Kim, Oh, Song, and Jeon: Trend of Intensive Care Unit Admission in Neurology-Neurosurgery Adult Patients in South Korea : A Nationwide Population-Based Cohort Study
Abstract
Objective
We aimed to examine trends in critically ill neurology-neurosurgery (NNS) patients who were admitted to the intensive care unit (ICU) in South Korea and identify risk factors for in-hospital mortality after ICU admission in NNS patients.
Methods
This nationwide population-based retrospective cohort study enrolled adult NNS adult patients admitted to the ICU from 2010 to 2019 extracted from the National Health Insurance Service in South Korea. The critically ill NNS patients were defined as those whose main admission departments were neurology or neurosurgery at ICU admission. The number of ICU admission, age, and total cost for hospitalization from 2010 to 2019 in critically ill NNS patients were examined as trend information. Moreover, multivariable logistic regression modeling was used to identify risk factors for in-hospital mortality among critically ill NNS patients.
Results
We included 845474 ICU admission cases for 679376 critically ill NNS patients in South Korea between January 1, 2010 to December 31, 2019. The total number of ICU admissions among NNS patients was 79522 in 2010, which increased to 91502 in 2019. The mean age rose from 62.8 years (standard deviation [SD], 15.6) in 2010 to 66.6 years (SD, 15.2) in 2019, and the average total cost for hospitalization per each patient consistently increased from 6206.1 USD (SD, 5218.5) in 2010 to 10745.4 USD (SD, 10917.4) in 2019. In-hospital mortality occurred in 75455 patients (8.9%). Risk factors strongly associated with increased in-hospital mortality were the usage of mechanical ventilator (adjusted odds ratio [aOR], 19.83; 95% confidence interval [CI], 19.42-20.26; p<0.001), extracorporeal membrane oxygenation (aOR, 3.49; 95% CI, 2.42-5.02; p<0.001), and continuous renal replacement therapy (aOR, 6.47; 95% CI, 6.02-6.96; p<0.001). In addition, direct admission to ICU from the emergency room (aOR, 1.38; 95% CI, 1.36-1.41; p<0.001) and brain cancer as the main diagnosis (aOR, 1.30; 95% CI, 1.22-1.39; p<0.001) are also potential risk factors for increased in-hospital mortality.
Conclusion
In South Korea, the number of ICU admissions increased among critically ill NNS patients from 2010 to 2019. The average age and total costs for hospitalization also increased. Some potential risk factors are found to increase in-hospital mortality among critically ill NNS patients.
Key Words: Critical care ┬Ę Intensive care units ┬Ę Mortality ┬Ę Neurology ┬Ę Neurosurgery.
INTRODUCTION
The intensive care unit (ICU) is a specialized unit within a hospital that provides care for critically ill patients and requires more support and monitoring than a regular ward [ 27]. As the volume of neurosurgical operations increased in the mid-1970s, the demands for neurological intensive care increased in both the United States and Europe [ 21]. With staffed with trained neuro-intensivists and special nursing staff, the role of neurological intensive care among neurology-neurosurgery (NNS) patients has been an important issue of modern critical care medicine, and it will be emphasized more in the future [ 13]. There has been special challenges in NNS patients in ICU because both systemic derangements, such as cardiac and respiratory care and intracranial processes, require neurocritical care [ 15, 24]. Previous reports showed clinical characteristics and outcomes among NNS patients who required ICU admission. A large-scale analysis in the United Kingdom reported that neurological critical care is associated with improved survival outcomes in patients who underwent a specialized intensive care technique [ 4]. Moreover, a recent meta-analysis reported that neurocritical care was associated with improved survival and functional outcomes in critically ill NNS patients with brain injury [ 18]. However, there are not enough reports regarding neurocritical care for NNS patients. A recent study using a survey from the Korean Neurosurgical Society reported that South Korean hospitals had exerted effort to implement neuro intensivist systems across South Korea [ 8]. However, studies focused on perspectives of South Korean hospital [ 8] and information regarding clinical characteristics and mortality in critically NNS patients in South Korea are lacking. Therefore, this study aimed to investigate trends in ICU admissions and examine risk factors for in-hospital mortality in critically ill NNS patients in South Korea.
MATERIALS AND METHODS
Ethical statement
This retrospective cohort study based on population data followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines [ 28]. The Institutional Review Board (IRB) approved our study protocol because we used public data from the South Korean National Health Insurance Service (NHIS) database (IRB number : X-2302-808-901). The NHIS also approved data sharing following the deliberation of our study protocol (NHIS grant number : NHIS-2021-1-620). Since we analyzed the anonymized data retrospectively, the IRB exempted us from obtaining informed consent from the participants.
Data source and study population
The NHIS is a single public health insurance system that collects and manages data on disease diagnoses, medical procedures, and medications. In South Korea, physicians must register all medical information using the International Classification of Diseases External 10th revision (ICD-10) codes in the NHIS database to receive reimbursements from the government. The NHIS database also includes demographic and socioeconomic information of all patients in South Korea. We included all adult NNS patients (Ōēź20 years) who were admitted to the ICU between January 1, 2010 and December 31, 2019, in South Korea using prescription codes for ICU admission during hospitalization. Patients with NNS were defined as those whose main admission department was neurology or neurosurgery at ICU admission.
