INTRODUCTION
Developments in modern medicine have significantly increased life expectancy, and the resulting population aging means that neurosurgeons are being increasingly confronted with older patients suffering from lumbar spinal stenosis caused by degenerative changes of the lumbar spine3,7,19).
Surgery should be considered when conservative therapy fails to improve the symptoms of lumbar spinal stenosis, and decompressive laminectomy with or without fusion is the standard surgical treatment for patients with two-level or more lumbar spinal stenosis.
Two-level or more decompressive laminectomy with fusion effectively ensures spinal stability, but has significant adverse events, such as, postoperative complications, instrument failure, and adjacent segment degeneration (ASD). To avoid these adverse events, two-level or more decompressive laminectomy alone has been attempted for lumbar spinal stenosis18,20). However, decompression alone can provoke lumbar instability and aggravate symptoms after surgery.
Some reports have been issued on decompression alone for patients with single-level stenosis12,17,22), and on decompression alone in elderly patients9). However, comparative studies of decompression alone and fusion in elderly patients with two-level or more lumbar spinal stenosis were rare.
Accordingly, we retrospectively analyzed clinical, radiologic, and surgical outcomes following decompression alone or fusion in elderly patients with two-level or more lumbar spinal stenosis.
MATERIALS AND METHODS
Patients
Sixty patients, aged 65 years or older, who received multi-level (two-level or more) surgery at our Spine Center from June 2003 to December 2008 were selected for this study. Three spine surgeons participated in this study.
The clinical indications for surgery were radiating leg pain and/or neurogenic intermittent claudication (NIC) with or without low back pain resistant to conservative treatment. Magnetic resonance imaging (MRI) was used to confirm the diagnosis of central stenosis or lateral stenosis. The selection of surgical methods depends on each surgeon's clinical impression that which would elicit a better outcome, based on symptom, general condition, and the degree of osteoporosis. The degree of osteoporosis was evaluated by subjective judgment based on imaging study or by dual-energy X-ray absorptiometry (DEXA) if needed.
The general indications of decompression alone were patients with overwhelming main symptom of radiating pain or NIC rather than low back pain, patients who successful fusion was not expected due to severe osteoporosis, and patients with intolerable general condition to fusion surgery. Whereas, the general indications of fusion were patients with relatively severe low back pain suspected mechanical back pain due to degeneration without overt segmental instability, patients who successful fusion was expected due to tolerable bone marrow density, and patients with tolerable general condition to fusion surgery.
Patients with no choice but fusion surgery, for example, patients with overt segmental instability (defined by White and Panjabi23) or severe spondylolisthesis (grade II or more), were excluded. Other exclusion criteria included infectious disease, traumatic lumbar disease, developmental spinal deformities, metabolic bone disease, and tumors.
There were 27 men and 33 women, and overall mean age for surgery was 71.1 years (range, 65-84). Mean follow-up was 5.5 years (range, 3.0-9.0). Patients followed up for less than 3 years were excluded. Fifty patients underwent surgery at 2 levels, 8 at 3 levels, and 2 at 4 levels.
