Single-Stage Posterior Subtotal Corpectomy and Circumferential Reconstruction for the Treatment of Unstable Thoracolumbar Burst Fractures
Article information
Abstract
Objective
To illustrate the technique of single-stage posterior subtotal corpectomy and circumferential reconstruction for the treatment of unstable thoracolumbar burst fractures and to evaluate the radiographical and clinical outcomes of patients treated using this technique.
Methods
16 consecutive patients with unstable thoracolumbar burst fractures were treated with single-stage posterior subtotal corpectomy and circumferential reconstruction. The mean patient age was 54.8 years. The mean follower up period was 25 months. Five patients suffered from T12 fractures, 10 from L1, 1 from L2. The segmental kyphosis, neurologic status, visual analogue scale for back pain was evaluated before surgery and at follow up.
Results
The segmental kyphotic angle improved from 18.5 degrees before surgery to -9.2 degrees at the last follow up. The mean correction angle was 28.9 degrees. The mean surgical time was 255 minutes, and a mean intraoperative blood loss was 1073 mL. Intraoperative complications included two dural tears, and a superficial wound infection. There were no other severe complications. The mean visual analog scale of back pain decreased from a mean value of 6.6 to 2 at the last follow up.
Conclusion
The single-stage posterior subtotal corpectomy and circumferential reconstruction achieved satisfactory kyphosis correction with direct visualization of the circumferentially decompressed spinal cord, as well as good fusion with less blood loss and complications. It is a safe and reliable surgical treatment option for unstable thoracolumbar burst fractures.
INTRODUCTION
Burst fractures are compression fractures of the anterior and middle portions of the spinal column in which vertebral body fragments to shift into the spinal canal1516). These fractures can cause neurologic complications and kyphotic deformity.
Patients with unstable burst fractures typically require surgery to relieve pain, to address neurologic deficits, and to stabilize the spine19). Common surgical options include posterior approach, anterior approach, and combined anterior-posterior approach461221263339). Each technique has advantages and disadvantages. Then, the optimal approach remains controversial1721).
Some reports have described posterior reconstruction using pedicle screws, aiming to reposition canal-compromising fragments by ligamentaxis or remodeling of the canal52436). Posterior surgeries of this type for thoracolumbar burst fractures have reported satisfactory results in fractures involving mild instability38). Conversely, McCormack et al.27) proposed that highly unstable spine fracture with load-sharing scores (LSS) ≥7 should be treated by anterior column reconstruction. For highly unstable thoracolumbar burst fractures, anterior decompression and reconstruction has been developed with a variety of anterior implant systems, which have achieved satisfactory results2133).
Currently, based on the biomechanical date, combined anterior-posterior approach can provide the most stable biomechanical stabilization of three columns for unstable thoracolumbar burst fracture12341). However, the extensive surgical procedures, including the anterior approach, may increase the morbidity, especially with traumatized thoracic or peritoneal cavities928343540). Theoretically, stabilization of three columns through a posterior approach would avoid these risks, shortcomings, and facilitate rehabilitation. Recently, authors have reported their experience with similar methods8).
The aim of this study was to illustrate the technique of single-stage posterior subtotal corpectomy and circumferential reconstruction for the treatment of unstable thoracolumbar burst fractures with LSS ≥7 and to evaluate the radiographical findings and clinical outcomes of patients treated using this technique.
MATERIALS AND METHODS
Patients
Between February 2012 and February 2014, 16 patients with acute traumatic fractures at thoracolumbar junction were included in this prospective study.
All patients with load sharing scores ≥7 were treated with single-stage posterior subtotal corpectomy and circumferential reconstruction132738).
This study was conducted with approval from the Ethics Committee of our Hospital.
There were nine males and seven females with an average age at the time of operation of 54.8 years (range 23–73 years). The mean follow up period was 25 months (range 12–32 months).
Five patients suffered from T12 fractures, 10 from L1, 1 from L2. Neurologic deficit was assessed using The American Spine Injury Association (ASIA) impairment scale. The ASIA impairment scale was A in 1 patient, B in 2, C in 3, D in 4, and E in 6.
Operative technique
All procedures were performed using somatosensory evoked potential monitoring. Following endotracheal intubation, patients were placed in a prone position on a radiolucent operation table.