Study endpoints
To understand the trends of the ICU admission among NNS patients during the 10 years, we searched for the number of ICU admission cases, mean age of patients, and mean total cost per patient admitted to the ICU in USD for each year. We then examined the risk factors related to in-hospital and 1-year mortality in all NNS patients admitted to the ICU. The 1-year mortality was defined as any death within 1 year after the date of ICU admission among critically ill NNS patients.
Study parameters
We collected the demographic variables of ICU-admitted NNS patients, such as age and sex, and gathered data on their socioeconomic status, employment status, household income, and area of residence at the time of ICU admission. With the medical aid program, the South Korean government covers nearly all medical expenses for those who cannot afford insurance premiums or have difficulty supporting themselves financially due to medical disasters. In addition to the medical aid program group, the remaining patients were divided into four quartiles according to household income level. In the residence category, urban areas included Seoul and other metropolitan cities, whereas rural areas included all other areas. The lengths of hospital stay and ICU stay were also recorded. The Charlson comorbidity index was determined for each patient using ICD-10 codes ( Supplementary Table 1) to evaluate the comorbid disease status [ 25]. Patients were admitted to the neurology or neurosurgery department, and whether they were admitted to the emergency room (ER) was determined. The patients were divided into three groups based on the level of the hospital where they were admitted to the ICU : tertiary general, general, and other hospitals. Hospitals in South Korea must have a minimum of 30 beds and the ability to provide inpatient care to be designated as medical institutions. A ŌĆśgeneral hospitalŌĆÖ is equipped with Ōēź100 beds, with departments according to the number of beds with specialists for each department. Among general hospitals, the Minister of Health and Welfare in South Korea designates medical institutions that specialize in medical practices with high levels of difficulty for severe diseases as tertiary general hospitals. We also gathered information regarding the medical procedures patients underwent in hospitals, such as surgery, mechanical ventilation, extracorporeal membrane oxygenation (ECMO), and continuous renal replacement therapy (CRRT). The outcomes of the hospital stay were categorized into four groups : 1) same hospital follow-up, 2) transfer to a long-term care center facility, 3) death during hospitalization, and 4) discharge and other outpatient clinic follow-ups. We collected data on the main diagnoses of NNS patients admitted to the ICU using the ICD-10 codes, which the NHIS assigns after hospital discharge or death. The main diagnosis is a major disease for which most treatment and examinations are required during hospitalization and is determined by the NHIS in South Korea. For example, if an NNS patient was admitted to the ICU and was diagnosed of having cerebrovascular disease and epilepsy, diseases that required more prescriptions or examinations in the patient during hospitalization were considered the main diagnosis by NHIS. The specific ICD-10 codes of main diagnosis at ICU admission in Detailed information of ICD-10 codes of main diagnosis are presented in Supplementary Table 2. We classified the top 12 diseases according to frequency and classified all diseases that did not correspond to these into the ŌĆśothersŌĆÖ category.
Statistical analyses
The clinical and pathological traits of the patients were described using the mean value with standard deviation (SD) for continuous variables, while categorical variables are expressed as numbers and percentages. A multivariable logistic regression model was used to identify the factors related to in-hospital mortality among critically ill NNS patients. In the multivariable model, all covariates were adjusted. The results were presented as adjusted odds ratios (aORs) with 95% confidence intervals (CIs). The main diagnosis at ICU admission and the 1-year mortality rate according to the main diagnosis at the ICU were presented as numbers with their corresponding percentages. All statistical analyses were performed using IBM SPSS Statistics for Windows (version 25.0; IBM Corp., Armonk, NY, USA), and statistical significance was set at p<0.05.
RESULTS
Study population
This study enrolled 845474 ICU admission cases for 679376 critically ill NNS patients in South Korea between January 1, 2010 to December 31, 2019. Table 1 shows the clinical and pathological features of critically ill NNS patients. Patients had a mean age of 64.7 years (SD, 15.4), and 53.7% were male. Patients stayed in the ICU for a mean of 5.0 days (SD, 6.9) and in the hospital for a mean of 16.9 days (SD, 13.2). Of the 845474 ICU admissions, 74.8% (632222/845474) had neurosurgery-related conditions, and 61.7% (521530/845474) arrived through the ER. In-hospital mortality occurred in 75455 patients (8.9%). Furthermore, the 90-day and 1-year mortality rates after ICU admission were 17.4% and 26.4%, respectively. The mean hospitalization cost for each patient was 7719.2 USD (SD, 7164.2).
Diagnosis at ICU admission among critically ill NNS patients
Table 2 shows the main diagnoses upon ICU admission. Cerebrovascular disease (I6*, 55.7%) was the most frequent diagnosis, followed by intracranial injury (S06, 16.5%), benign neuroendocrine tumor (D3A, 3.6%), and epilepsy or seizures (G40, 3.1%).