Outcome parameters
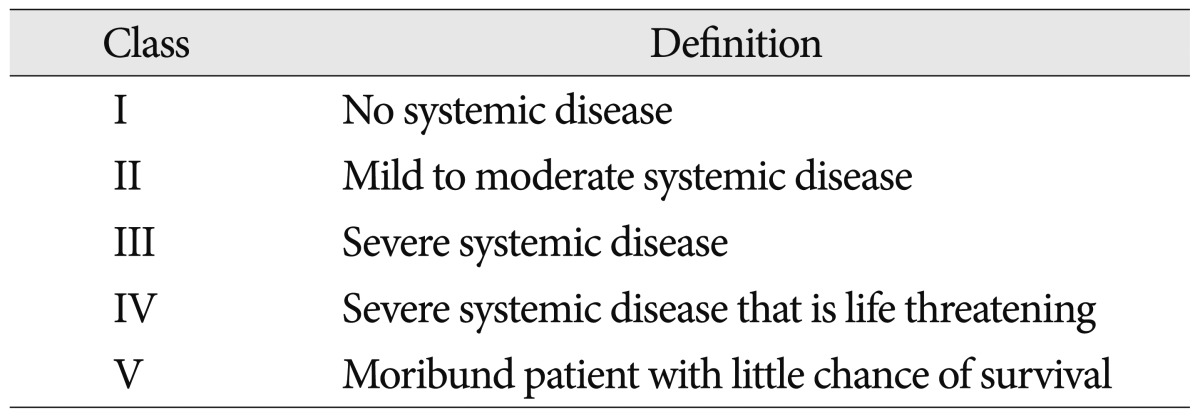
Preoperative conditions were assessed using the American Society of Anesthesiologists (ASA) classification of physical status (Table 1)8), and clinical outcomes were assessed using a visual analogue scale (VAS) for low back pain, a VAS for leg pain, the Oswestry Disability Index (ODI), and the Odom's criteria. VAS scores were determined using 0 to 10 point scales, where a score of 0 means symptom-free, and a score of 10 means the most serious symptom. VAS and ODI were scored preoperatively and at 6 weeks, 6 months, 1 year, and 3 years postoperatively. Odom's criteria were used to evaluate patient satisfaction at final follow-up.
Standard anterior-posterior and lateral radiographs of the lumbar spine were taken preoperatively and during follow-up for all patients. Lumbar lordotic angle was measured on a lateral radiograph in the neutral position using Cobb's method (Fig. 1). Preoperative and postoperative lumbar lordotic angles were compared at 6 weeks, 6 months, 1 year, and 3 years after surgery.
Surgical methods were compared with respect to estimated blood losses (EBL), operation times, and hospital stays. The occurrences of perioperative morbidities [e.g. neurologic deterioration, cerebrospinal fluid (CSF) leakage, wound infection, pneumonia, heart problem, urinary difficulty, epidural hematoma, and deep vein thrombosis] were checked. In addition, reoperation and developments of late postoperative complications (e.g. recurrence, instability, subsidence, screw looseing, non-union, and ASD) were documented.
Surgical technique
All operations were performed in the prone position. In cases of decompression alone, after a traditional median incision, partial laminectomy and decompressive ligamentectomy were performed at each symptomatic stenotic level. Unilateral foraminotomy, bilateral foraminotomy, or unilateral laminotomy and bilateral decompression were performed according to symptoms and MRI findings.
In cases of fusion, after decompression and discectomy, posterior lumbar interbody fusion (PLIF) or transforaminal lumbar interbody fusion (TLIF) was performed, and followed by two-level or more transpedicular screw fixation (percutaneous or open).
Statistical methods
SPSS version 16.0 (SPSS Inc., Chicago, IL, USA) was used to analyze all data. The chi square test, the independent 2-sample t-test, and the one-way analysis of variance were used depending on the characteristics of the variables being compared. Statistical significance was accepted for p values of <0.05.
