An Unusual Cervical Spinal Meningioma in a Child
Article information
Abstract
The incidence of spinal meningioma is very rare in children. A 14-year-old girl presented with right arm weakness, gait disturbance, and urinary incontinence. Cervical magnetic resonance imaging revealed an intradural extramedullary tumor dorsal to the spinal cord in the level of C1. The tumor was totally removed despite the severe cord compression. Meningotheliomatous meningioma was diagnosed after histological examination.
INTRODUCTION
Spinal meningioma, like intracranial meningioma, is extremely rare in children. Meningiomas, unlike the case of the adult population, account for less than 5% of intradural extramedullary spinal cord tumors3,12). Tumor locations also differ from those seen in adults. These rare lesions tend to occur in the cervical or thoracic region in children10). The recognition and complete excision of these tumors are very important in view of their benign nature and complete curability. With a review of the literature, we present a rare case of a 14-year-old girl with cervical spinal meningioma.
CASE REPORT
A 14-year-old girl was admitted to our hospital in May 2012 due to right arm weakness and gait disturbance lasting for 2 weeks. She had also urinary incontinence. On general appearance, this patient looked healthy. Her neurological examination revealed right hemiparesis (Grade 2-3/4) that was more severe in the upper extremity than the lower and in the distal region than the proximal. The right biceps reflex, knee jerk, and ankle jerk were hyperactive. The Babinski sign was not found. There was no discernible sensory level.
A magnetic resonance imaging (MRI) revealed an intradural extramedullary mass that was an isointense lesion on T1- and a slightly hyperintense on T2-weighted images, dorsal to the spinal cord in the level of C1. Spinal meningioma showed an intense enhancement on MRI after gadolinium administration (Fig. 1).
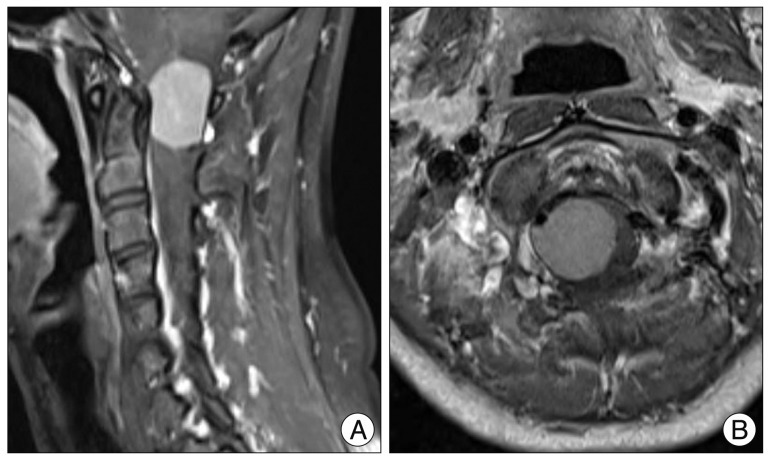
Preoperative midsagittal (A) and axial (B) T1-weighted magnetic resonance images obtained after gadolinium administration, demonstrating a well enhanced intradural extramedullary tumor posterior to the cervical spinal cord.
Surgery was performed in the prone position. A rigid head holder, such as the skeletal fixation device, was used to secure the head in a neutral position. A laminectomy was performed with Kerrison punch at the C1 level. The dura mater was not tense. The operation was performed using a microsurgical technique. The dura was then opened straightly in the midline. A yellowish, hard tumor of oval shape was found immediately. The tumor was found to be intradural-extramedullary (Fig. 2). The thinned cervical cord was displaced laterally by the tumor. First, the central decompression of the tumor was done with the use of the ultrasonic surgical aspirator. The well-circumscribed, encapsulated tumor was separated easily from the surrounding tissue, allowing total excision. During the dissection, a major intradural vessel did not adhere to the tumor. After the tumor removal, hemostasis was obtained with warm saline irrigation and avitene hemostatic collagen. The dura was then closed primarily in a watertight fashion. The wounds were closed without tension.
Postoperatively, the patient received systemic dexamethasone. Over the few days, her motor strength was markedly improved. The postoperative magnetic resonance study was done 2 days after the surgery (Fig. 3). Her neurological function had completely returned to its normal level at the time of discharge, 3 weeks after the surgery.
The histology examination of the tumor revealed that it was a meningotheliomatous meningioma. Individual tumor cells had indistinct cytoplasmic boundaries and nuclear clearing, cellular whorls, and psammoma body were noticed (Fig. 4).