Trends of ICU admission among critically ill NNS patients
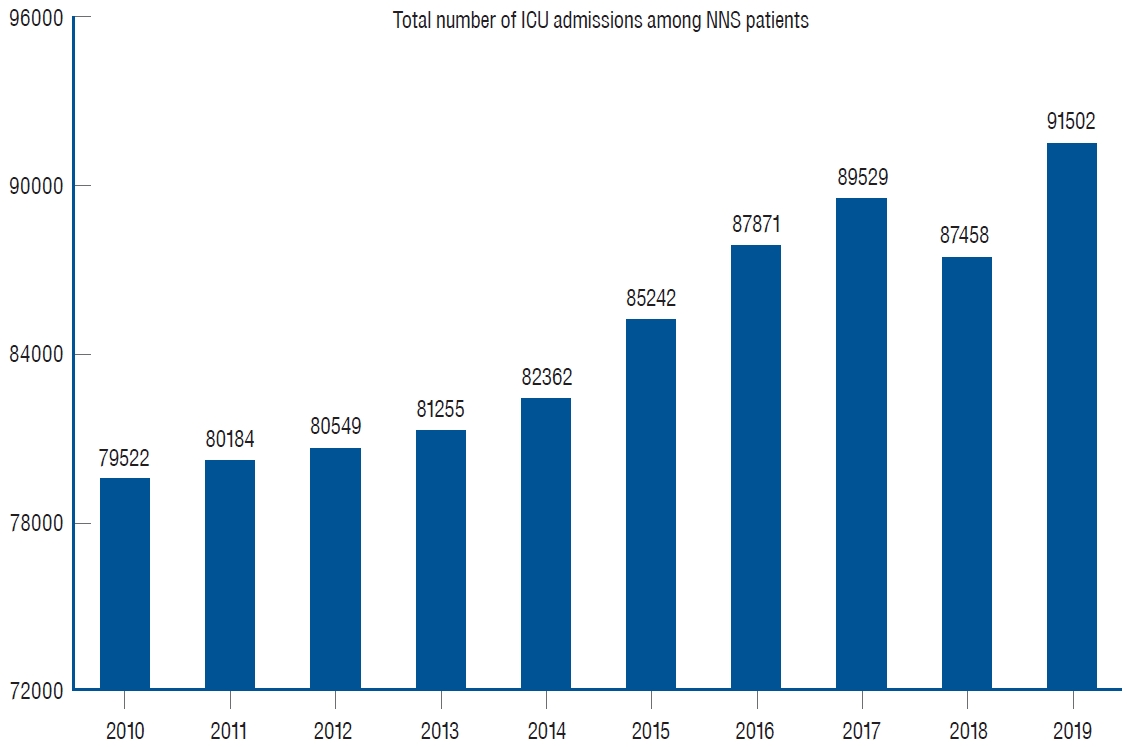
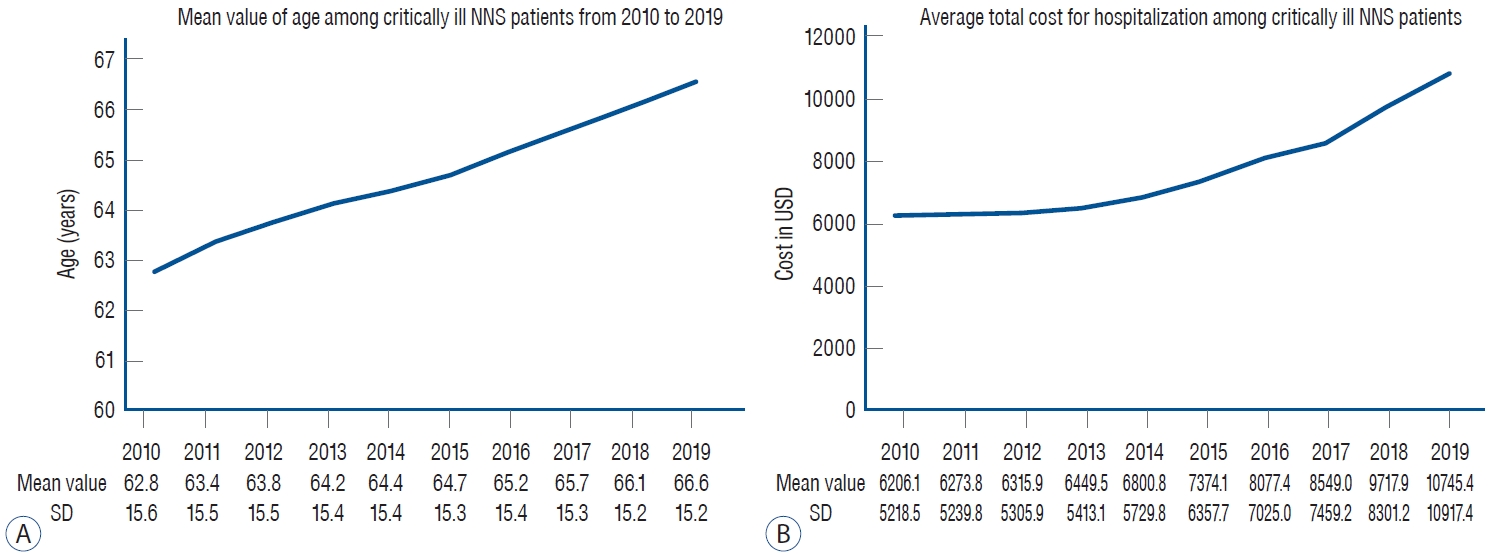
The total number of ICU admissions among NNS patients was 79522 in 2010 and increased to 91502 in 2019 ( Fig. 1). The mean age rose from 62.8 years (SD, 15.6) in 2010 to 66.6 years (SD, 15.2) in 2019 ( Fig. 2A), and the average total cost for hospitalization per each patient consistently increased from 6206.1 USD (SD, 5218.5) in 2010 to 10745.4 USD (SD, 10917.4) in 2019 ( Fig. 2B).