RESULTS
Demographic and preoperative data
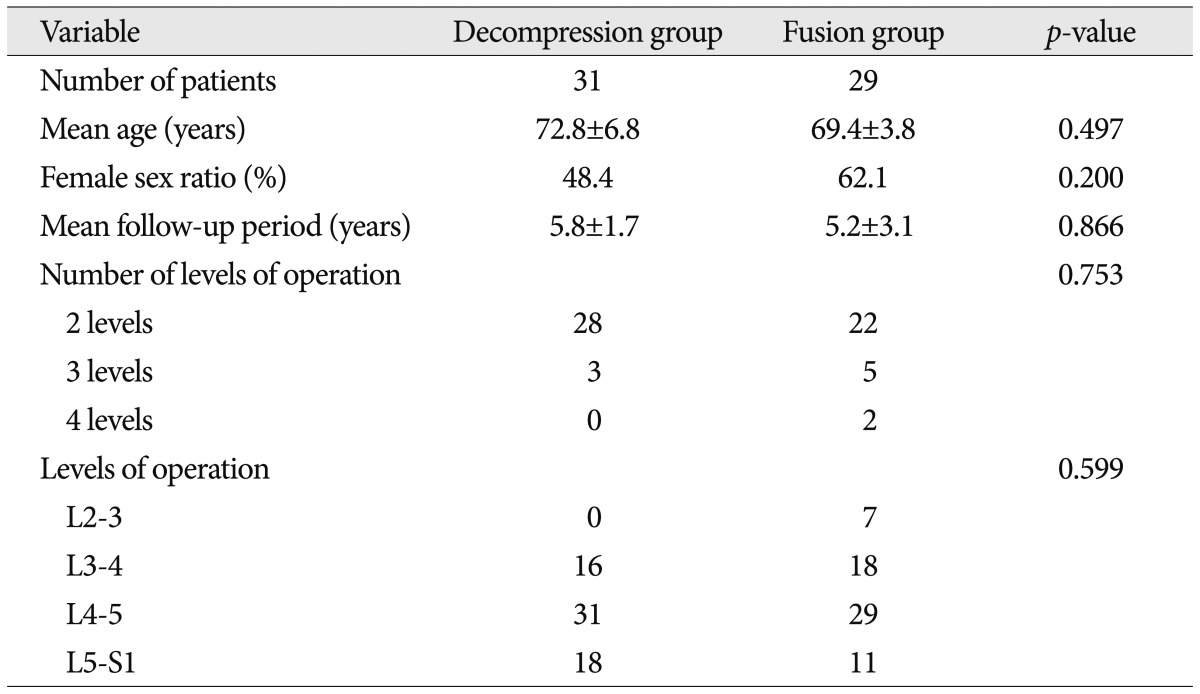
The patients were divided into two groups according to surgical technique. Of the 60 patients, 31 (51.7%) were allocated to the decompression group, and 29 (48.3%) to the fusion group.
No significant intergroup difference was found with respect to age, sex ratio, follow-up period, or surgical levels (Table 2). There was no significant difference with respect to ASA classification, preoperative ODI, or preoperative lumbar lordotic angle. Although there was no statistical significance, ASA classification tended to be worse in the decompression group, whereas preoperative ODI and lumbar lordotic angle tended to be worse in the fusion group. Also, unlike preoperative VAS for leg pain, preoperative VAS for low back pain of fusion group was higher than that of decompression group (p<0.05) (Table 3).
Unfortunately, the objective comparison of degree of osteoporosis was impossible because DEXAs were not evenly performed in the two groups.
Clinical outcome
In both groups, VAS for low back pain and leg pain was decreased during follow-up, sequentially.
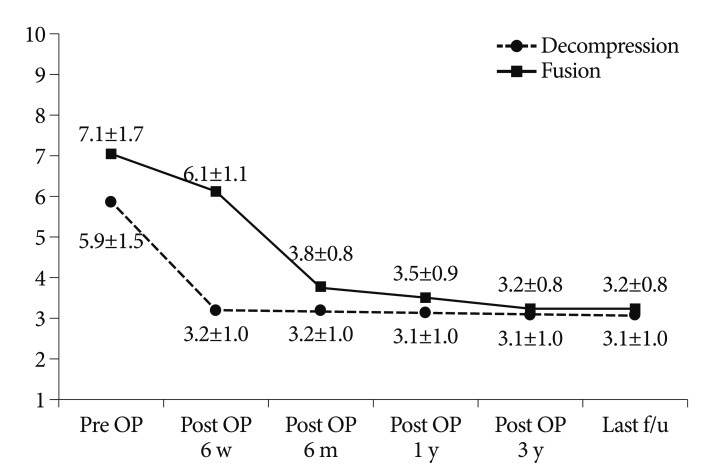
In decompression group, VAS for low back pain was improved from 5.9 to 3. 1 (p<0.05). Also, in fusion group, VAS for low back pain was improved from 7.1 to 3.2 (p<0.05) (Fig. 2).