A posterior midline incision was made spreading from two or three levels above the fracture site to two or three levels below it, and subperiosteal dissection performed from the spinous process to the tip of the transverse process at all predetermined levels.
With C-arm guidance, pedicle screws were inserted two level below and above the fracture site or three levels in patients with severe osteoporosis or patients with translational or rotational injuries combined with posterior ligamentous complex disruption.
The single-stage posterior subtotal corpectomy was then performed (Fig. 1).

Preoperative and postoperative imaging of a 49-year-old male patient with L1 burst fracture. A : Preoperative lateral supine roentgenogram showing a L1 burst fracture with an angular segmental deformity of 35°. B and C : Preoperative sagittal and axial lumbar magnetic resonance imaging demonstrating a significant spinal canal encroachment by retropulsion of the fragments of the fracture vertebra. D and E : Photograph (D) and postoperative axial CT showing circumferential spinal canal clearance and anterior-lateral wall of vertebral body restored. F and G : Postoperative standing AP and lateral radiograph showing a correct position of the mesh cage and normal thoracolumbar alignment. Angular deformity was corrected and segmental height was restored. AP : anteriorposterior.
Posterior elements of the fractured level are removed. With dura mater on sight, both lamina of the fractured vertebra are completely removed. Facet joint of more severe injured side is then removed to reveal nerve root and dorsal root ganglions. Epidural veins and radicular veins are cauterized with bipolar forceps to avoid massive bleeding. These steps decompress the posterior aspect of the thecal sac. After that, for reduction of the segmental height, a rod is applied to the side of the vertebra with the facet joint still intact. Once these are done, the thecal sac can be easily retracted to provide better exposure of the posterior portion of the fractured vertebral body and the intervertebral discs. The thecal sac and nerve root are then gently retracted and protected with a nerve retractor. A subtotal corpectomy of the fractured vertebral body is performed with a high-speed drill and osteotome and curette leaving lateral and anterior vertebral body wall. The posterior wall, superior and inferior end-plates of the fractured vertebral body are then broken down using a curved curette and the pieces are removed with pituitary. The discectomies are performed to provide sufficient space for cage. During this process, under fluoroscopy, a probe was used to check the depth of bone resection.
The appropriate size of cage is confirmed and the cage is pinned to the cage holder. The interior of the device is packed with resected local bone and allograft bone.
By gently distracting the thecal sac and nerve root, we insert a cage into the corpectomy cavity.
Using an impactor, the cage is shifted as necessary so that it is positioned exactly at the midline and in the anterior of the corpectomy cavity. Cage positioning can be monitored during all stages of implantation using posteroanterior and lateral fluoroscopy. Once proper placement is confirmed, additional bone graft tissue is packed around the cage and posterolateral sides of the column for the circumferential fusion.
Postoperatively, the patients were allowed out of bed using a customized thoracolumbar orthosis 24 hours after surgery. The orthosis was used for 3 months.
Radiologic evaluation and clinical assessments
Preoperative anteriorposterior and lateral radiographic images were obtained to evaluate each fracture and degrees of segmental kyphosis. Computed tomography scanning and magnetic resonance imaging was done before surgery to assess for signal abnormalities in the spinal cord and other soft tissues (for e.g., indications of a tear in the interspinous or posterior longitudinal ligament).
The kyphotic angle was measured on lateral radiographs using the Cobb method. Regional angles (RAs) between the superior endplate of the vertebral body above the affected level and the inferior endplate of the vertebral body below the affected level were measured preoperatively, immediately after surgery, and at the final follow up (Fig. 2).

The kyphotic angle was measured on lateral radiographs using the Cobb method. Regional angles (RAs) between the superior endplate of the vertebral body above the affected level and the inferior endplate of the vertebral body below the affected level were measured preoperatively (A) and after surgery (B).
Radiologic assessment of fusion at follow up was based on the presence of trabecular bone bridging at the fracture site, or no motion (less than 3°) in lateral dynamic views (Fig. 3).