In-hospital mortality and 1-year mortality
Table 3 presents the results of the multivariable logistic regression model for in-hospital mortality among ICU-admitted patients in South Korea from 2010 to 2019 among critically ill NNS patients. In-hospital mortality increased with older age (aOR, 1.03; 95% CI, 1.03-1.03; p<0.001), neurosurgery-related admission (aOR, 1.04; 95% CI, 1.02-1.07; p=0.001), and admission via ER (aOR, 1.38; 95% CI, 1.36-1.41; p<0.001). The use of a mechanical ventilator (aOR, 19.83; 95% CI, 19.42-20.26; p<0.001), ECMO support (aOR, 3.49; 95% CI, 2.42-5.02; p<0.001), and CRRT (aOR, 6.47; 95% CI, 6.02-6.96; p<0.001) were also associated with increased in-hospital mortality. Regarding the main diagnoses at ICU admission, the brain cancer (aOR, 1.30; 95% CI, 1.22-1.39; p<0.001) and secondary brain tumor (aOR, 1.14; 95% CI, 1.04-1.24; p<0.001) were associated with higher in-hospital mortality. Patients who underwent surgery showed lower in-hospital mortality (aOR, 0.59; 95% CI, 0.58-0.61; p=0.004). Compared to the patients in 2010, those admitted in 2011 were associated with lower in-hospital mortality (aOR, 0.93; 95% CI, 0.89-0.96; p<0.001), and aOR continuously decreased as the year passed. Supplementary Table 3 shows the 1-year mortality rate according to the main diagnosis in the ICU among critically ill NNS patients. The top three diagnoses with the highest 1-year mortality rates were secondary brain tumors (61.8%), brain cancer (45.8%), and extrapyramidal and movement disorders (37.5%).
DISCUSSION
In South Korea, the number of ICU admissions among critically ill NNS patients increased from 2010 to 2019. Additionally, the mean age and total cost for hospitalization also increased from 2010 to 2019. The most common diagnosis in the ICU was cerebrovascular disease. In-hospital mortality was positively associated with hospital admission through the ER, brain cancer, and the use of supporting invasive devices (mechanical ventilation, ECMO, and CRRT).
The growth of the aging population and subsequent increase in neurocritical elderly patients have contributed to recent trends in increasing ICU admissions and the associated burden. South Korea became an aged society in 2017, which is defined as a proportion of the population aged 65 years or older of Ōēź14.0% [ 2]. It is expected to become a super-aged society, defined as having a proportion of the population aged 65 years or older of Ōēź20.0% in 2025 [ 2]. This study showed that a growing proportion of the aged population has resulted in an increase in both the mean age and number of ICU-admitted critically ill NNS patients. Moreover, as the Korean population has grown old rapidly over the recent period, the need for neurocritical care and its costs also increases. Neurologic diseases that require neurocritical care are known as costly and resource-demanding diseases with poor hospital outcomes [ 20]. Due to the high cost of neurocritical care, the health burden is a crucial issue in many countries, especially with resource-limited settings [ 19]. In addition to these findings, our result suggested that the health burden associated with the cost of neurocritical care in critically ill NNS patients will also be an important issue in South Korea. In this study, the most common main diagnosis upon ICU admission among critically ill NNS patients was cerebrovascular disease (I6), followed by intracranial injury (S06), benign neuroendocrine tumor (D3), and epilepsy or seizure (G40). According to the Point Prevalence in Neurocritical CarE (PRINCE) Study, which included 147 participating sites from 31 countries, the most common primary diagnoses were subarachnoid hemorrhage (SAH), spontaneous intracerebral hemorrhage (ICH), subdural hematoma, and severe traumatic brain injury (TBI). The primary diagnosis varies by country, with SAH being the most common in Europe, Latin America, and Oceania. Severe TBI is the most common type of injury in Asia and the Middle East [ 26]. In this study, we identified some potential risk factors for in-hospital mortality among critically ill NNS patients. Patients admitted through the ER are expected to be at risk in terms of severity and comorbidities since they are in an unexpectedly deteriorated medical state and need immediate intensive care; this was also proven in the PRINCE Study Part 2 (emergency room vs. direct admission) [ 26]. Patients admitted to the neurosurgery department were more likely to have poor prospective outcomes since they needed alleviation of increased intracranial pressure (from midline shift, continuous bleeding, disruption of parenchyma, ICH growth, mass effect, etc.) and prevention of further brain injury resulting from the toxic effect of blood degradation products and the