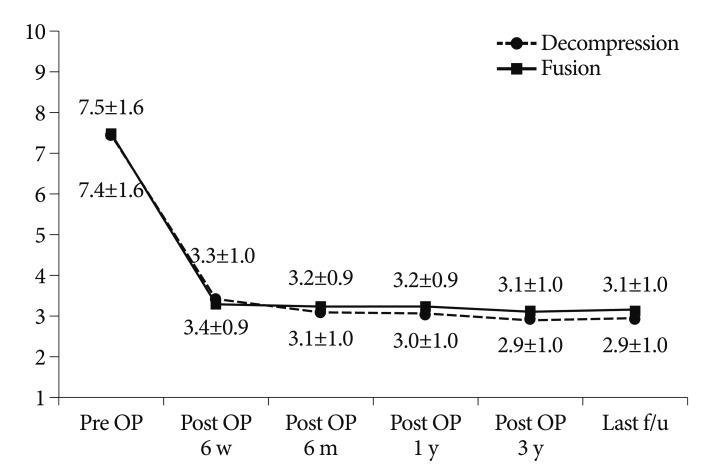
In decompression group, the mean preoperative VAS for leg pain of 7.4 decreased to 2.9 at last follow-up (p<0.05). Also, in fusion group, the mean preoperative VAS for leg pain of 7.5 decreased to 3.1 at last follow-up (p<0.05) (Fig. 3).
Follow-up VAS scores were not significantly different in two groups, but decompression group showed a better improvement in low back pain VAS scores at 6 weeks after surgery.
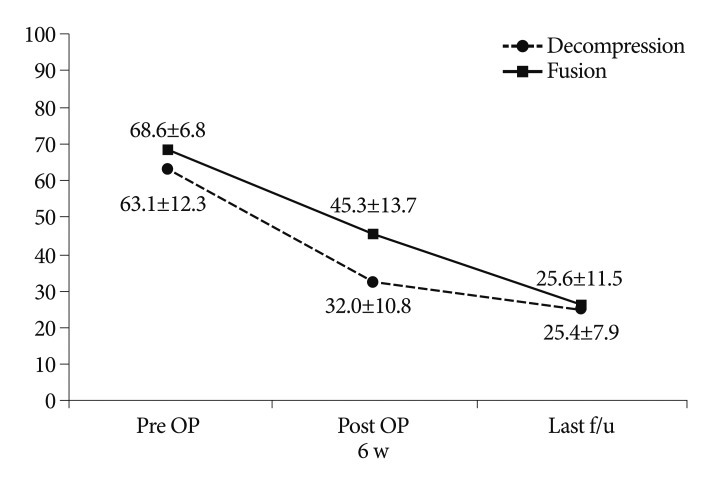
The functional aspects were evaluated using ODI scores. In both groups, ODI decreased during follow-up, sequentially (p<0.05). ODI scores were not significantly different in two groups (Fig. 4).
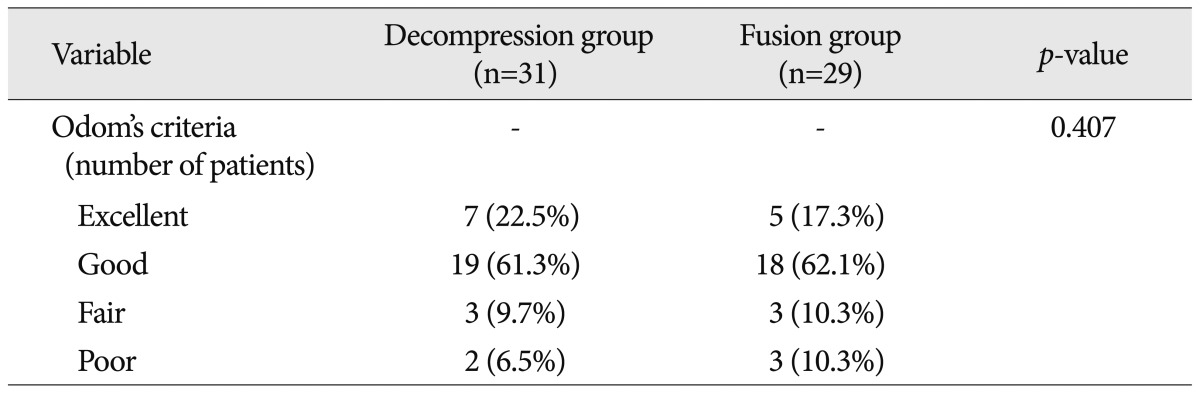
Odom's criteria failed to reveal a significant intergroup difference at last follow-up (Table 4).