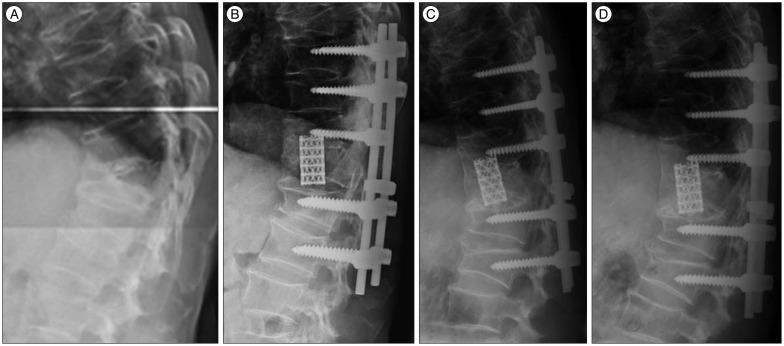
A lateral radiographs of a 72-year-old male with T12 burst fracture (A). He was treated using the single-stage posterior subtotal corpectomy and circumferential reconstruction. A postoperative lateral radiograph showed good sagittal alignment (B). During a visit to 18 months after surgery, lateral flexion (C) and extension (D) dynamic radiographs showed bony fusion at the fracture site.
Surgical time, operative blood loss, functional improvement, and complications, including intraoperative and early postoperative events, were assessed by chart review. Clinical outcome was analyzed using a visual analogue scale (VAS) for back or radicular pain. The ASIA impairment scale for neurological deficit was used before surgery and at follow up.
Statistical analysis
The PACS system (π view®, Infinitt, Seoul, Korea) was used by two independent observers for the measurement. The intraobserver and interobserver agreement rate and k values were obtained to check errors between 2 observers. For statistical analysis, the SPSS 17.0 was used and the p-value less than 0.05 were considered significant.
RESULTS
The interobserver agreement rate was 94% (mean k=0.75), and intraobserver agreement rate was 97% (mean k=0.81). The intraobserver and interobserver error analyses showed good agreement.
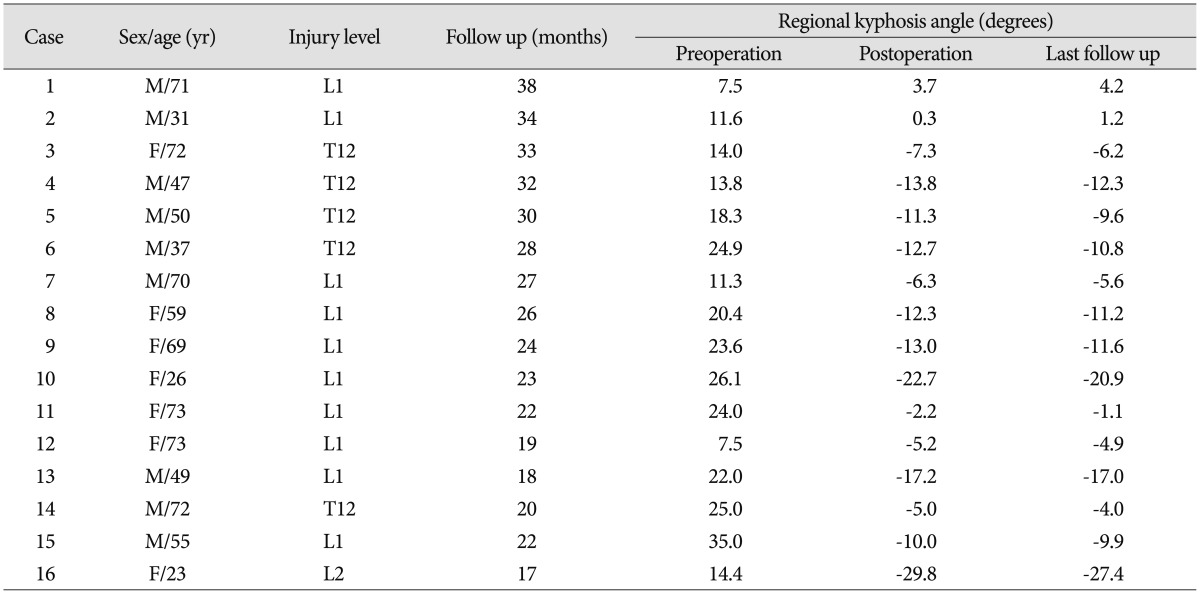
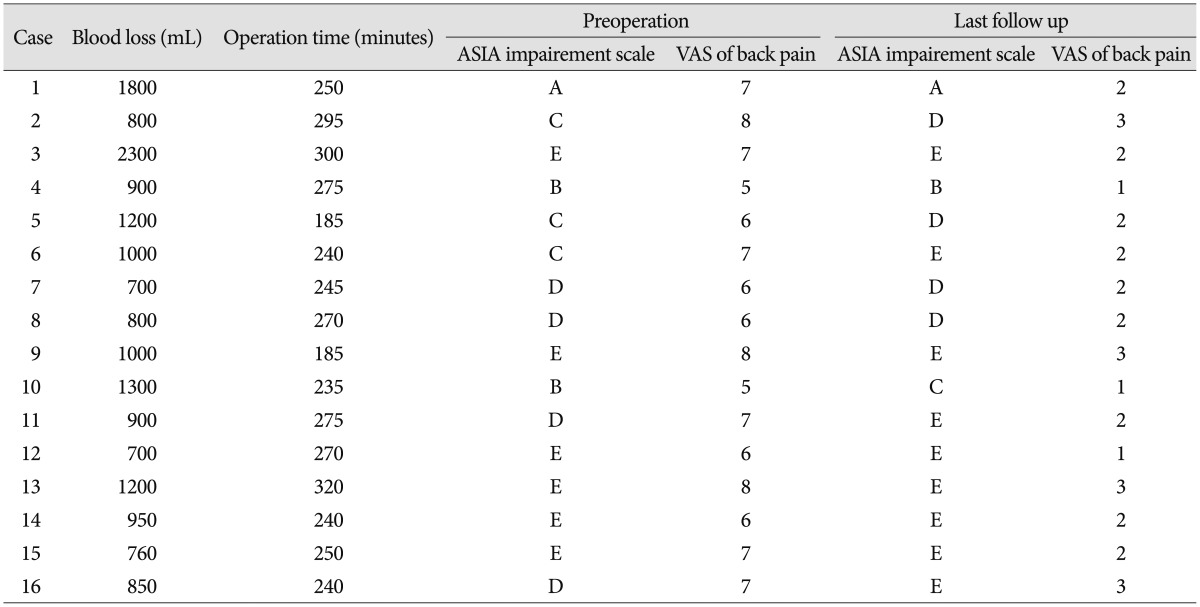