inflammatory response after ICH [ 23]. Moreover, neurosurgery poses inevitable/unavoidable dangers to patients, such as intracranial infection [ 3], postoperative pulmonary complications [ 1], rebleeding [ 5], or increased abdominal pressure [ 6]. One in four patients underwent additional procedures following non-elective surgery [ 29], and the mortality rate of patients who underwent nonelective neurosurgery was higher [ 29]. Patients supported by equipment such as mechanical ventilators, ECMO, and CRRT are in a major organ failure stage with unstable hemodynamics and are probably associated with prolonged hospitalization and higher in-hospital mortality [ 12, 22]. Patients with brain cancer or secondary brain tumors were highly associated with both in-hospital and 1-year mortality rates. The incidence and mortality rates of brain cancer have been reported to be 3.4 and 2.5 per 100000 people in the world [ 7]. Malignant tumors account for approximately one-third of all brain and other central nervous system tumors diagnosed in the state but account for most deaths from the disease [ 7] : 5-year survival for patients diagnosed with malignant tumors was 36% overall. Glioblastoma accounts for nearly half of all malignant tumors in all ages combined, and the 5-year survival rate is only 7% [ 14]. Non-small cell lung cancer constitutes most tumor types in patients with brain metastases, followed by other cancers, such as small cell lung cancer, melanoma, and breast cancer [ 14]. Patients with brain metastases at the presentation of systemic malignancy have indicated a median survival of 12 months or less across nearly all primary sites [ 14]. Among older patients (age Ōēź65 years) with brain metastases who are diagnosed at or after primary malignancy, the prognosis is even poorer, with a median survival of 4 months or less for nearly all evaluable primary sites [ 11]. It is important to carefully interpret the high 1-year mortality rate of 37.5% (1228/3438) in patients with extrapyramidal and movement disorders. The patients with extrapyramidal and movement disorders in this study were in a critically ill condition. We only included critically ill NNS patients who required ICU admission. For example, patients with ParkinsonŌĆÖs disease were admitted to ICU due to several systemic causes [ 17], and their prognosis was determined by the inherent morbidity and mortality of the critical illness [ 16]. Musculoskeletal system and connective tissue diseases were weakly associated with in-hospital mortality and showed a low 1-year mortality rate. Reasons for admission after spinal surgery are mostly neurological and cardiac-related issues [ 9]. As connective tissue diseases are relatively rare and often require immunosuppressive therapy, the main causes of ICU admission are sepsis (43%), respiratory failure, neurological involvement, and post-surgical care [ 10]. Our study has several limitations. First, we could not differentiate the types of ICUs (closed, semi-open, or open) to which critically ill NNS patients were admitted. Second, we were unable to adjust for confounding variables such as body mass index, exercise, alcohol consumption, and smoking, owing to the lack of information from the NHIS database. Third, there may have been a selection bias arising from critically ill NNS patients who were too sick to be admitted to the ICU or when the number of ICU beds was insufficient. Fourth, we used the ICD-10 codes as the main diagnoses at ICU admissions that were registered by neurologists or neurosurgeons. Therefore, the accuracy of the main diagnosis could be argued because many neurologists or neurosurgeons were involved in this determination of main diagnoses in many cases of ICU admission among critically ill NNS patients. Finally, we did not adjust for disease severity in patients admitted to the ICU using a standardized health evaluation tool.
CONCLUSION
The number of ICU admission among critically ill NNS patients increased from 2011 to 2019 in South Korea. The average age and total cost of hospitalization also increased during 2011-2019. Some potential risk factors (admission through ER, neurosurgery department admission, and the need for invasive supporting devices) were identified to increase in-hospital mortality among critically ill NNS patients. These findings provide insights into the aspects of neurocritical care that require further research to improve ICU-related mortality and can help inform future changes in critical care medicine in terms of health policy and medical fields for critically ill NNS patients in South Korea.
Fig.┬Ā1.
Total number of intensive care unit (ICU) admission among neurology-neurosurgery (NNS) patients from 2010 to 2019. 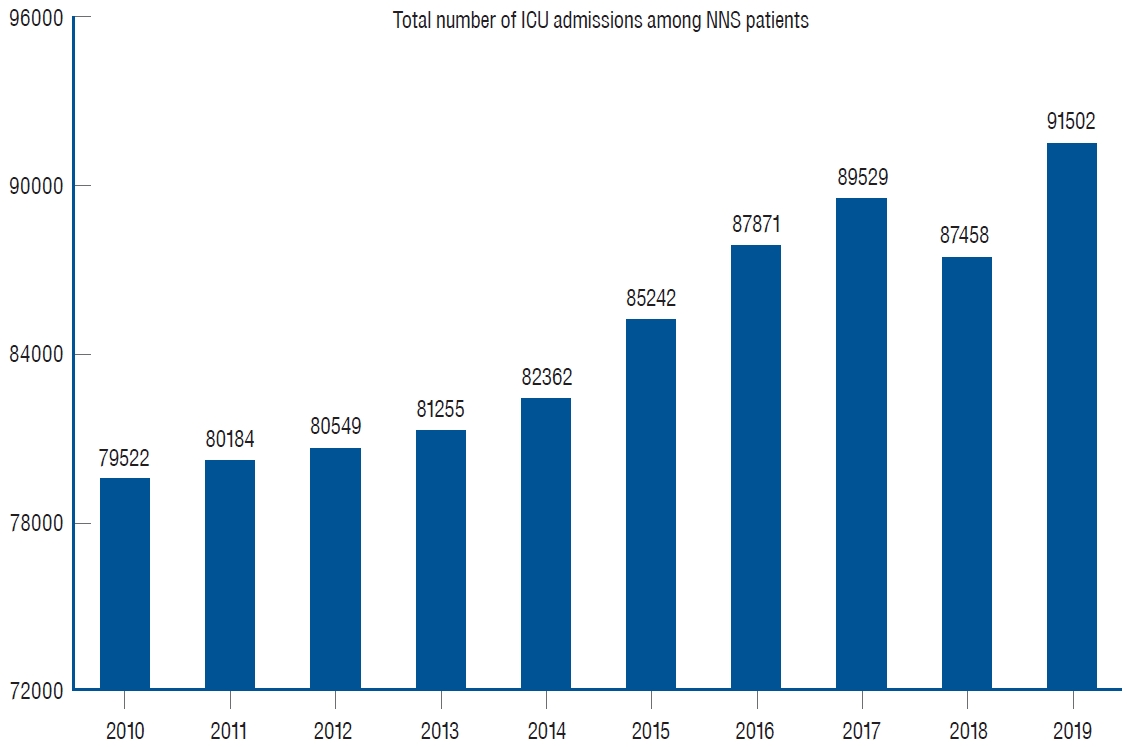
Fig.┬Ā2.
