the disc space or posterior spinal canal in some patients. Mean kyphotic angle and vertebral height increased significantly at last follow-up in all three Groups (p<0.01), but Group I showed more correction loss of kyphotic deformities and vertebral height loss than with Group II or III (Table 3).

A case of screw loosening in 48-year-old male patient in Group I. A : Preoperative simple lateral radiograph shows an L1 burst fracture. B : Postoperative simple lateral radiograph shows correction of kyphosis and short segment screw fixation. C : Postoperative simple lateral radiograph obtained at 6 months after surgery reveals screw pull-out and aggravated kyphosis. A surgical treatment removing the screws was performed in this case.

A case of asymptomatic screw loosening in 49-year male patient in Group III. A and B : Preoperative simple radiographs showing an L2 bursting fracture. C and D : Postoperative simple radiographs showing bone cement augmented short segment fixation using percutaneous screws. E and F : Postoperative simple radiographs obtained at 11 months showing loosening at the L1 level. A surgical treatment removing the screws was not performed in this case.
DISCUSSION
Minimizing the number of vertebral levels in screw fixation is another important goal of internal fixation. Traditional short segment fixation, which is, pedicle screw fixation one level cephalad and one level caudad a fracture, is used to save the motion segments by limiting the number of the fusion segments. Despite the theoretical benefits of motion preservation, clinical studies on traditional short segment instrumentation have yielded disparate results2). Failure to restore anterior column support can lead to secondary kyphosis, depending on the residual load transfer capacity of the fractured vertebral body. However, the trend toward preservation of motion segments using short segment instrumentation has continued to gain popularity, especially when anterior column support is not severely compromised5). In the present study, the radiographic and clinical outcomes of neurologically intact patients with a thoracolumbar burst fracture that underwent short segment fixation at the level of the fracture with or without posterolateral fusion and a vertebral augmentation procedure were analyzed. Although kyphotic angle, vertebral height restoration, and clinical outcome were not significantly different in the three groups, our results show that bone cement augmentation seems to be essential in terms of reducing screw loosening and implant failure rates. The pedicle screw-based instrumentation system has been used widely for the treatment of thoracolumbar fractures, and posterior fixation with pedicle instrumentation not only allows satisfactory fracture reduction but also provides immediate mechanical stability and alignment while preventing additional damage to non-injured segments. With regard to posterior fixation, spinal fusion is usually believed to necessary to reduce loss of kyphosis correction and implant failure. However, short segment fixation with bone has also been associated with considerable rates of implant failure and correction loss2,4).
Some authors have recently reported the results for posterior screw fixation without bone fusion for the treatment of thoracolumbar burst fractures. Sanderson et al.6), in a retrospective study, examined 24 patients who had undergone short-segment fixation without fusion, and concluded that routine posterior or posterolateral fusion is unnecessary. In 2006, Wang et al.8), also reported satisfactory results for short-segment fixation without fusion in surgically-treated thoracolumbar burst fractures, and found that low back outcome scores were no different for patients treatment with or without bone fusion. However, in the osteoporotic or osteopenic spine, the screw anchoring effect is reduced and the probability of hardware failure is high, and thus, the possibility of non-union is increased7). Therefore, screw loosening or vertebral collapse may occur more frequently after screw fixation without bone fusion in osteoporotic or osteopenic spines. However, insertion of pedicle screws at the fracture level results in a segmental construct that improves biomechanical stability by protecting the fractured body and by supporting the anterior column indirectly3). In addition, the insertion of bone cement to augment pedicle screws at the fracture level probably results in a segmental construct with improved biomechanical stability by providing protection to the fractured vertebral body and indirectly supporting the anterior column3). Furthermore, Bone cement augmentation at fractured level itself and adjacent vertebrae can significantly reduce pedicle screw bending and increase initial stiffness in the flexion-extension plane. Wittenberg et al.9) reported that PMMA can increase pull-out strength from 96% to 262% and transverse bending stiffness by up to 153%9). In the present study, we obtained good surgical outcomes in all three groups. Mean kyphotic angle and vertebral height increased significantly at last follow-up in all three groups. However, improved vertebral height and kyphotic angle were maintained during the follow-up and lower complication rates were observed in bone cement augmented screw fixation groups (Group II and III). As a result, bone cement augmented screw fixation procedure including fractured level was helpful for prevent screw loosening and implant failure. Moreover, due to the advance in minimally invasive instrumentation, bone cement augmented, percutaneous screw fixation was a safe and effective management to reduce screw loosening implant failure for the thoracolumbar burst fractures without neurologic deficits. All surgical procedures in this study were performed by a single surgeon to eliminate the effects of different surgeons on outcome variables. However, larger-scale, multicenter studies involving more surgeons and fracture types are required to validate our results.
CONCLUSION
Bone cement augmentation procedure is an effective and reliable operative technique for reducing screw loosening and implant failure after short segment fixation for thoracolumbar burst fractures accompanying osteopenia.
Acknowledgements
This study was supported by AO spine research fund.