The average preoperative RA was 18.5±7.7 degrees (range, 7.7–35.2 degrees). Immediately after the operation, the average RA was -10.3±8.5 degrees (range, -30.1–3.5 degrees), and it was -9.2±8.0 degrees (range, -27.4–4.1 degrees) at the last follow up. The average correction angle was 28.9±13 degrees (range, 3.7–48.2 degrees). The difference in average preoperative and postoperative RA was statistically significant (p=0.024). No obvious correction loss was noted at the last follow up (Table 1).
The mean surgical time was 255 minutes (range, 185–300 minutes), with a mean intraoperative blood loss of 1073 mL (range, 700–2300 mL) (Table 2). Intraoperative complications included two dural tears, and one superficial wound infection. All dural tears were repaired primarily and did not result in adverse sequelae. The superficial wound infection successfully treated with debridement, primary closure over drains, and antibiotic therapy. There were no other severe complications.
The mean VAS of back pain decreased from a mean value of 6.6±1.0 (range, 5–8) preoperatively to 2±0.7 (range, 1–3) at the last follow up (p=0.001) (Table 2).
Some patients had an improvement in their neurological functions after surgery. The ASIA impairment scale was A in 1, B in 1, C in 1, D in 4, and E in 9 at the last follow up. The preoperative ASIA impairment scale was B in two patients, one of whom was restored to ASIA C. The preoperative ASIA impairment scale was C in three patients, these patients were restored to ASIA D or E. The preoperative ASIA impairment scale was D in four patients, two of whom were restored to ASIA E (Table 2).
All patients achieved bony fusion, which was confirmed based on the presence of trabecular bone bridging at the fracture site using radiographic evaluations including lateral dynamic views (Fig. 3).