Mean value of age (A) and average total cost (B) for hospitalization among critically ill neurology-neurosurgery (NNS) patients from 2010 to 2019. SD : standard deviation. 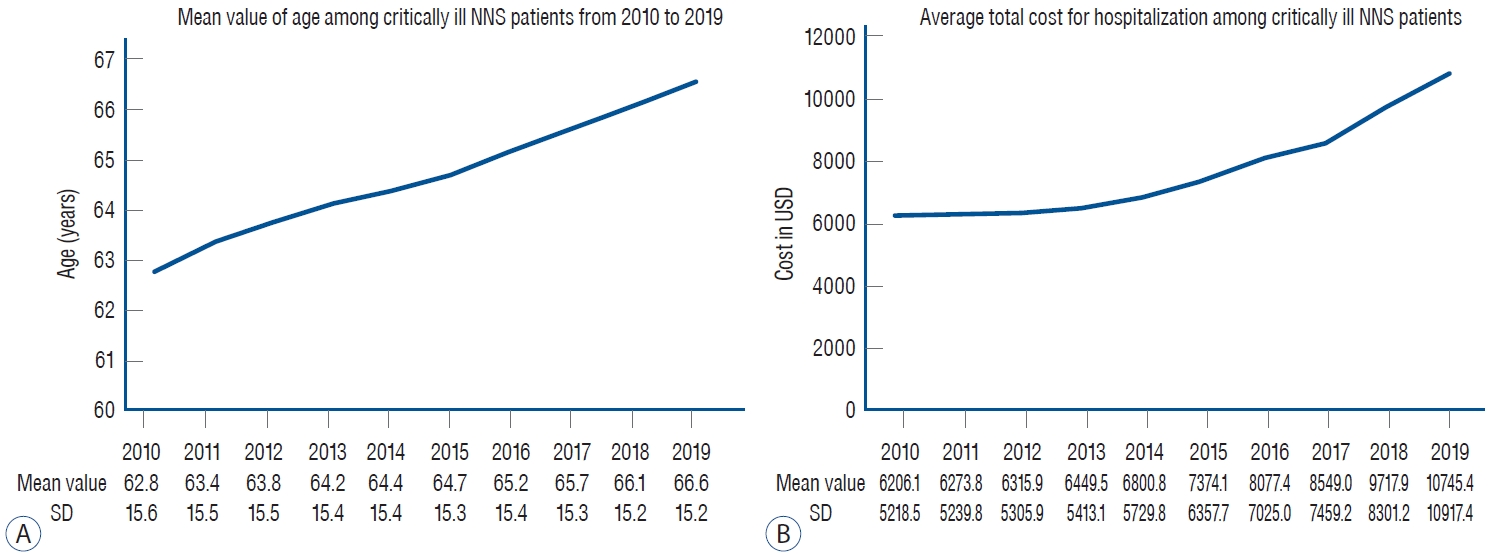
Table┬Ā1.
Clinical and pathological features of critically ill NNS patients
|
Variable |
Value |
|
Age (years) |
64.7┬▒15.4 |
|
Sex, male |
453694 (53.7) |
|
Employed |
388350 (45.9) |
|
Household income level |
|
|
ŌĆāMedical aid program |
65840 (7.8) |
|
ŌĆāQ1, lowest |
129274 (15.3) |
|
ŌĆāQ2 |
123094 (14.6) |
|
ŌĆāQ3 |
154389 (18.3) |
|
ŌĆāQ4, highest |
224466 (26.5) |
|
ŌĆāUnknown |
148411 (17.5) |
|
Residence |
|
|
ŌĆāUrban area |
293242 (34.7) |
|
ŌĆāRural area |
417532 (49.4) |
|
ŌĆāUnknown |
134700 (15.9) |
|
ICU stay (days) |
5.0┬▒6.9 |
|
LOS (days) |
16.9┬▒13.2 |
|
CCI (points) |
2.2 (1.9) |
|
Admission department |
|
|
ŌĆāNeurology |
213252 (25.2) |
|
ŌĆāNeurosurgery |
632222 (74.8) |
|
Hospital admission through ER |
521530 (61.7) |
|
Type of hospital |
|
|
ŌĆāTertiary general hospital |
352630 (41.7) |
|
ŌĆāGeneral hospital |
467109 (55.2) |
|
ŌĆāOther hospital |
25735 (3.1) |
|
Underwent surgery |
497660 (58.9) |
|
Mechanical ventilator support |
215587 (25.5) |
|
ECMO support |
182 (0.0) |
|
CRRT use |
5389 (0.6) |
|
Result of hospitalization |
|
|
ŌĆāSame hospital follow-up |
261870 (31.0) |
|
ŌĆāTransfer to long-term care facility |
54484 (6.4) |
|
ŌĆāDeath during hospitalization |
75455 (8.9) |
|
ŌĆāDischarge, and other outpatient clinic follow up |
453665 (53.7) |
|
90-day mortality |
147448 (17.4) |
|
1-year mortality |
223311 (26.4) |
|
Total cost for hospitalization (USD) |
7719.2┬▒7164.2 |
Table┬Ā2.