DISCUSSION
In children, tumors of the spinal canal constitute a smaller proportion (5 to 10%) of tumors of the central nervous system than in adults. The various types of tumors that occur in children also differ from those seen in adults11). There has not been much study on the pediatric spinal meningioma series. Meningioma of the brain is also very rare in children younger than 16 years old, with an incidence as low as 2.19% of whole-brain tumors. The ratio of intracranial to intraspinal tumors in children is approximately 20 : 1; thus, intraspinal meningioma in childhood is extremely rare9).
These rare lesions tend to occur in the cervical or thoracic region in children. Meningioma occurrence in the lumbosacral area is the least common but not unheard of. Spinal meningioma may occur not only in the intradural, extramedullary space (83%) but also in the extradural space (14%) and intradural, intramedullary space (3%)10).
Compared to children, adult spinal meningioma commonly occurs in middle aged women in the form of a benign lesion. It accounts for approximately 25-46% of spinal tumors. The most frequent location of spinal meningioma is the thoracic region in the intradural-extramedullary spaces2).
The patient presented here is a 14-year-old girl with upper cervical intradural extramedullary meningioma. Dermoids, epidermoids, nerve sheath tumors, and diffuse leptomeningeal tumors were also considerated to be a diagnostic candidate for the intradural extramedullary tumors before surgery.
Cervical kyphosis does not commonly develop after cervical laminectomy. Nonetheless, postlaminectomy deformities are most common in pediatric patients with an immature skeletal system, but are also more common in young adults (<25 years of age) than older adults.
The risk of postlaminectomy kyphosis should be always considered before approaching tumors in the spinal canal for resection, especially in higher-risk patients such as children and young adults. Multiple risk factors are associated with cervical spine deformity after laminectomy, including age, the extent of laminectomy and facetectomy, the number of laminae removed, the location of laminectomy (upper, middle, or lower cervical spine), the preoperative loss of lordosis, the pathological condition in the intramedullary spinal cord, and the radiation treatment in the spine1).
To decrease the risk of postlaminectomy kyphosis in our case, efforts were made to leave the facets intact and preserve the facet capsules when performing the muscle detachment. Only one-level laminectomy was only performed.
Spinal meningioma arises from cap cells of the arachnoid membrane and originates in proximity to nerve root, accounting for its predominantly lateral location2,8). In our case, the tumor originated from an upper dorsal cervical rootlet. Reports on pediatric spinal meningioma that mention histology indicate psammomatous and meningotheliomatous patterns as well as malignant meningioma4,6,7). The hallmark of psammomatous meningioma is the presence of a cellular whorl growth pattern with central psammoma bodies. Meningotheliomatous meningiomas, also known as syncytial meningiomas, are characterized by large nucleoli surrounded by polygonal cytoplasmic borders. Intranuclear cytoplasmic inclusions or whorl formations may appear as well. Increased cellularity and the presence of mitotic figures push the diagnosis to one of malignancies10). Histologically, our patient's tumor was a meningotheliomatous meningioma with increased cellularity and rare mitoses.
Advances in radiological and surgical techniques such as computed tomography (CT), MRI, intraoperative ultrasound, evoked responses, ultrasonic aspirators, and lasers have contributed to better clinical results. The best treatment for meningioma is surgery. The goal of surgery must be total resection. The gross total removal is possible in most cases. However, there is frequently significant spinal cord compression. When the tumor is ventral to the cord and calcified, surgery becomes more hazardous and may damage the cord7). Excessive manipulation of the cord should be avoided during resection. Usually the prognosis of these tumors is good when they are completely resected, showing the need for early diagnosis and timely intervention.
However, meningioma may recur, especially as a result of incomplete resection. In children, meningioma tends to grow rapidly and undergoes malignant changes9). There are few long-term studies that examine the recurrence rate in both adult and children. Recurrences range from 1.3% to 32%2). Klekamp and Samii5) demonstrated that partial tumor removal, arachnoid scarring, primary dural suture, surgery on a recurrent meningioma, and male sex are significant risk factors for a clinical recurrence.
CONCLUSION
Because the tumor of our patient was diagnosed early and removed completely, the rapid recovery of neurologic deficit could be achieved. The operation was successful. Since the recurrence rate in pediatric spinal meningioma is not low, we need to conduct a long-term follow-up study to determine whether a tumor recurs.


