INTRODUCTION
Saphenous neuralgia (SN) is a rare clinical syndrome characterized by a tingling sensation, pain, or a burning sensation in the medial calf resulting from entrapment of the saphenous nerve8,12,15,16). The saphenous nerve is a purely sensory nerve, so no associated motor or reflex problems are present in patients with SN15).
In many patients with SN, satisfactory pain relief is expected from conservative treatments, such as medications or nerve blocks15,18). However, the effects of nerve blocking are generally temporary, and a small group of patients show medically intractable pain. More aggressive treatment tools have been considered for such patients, including neurolysis and neurectomy of the saphenous nerve12,13,17,19). However, surgical procedures are invasive and risk further complications.
In this case, we treated a patient with medically intractable SN by pulsed radiofrequency (PRF) and found that it was an effective and low-risk alternative treatment.
CASE REPORT
A 65-year-old male presented with severe pain and a tingling sensation in the right medial knee, calf, and ankle. He walked with a limp due to pain but and not weakness. The patient had experienced severely disabling conditions for over 1 month. The pain and tingling sensation occurred every 5-10 minutes and lasted more than 5 minutes per episode. A neurological examination was normal, except for severe pain and tingling sensation in the right medial knee, calf, and ankle.
Lumbar magnetic resonance imaging (MRI) revealed no acute lesions except for distal degenerative changes at multiple levels. Knee MRI revealed no acute lesion except for mild degenerative osteoarthritis. A nerve conduction study revealed an absence of a right saphenous response in both the medial leg and the infrapatellar region, while normal findings were recorded from the left side. Electromyography was normal for all muscles tested. Before visiting our outpatient clinic, the patient had undergone a variety of treatments, including medication, an intra-articular injection for knee pain, and acupuncture around the right knee and medial calf. However, his symptoms did not improve but instead progressed. Saphenous nerve blocks using a local anesthetic and steroids were performed twice at 1-week intervals with fluoroscopy in our clinic. The target sites of nerve blocks were two point, the saphenous nerve around adductor's canal and the sartorial branch of the saphenous nerve around superficial saphenous vein. These blocks provided temporary pain relief that lasted about 3 days. After the positive results of the diagnostic nerve blocks, the patient was scheduled for PRF neuromodulation of the saphenous nerve.
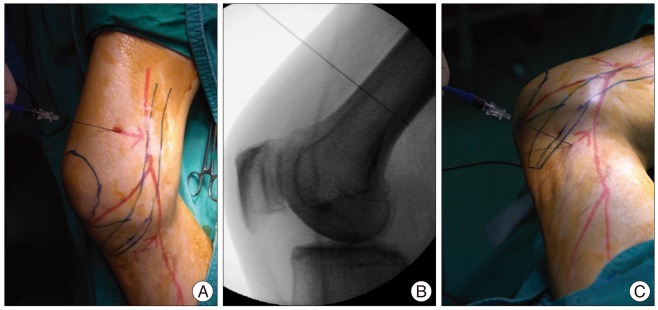
We performed fluoroscopically guided selective saphenous nerve PRF using a model NT1000 radiofrequency generator (NeuroTherm, Middleton, MA, USA). In the operating room, the patient was supine, with the right leg positioned with hip external rotation, hip abduction, and knee flexion. We drew a hypothetical line for the saphenous nerve (complete nerve, infrapatellar branch, and sartorial branch) and the trajectory for the cannula on his leg (Fig. 1). The target site was prepped with betadine and aseptically draped, and the right knee joint and epicondyle were identified under C-arm fluoroscopy. Disposable 20-gauge, 10-cm radiofrequency cannulas (Model S-1505; NeuroTherm) with a 5-mm active tip were inserted at the level of the adductor's canal and below the epicondyle. The introducer needles were withdrawn, and a Model RFDE-15 disposable radiofrequency electrode (NeuroTherm) was advanced (Fig. 2).
Selective stimulation of the sensory fibers (50 Hz) showed concordant pain between 0.3-0.5 V, which confirmed proper localization of the PRF electrode. Motor stimulation was negative. After stimulation, PRF neuromodulation was performed for 240 pulses. The maximal temperature was 42в„ғ. After the procedure, the pain measured on a visual analog scale had decreased by 90% without medication. The pain relief was maintained for 6 months of follow-up without medication.