Radiological outcomes
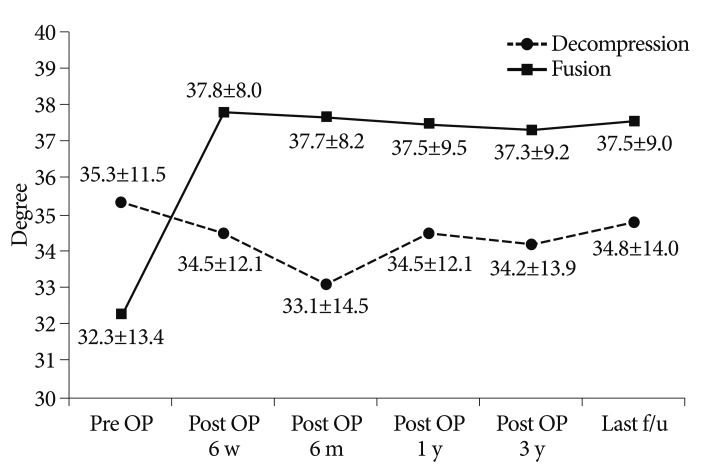
In decompression group, the mean preoperative lumbar lordotic angle of 35.3° decreased to 34.8° at last follow-up. However, the changes of angles were not significant.
On the other hand, in fusion group, the mean preoperative lumbar lordotic angle of 32.3° increased to 37.5° at last follow-up (p<0.05) (Fig. 5).
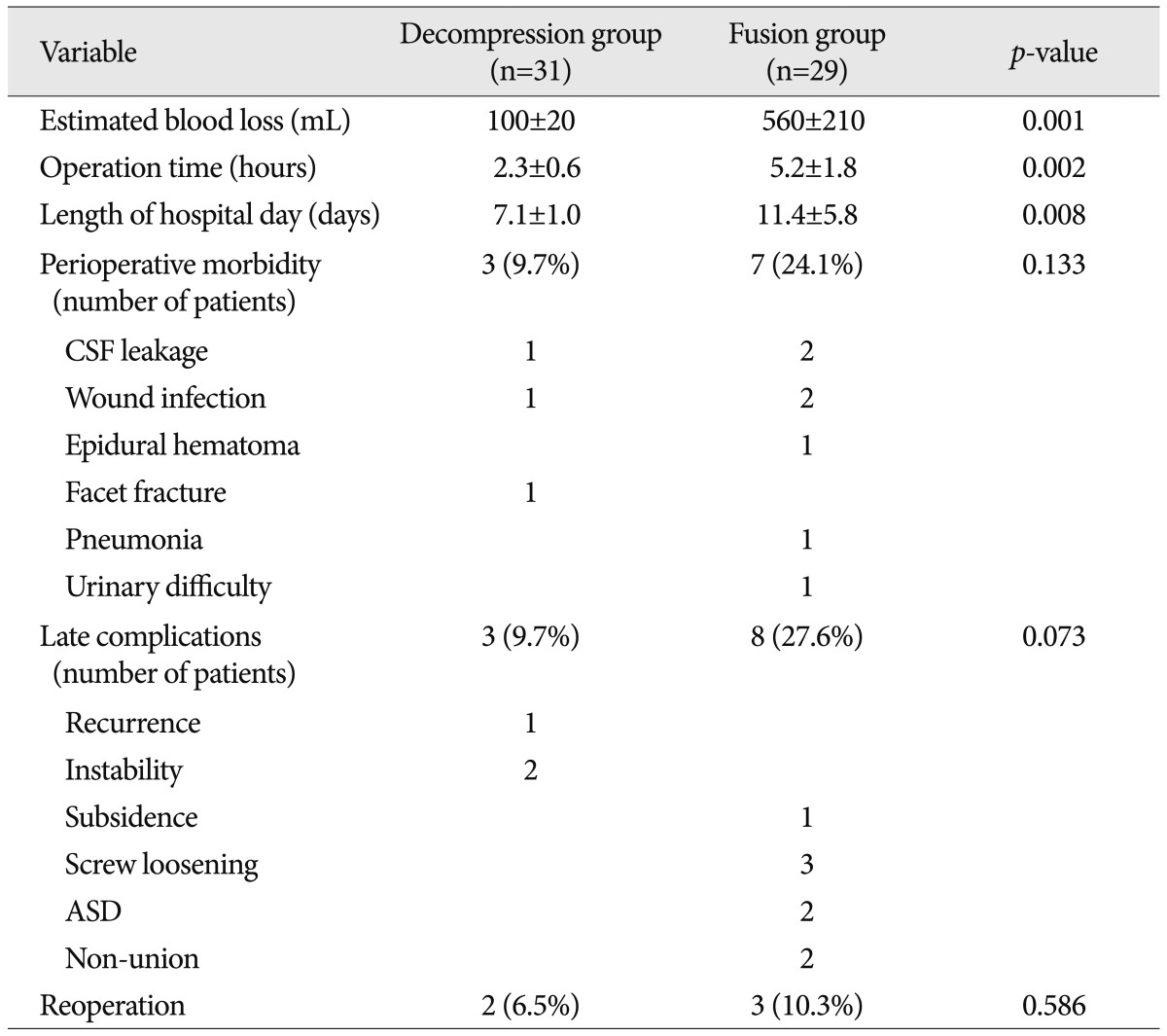
Comparison of surgical methods and complications (Table 5)
The EBL, operation time, and length of hospital stay were significantly better in the decompression group (p<0.05).
There was no postoperative mortality and no neurologic deterioration after surgery. Perioperative morbidity was noted in 3 patients (9.7%) in the decompression group, and in 7 patients (24.1%) in the fusion group. In decompression group, CSF leakage in 1 patient, wound infection in 1 patient, and facet fracture in 1 patient were occurred. In fusion group, CSF leakage in 2 patients, wound infection in 2 patients, epidural hematoma in 1 patient, pneumonia in 1 patient, urinary difficulty in 1 patient were found. Although there was no statistical significance, perioperative morbidities were more frequent in the fusion group.
In decompression group, 3 patients (9.7%) developed late complications (1 recurrence, 2 instability), and 2 patients (6.5%) underwent reoperation due to spinal instability and recurrence of symptoms with disc herniation. In fusion group, 8 patients (27.6%) developed late complications (1 subsidence, 3 screw loosening, 2 non-union, and 2 ASD) and fusion rate was 93.1%. Also, 3 patients (10.3%) underwent reoperation due to