Main diagnosis at ICU admission in NNS patients using ICD-10 codes
|
Main diagnosis |
Value |
|
Cerebrovascular disease (I6) |
470699 (55.7) |
|
Intracranial injury (S06) |
139403 (16.5) |
|
Brain cancer (C71) |
17812 (2.1) |
|
Benign neuroendocrine tumor (D3A) |
30821 (3.6) |
|
Epilepsy or seizure (G40) |
26491 (3.1) |
|
Nerve, nerve root and plexus disorder (G5) |
1996 (0.2) |
|
Secondary brain tumor (C79) |
8718 (1.0) |
|
Transient cerebral ischemic attack (G45) |
5395 (0.6) |
|
Musculoskeletal system and connective tissue disease (M) |
22577 (2.7) |
|
Conversion (R56) |
6762 (0.8) |
|
Extrapyramidal and movement disorders (G2) |
3438 (0.4) |
|
Inflammatory disease of CNS (G0) |
8325 (1.0) |
|
Other disease |
103037 (12.3) |
Table┬Ā3.
Multivariable logistic regression for hospital in-hospital mortality
|
Variable |
aOR (95% CI) |
p-value |
|
Age (years) |
1.03 (1.03 to 1.03) |
<0.001 |
|
Sex, male vs. female |
0.99 (0.98 to 1.01) |
0.499 |
|
Employed vs. unemployment |
0.95 (0.93 to 0.97) |
<0.001 |
|
Household income level |
|
|
|
ŌĆāQ2 vs. Q1 (lowest) |
1.00 (0.97 to 1.03) |
0.974 |
|
ŌĆāQ3 vs. Q1 (lowest) |
0.97 (0.94 to 1.00) |
0.068 |
|
ŌĆāQ4 (highest) vs. Q1 (lowest) |
0.94 (0.92 to 0.97) |
<0.001 |
|
ŌĆāMedical aid program vs. Q1 (lowest) |
1.28 (1.23 to 1.33) |
<0.001 |
|
ŌĆāUnknown |
0.90 (0.84 to 0.96) |
0.002 |
|
Residence |
|
|
|
ŌĆāRural area vs. urban area |
0.93 (0.92 to 0.95) |
<0.001 |
|
ŌĆāUnknown vs. urban area |
1.01 (0.94 to 1.09) |
0.704 |
|
CCI (points) |
1.02 (1.00 to 1.03) |
0.062 |
|
Admission department |
|
|
|
ŌĆāNeurosurgery vs. neurology |
1.04 (1.02 to 1.07) |
0.001 |
|
Hospital admission through ER |
1.38 (1.36 to 1.41) |
<0.001 |
|
Type of hospital |
|
|
|
ŌĆāGeneral hospital vs. tertiary general hospital |
1.88 (1.84 to 1.92) |
<0.001 |
|
ŌĆāOther hospital vs. tertiary general hospital |
3.29 (3.13 to 3.45) |
<0.001 |
|
Underwent surgery |
0.59 (0.58 to 0.61) |
<0.001 |
|
Mechanical ventilator support |
19.83 (19.42 to 20.26) |
<0.001 |
|
ECMO support |
3.49 (2.42 to 5.02) |
<0.001 |
|
CRRT use |
6.47 (6.02 to 6.96) |
<0.001 |
|
Year of admission |
|
|
|
ŌĆā2011 vs. 2010 |
0.93 (0.89 to 0.96) |
<0.001 |
|
ŌĆā2012 vs. 2010 |
0.85 (0.82 to 0.89) |
<0.001 |
|
ŌĆā2013 vs. 2010 |
0.86 (0.82 to 0.89) |
<0.001 |
|
ŌĆā2014 vs. 2010 |
0.83 (0.80 to 0.86) |
<0.001 |
|
ŌĆā2015 vs. 2010 |
0.76 (0.73 to 0.79) |
<0.001 |
|
ŌĆā2016 vs. 2010 |
0.72 (0.69 to 0.74) |
<0.001 |
|
ŌĆā2017 vs. 2010 |
0.68 (0.65 to 0.71) |
<0.001 |
|
ŌĆā2018 vs. 2010 |
0.64 (0.62 to 0.69) |
<0.001 |
|
ŌĆā2019 vs. 2010 |
0.57 (0.55 to 0.59) |
<0.001 |
|
Main diagnosis |
|
|
|
ŌĆāCerebrovascular disease |
1 |
|
|
ŌĆāIntracranial injury |
0.96 (0.94 to 0.98) |
0.001 |
|
ŌĆāBrain cancer |
1.30 (1.22 to 1.39) |
<0.001 |
|
ŌĆāBenign neuroendocrine tumor |
0.17 (0.15 to 0.19) |
<0.001 |
|
ŌĆāEpilepsy or seizure |
0.36 (0.33 to 0.39) |
<0.001 |
|
ŌĆāNerve, nerve root and plexus disorder |
0.16 (0.12 to 0.21) |
<0.001 |
|
ŌĆāSecondary brain tumor |
1.14 (1.04 to 1.24) |
0.004 |
|
ŌĆāTransient cerebral ischemic attack |
0.17 (0.14 to 0.22) |
<0.001 |
|
ŌĆāMusculoskeletal system and connective tissue disease |
0.24 (0.21 to 0.26) |
<0.001 |
|
ŌĆāConversion |
0.19 (0.16 to 0.23) |
<0.001 |
|
ŌĆāExtrapyramidal and movement disorders |
0.60 (0.52 to 0.69) |
<0.001 |
|
ŌĆāInflammatory disease of CNS |
0.86 (0.78 to 0.94) |
0.001 |
|
ŌĆāOther disease |
0.92 (0.89 to 0.94) |
<0.001 |
References