DISCUSSION
General aspect of saphenous neuralgia
Kopell and Thompson10) first described SN in 1960. Patients with saphenous mononeuropathy experience pain and sensory disturbances within the distribution of the saphenous nerve without motor symptoms. Patients also complain of progressive paresthesias or hypoesthesia12). The etiology of SN can be categorized as idiopathic, traumatic, intrinsic, and iatrogenic causes1-3,11). Patients complain of medial knee and/or leg pains that are worsened by prolonged activity.
More than half of patients with SN are successfully managed with conservative treatment, including medication and nerve block12,20). When patients do not respond to conservative treatments, physicians consider surgical neurolysis or surgical neurectomy11,20). In the present case, saphenous nerve blocks provided temporary pain relief, but symptoms recurred within 3 days. Thus, we recommended PRF neuromodulation for SN.
Anatomical considerations of the saphenous nerve
The saphenous nerve is the terminal sensory branch of the femoral nerve. It supplies sensation to the anteromedial aspect of the leg. The saphenous nerve originates from the femoral nerve in the inguinal region and travels with the femoral artery and vein down into the adductor canal. At the end of the canal, it emerges through the aponeurotic covering, travels along the medial side of the knee behind the sartorius muscle, and then pierces the fascia lata between the tendons of the sartorius and gracilis muscles. Around the medial knee, the infrapatellar nerve branches off the saphenous nerve to supply the prepatellar skin. The saphenous nerve continues down subcutaneously with the long saphenous vein along the medial tibial border. The nerve terminates distally into two branches that supply the ankle and medial foot6). The relative positioning of the saphenous nerve and the long saphenous vein during their course down the medial leg can vary from person to person6).
The entrapment site is most commonly at the adductor canal where the nerve changes course and travels through a fibrous band. This area can be palpated approximately 10 cm above the medial femoral condyle below the sartorius muscle19).
Anatomical consideration for the target of the radiofrequency modulation
Nerve blocks by injections deliver their effects through diffusion to the surrounding tissue, which indicates that relatively inaccurate targeting can be tolerated. However, when modulating the nerve with PRF, the practitioner should be aware of the exact anatomy because lesion creation should be more restricted and exact.
While the medial branch, dorsal root ganglion, and suprascapular nerve have confident bony landmarks for local injection and PRF neuromodulation, the saphenous nerve landmarks are relatively uncertain. Thus, it is difficult to accurately target the saphenous nerve due to its anatomical variations9). For this reason many articles and clinical experiences were often described by using ultrasound for saphenous nerve block. In this case, the nerve was found and targeted around the adductor canal and below the medial epicondyle by using fluoroscopy (Fig. 1).
Mechanism and effect of pulsed radiofrequency
Two types of radiofrequency lesioning are clinically used : conventional radiofrequency and PRF. PRF neuromodulation is nondestructive but can relieve pain by delivering an electrical field to the neural tissue14). While the effects of conventional radiofrequency thermal lesioning have a clear pathophysiological background in the destruction of nerve tissue and the subsequent blockade of pain transmission, the mechanism of PRF is still unknown. One theory to explain PRF suggests that a neuromodulatory effect occurs through changes in gene expression in pain processing neurons4,5,7). There are several advantages to using PRF for pain control. Firstly, PRF may provide long lasting pain relief with less side effects. Secondly, PRF can be repeated if the pain recurs since no tissue has been destroyed14). Thirdly, many published reports have revealed the efficacy of PRF for peripheral nerve lesions14). Thus, PRF is a promising treatment for patients with chronic pain refractory to conservative treatment.
CONCLUSION
We present the first known application of PRF neuromodulation for a case of SN. PRF neuromodulation of the saphenous nerve may offer an effective and low-risk treatment in patients with medically intractable SN or who are unwilling or unfit to undergo surgery. Further controlled prospective studies are necessary to evaluate the exact effects and long-term outcomes of this method.