postoperative epidural hematoma, development of ASD, and fusion failure (Table 4). Although late complications were more frequent in the fusion group, it is not reasonable to compare the late complication rate between two groups because the items of complications are different.
DISCUSSION
The indications for decompressive surgery for two-level or more lumbar spinal stenosis are radiating leg pain or NIC resistant to conservative treatment. However, the appropriate surgical technique for treating two-level or more lumbar spinal stenosis remains controversial because the different surgical techniques (i.e., decompression alone or fusion) have their own unique advantages and disadvantages.
Spinal fusion has been performed on patients with severe spinal stenosis and instability to reduce the movement of the injured segment or to increase segment weight bearing ability2,4,10,13,16). Spinal fusion is known to relieve motion-induced discogenic pain and is biomechanically more stable than other procedures.
However, fusion also has its problems, such as, hardware failure, non-union, donor site pain, a protracted operation time, and invasiveness causing injury to paravertebral soft tissues which results in high perioperative morbidity15). In addition, fusion causes restricts motion by eliminating the functional mobilities of involved segments, and may increase biomechanical stresses on adjacent segments and lead to ASD14,21). Furthermore, two-level or more fusion is likely to cause more ASD than single-level fusion, therefore, selection of fusion should be carefully considered in cases of two-level or more lumbar spinal stenosis6).