3. Beer R, Pfausler B, Schmutzhard E : Infectious intracranial complications in the neuro-ICU patient population. Curr Opin Crit Care 16 : 117-122, 2010   4. Damian MS, Ben-Shlomo Y, Howard R, Bellotti T, Harrison D, Griggs K, et al : The effect of secular trends and specialist neurocritical care on mortality for patients with intracerebral haemorrhage, myasthenia gravis and Guillain-Barr├® syndrome admitted to critical care : an analysis of the Intensive Care National Audit & Research Centre (ICNARC) national United Kingdom database. Intensive Care Med 39 : 1405-1412, 2013    7. Farmanfarma KK, Mohammadian M, Shahabinia Z, Hassanipour S, Salehiniya H : Brain cancer in the world: an epidemiological review. WCRJ 6 : e1356, 2019
9. Kay HF, Chotai S, Wick JB, Stonko DP, McGirt MJ, Devin CJ : Preoperative and surgical factors associated with postoperative intensive care unit admission following operative treatment for degenerative lumbar spine disease. Eur Spine J 25 : 843-849, 2016    10. Kouchit Y, Morand L, Martis N : Mortality and its risk factors in critically ill patients with connective tissue diseases: a meta-analysis. Eur J Intern Med 98 : 83-92, 2022   12. Lee HJ, Son YJ : Factors associated with in-hospital mortality after continuous renal replacement therapy for critically ill patients: a systematic review and meta-analysis. Int J Environ Res Public Health 17 : 8781, 2020    13. Malaiyandi D, Shutter L : Neurocritical care past, present, and future. Crit Care Clin 39 : xiii-xiv, 2023  14. Miller KD, Ostrom QT, Kruchko C, Patil N, Tihan T, Cioffi G, et al : Brain and other central nervous system tumor statistics, 2021. CA Cancer J Clin 71 : 381-406, 2021    15. Moheet AM, Livesay SL, Abdelhak T, Bleck TP, Human T, Karanjia N, et al : Standards for neurologic critical care units: a statement for healthcare professionals from the Neurocritical Care Society. Neurocrit Care 29 : 145-160, 2018    16. Mucksavage J, Kim KS : Challenges in ICU care: the patient with Parkinson's disease. Crit Care Nurs Q 43 : 205-215, 2020  17. Paul G, Paul BS, Gautam PL, Singh G, Kaushal S : Parkinson's disease in intensive care unit: an observational study of frequencies, causes, and outcomes. Ann Indian Acad Neurol 22 : 79-83, 2019    18. Pham X, Ray J, Neto AS, Laing J, Perucca P, Kwan P, et al : Association of neurocritical care services with mortality and functional outcomes for adults with brain injury: a systematic review and meta-analysis. JAMA Neurol 79 : 1049-1058, 2022    19. Prust ML, Mbonde A, Rubinos C, Shrestha GS, Komolafe M, Saylor D, et al : Providing neurocritical care in resource-limited settings: challenges and opportunities. Neurocrit Care 37 : 583-592, 2022    21. Ropper AH : Neurological intensive care. Ann Neurol 32 : 564-569, 1992   22. Sanaiha Y, Bailey K, Downey P, Seo YJ, Aguayo E, Dobaria V, et al : Trends in mortality and resource utilization for extracorporeal membrane oxygenation in the United States: 2008-2014. Surgery 165 : 381-388, 2019   24. Suarez JI : Outcome in neurocritical care: advances in monitoring and treatment and effect of a specialized neurocritical care team. Crit Care Med 34( 9 Suppl):S232-S238, 2006   25. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA : New ICD-10 version of the Charlson comorbidity index predicted inhospital mortality. J Clin Epidemiol 57 : 1288-1294, 2004   26. Venkatasubba Rao CP, Suarez JI, Martin RH, Bauza C, Georgiadis A, Calvillo E, et al : Global survey of outcomes of neurocritical care patients: analysis of the PRINCE study part 2. Neurocrit Care 32 : 88-103, 2020    27. Vincent JL, Marshall JC, Namendys-Silva SA, Fran├¦ois B, Martin-Loeches I, Lipman J, et al : Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med 2 : 380-386, 2014   28. von Elm E, Altman DG, Egger M, Pocock SJ, G├Ėtzsche PC, Vandenbroucke JP, et al : The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370 : 1453-1457, 2007   29. Wahba AJ, Cromwell DA, Hutchinson PJ, Mathew RK, Phillips N : Patterns and outcomes of neurosurgery in England over a five-year period: a national retrospective cohort study. Int J Surg 99 : 106256, 2022  
|
|