To prevent these problems associated with fusion, decompressive laminectomy alone has been adopted by many surgeons. Decompressive laminectomy alone can minimize tissue injuries, shorten operation times, reduce perioperative morbidity, and prevent instrument-related complications. Some surgeons have reported that decompressive surgery alone in single-level spinal stenosis produces good results5,12,17,22), and other have reported that old age does not increase morbidity associated with decompressive surgery alone in lumbar spinal stenosis9,11,19).
However, the stability, safety, and efficacy of decompression without fusion are somewhat controversial. Two-level or more decompression alone has a risk of lumbar instability after surgery. In a meta-analysis, some authors found that 69% of patients treated with decompression alone for lumbar spinal stenosis experienced a favorable outcome, as compared with 90% of those treated with fusion1).
The present study demonstrates that the postoperative total lumbar lordotic angles increased significantly in the fusion group, which indicates in terms of the correction of lumbar lordosis, fusion is better than decompression alone. However, in our decompression group, decreases in lumbar lordotic angles were not significant, and aggravations of instability were uncommon (only 2 of 31 patients). These results suggest two-level or more laminectomy does not normally cause instability, and that preoperative mild instability is not normally aggravated after surgery. In old age groups, these findings are probably due to the spinal stability conferred by age-related changes of discs and facet joints.
In fact, many authors have reported that the corrections of lumbar lordosis have not been well correlated with clinical outcomes15,17,24). In this study, irrespective of radiological outcome, clinical outcomes, as determined using VAS and ODI scores and Odom's criteria, were not significantly different between our two groups, except low back pain VAS scores at 6 weeks after surgery (i.e., in the short-term). This slow improvement of low back pain in fusion group was probably due to the greater retraction and more severe injury of soft tissues.
In the viewpoint of comparison of each surgical method, EBL, operation time, and hospital stay of decompression group was obviously better than that of fusion group. As a result, although no significant difference in preoperative general conditions was found between the two groups, perioperative morbidities were more frequent in the fusion group. We attribute these differences to more blood loss, longer anesthesia time, more transfusion, and more fluid infusion in fusion group.
The selection of decompression alone or fusion depends on numerous factors, such as, symptoms, age, general condition, the presence of osteoporosis, the number of segments involved, the presence of instability, and surgeon's preference. The most important factor, during the selection process for two-level or more lumbar spinal stenosis, is radiographic instability of the lumbar spine, because fusion is the treatment of choice in overt instability. However, in mild or equivocal instability, the selection of fusion is sometimes worrisome. For example, in elderly patients or those with a poor general condition who is vulnerable to major surgery, protracted surgery, heavy bleeding, and extensive soft tissue injury can cause severe perioperative morbidities, such as, cardiopulmonary complications, wound infections, or even death. Also, in patients with osteoporosis, transpedicular screw fixation or interbody fusion can cause instrument-related complications, such as, subsidence, screw failure, or non-union. Accordingly, decompression alone can be the better choice for patients with two-level or more lumbar spinal stenosis with an advanced age, a poor preoperative condition, or osteoporosis, if there is no severe instability.
Our study has some limitations however. First, since it limited by its retrospective nature, surgical indications in the two study groups were not precisely the same. In particular, patients in fusion group had worse preoperative symptom including low back pain and lumbar lordotic angle, and better preoperative general condition. Second, surgical techniques were not separated in each group (i.e., unilateral or bilateral laminectomy in decompression group, PLIF or TLIF, and percutaneous or open screw fixation in fusion group). Surgical techniques were applied in varying depending on the type of stenosis, and these differences could affect the results. Third, three spinal surgeons were involved in this study, and difference between surgical techniques could have influence outcomes. Finally, the lack of long-term clinical follow-up is a concern, because the risk of symptoms recurrence is generally assessed over 5 years after surgery24).
CONCLUSION
Although the correction of lumbar lordotic angle was better in fusion group, clinical outcomes were not significantly different in the two groups. Moreover, perioperative morbidities and late complications were better in the decompression group. We suggest that decompressive laminectomy alone to be considered rather than fusion, if there is no overt instability, for patients with two-level or more lumbar spinal stenosis, and especially for elderly patients with a poor general condition or osteoporosis.