DISCUSSION
The goals of surgical treatment for unstable thoracolumbar burst fractures are to restore vertebral body height, correct angular deformity, decompress neural tissue, allow rapid mobilization and rehabilitation, decrease the complications of prolonged immobilization, prevent development of progressive deformity with neurologic deficit, and limit the number of instrumented vertebral motion segments23461011122021).
A large number of articles have been published describing techniques for the reduction and stabilization of these fractures, including posterior fixation, stand-alone anterior approach fixation, and combined anterior-posterior approach461221263339). Each surgical treatment has advantages and disadvantages1729).
In practice, the management of each patient should be individually based on a variety of clinical and radiologic factors, including the presence of neurologic deficit, fracture type, location of the injuries, deformity angulation, residual canal diameter, vertebral body height and nonspinal factors, such as age and medical comorbidities1930).
In cases of unstable thoracolumbar burst fracture with compression of neural elements or load sharing scores ≥7, anterior decompression with anterior instrumentation provides good exposure for direct decompression of the spinal canal, facilitates good reconstruction of the anterior and middle portions of the spinal column. Solely anterior approaches are indicated in cases where the posterior longitudinal ligament and posterior column is intact38). However, the operative risk is higher than that associated with posterior approaches16).
Traditionally the standalone posterior approach is the optimal in case of the posterior ligamentous complex injury, but it can only indirectly reduce a fractured vertebral body, and the means of augmenting the anterior column are limited19). Reported loss of reduction caused by insufficient anterior column support with or without hardware failure is not uncommon4724).
A combined anterior and posterior approach is the optimal for patients who have incomplete spinal cord damage, disrupted posterior ligamentous complex or translation injuries where anterior decompression or stabilization is required38). Although the anterior approach provides good spinal cord decompression and allows for good vertebral column reconstruction, it may not resist further destructive flexion forces when the posterior ligaments have been rendered incompetent. Therefore, a combined surgical approach is appropriate for the purpose of reconstructing the tension bond14).
Although the combination of anterior and posterior approach can provide the most stable biomechanical repair, the operation time, complication and morbidity rate might be apparently higher than that of the single approach.
Recently, single-stage posterior corpectomy and replacement with various types of cage followed by pedicle screw instrumentation for unstable thoracolumbar burst fractures have been reported81832). Ayberk et al.8) and Sasani et al.32) have reported 8 and 14 cases of thoracolumbar burst fracture treated by the similar approach. The clinical outcomes were satisfied. They proposed that a single-stage posterior approach may be preferable to the combined anterior-posterior approach and that this procedure is associated with fewer complications than the traditional combined approach. Haiyun and Ozer18) reported a similar three-column reconstruction of thoracolumbar fracture above L2 through a single posterior approach with mesh cages and pedicle screws.
Instead of expandable cage as Ayberk et al.8) and Sasani and Ozer32) described, Haiyun et al.18) used nonexpandable cage to reconstruct anterior and middle column.
They noted that use of an adequate shorter nonexpendable cage can provide sufficient biomechanical stability and has benefits in the treatment of thoracolumbar burst fractures.
Using an expandable cage allows easier restoration of body height than use of a nonexpandable cage or strut bone. However, shortening reconstruction for unstable burst fracture with a shorter nonexpandable cage appears to offer two advantages : 1) the shorter nonexpandable cage can be easily inserted into the anterior part. By posterior compression, this maneuver did not affect the correction of kyphotic deformity. The shortening is from 0 to 5 mm (0–7.01%), which is within the safe range37). 2) acute spinal column shortening within the safe range increases spinal cord blood flow, which is important for recovery of spinal cord function22). Therefore, no significant difference was found between the biomechanical properties of expandable and nonexpandable cages31). According to above reason, we used nonexpandable cage to reconstruct anterior and middle column in our cases.
Compared with stand-alone anterior or posterior approach, single-stage posterior subtotal corpectomy and circumferential reconstruction can not only decompress the canal anteriorly but also decompress and repair neural elements posteriorly at same time. Anterior cage can significantly decrease the load over the posterior fixation system and avoid the loosening or fatigue fracture of screws, reduce the loss of the interbody height, prevent secondary kyphotic deformity. In addition, with the help of intact anterior longitudinal ligament and anterolateral wall of vertebral body that can form a protective band to strengthen the fixation against hyperextension and rotation force, single-stage posterior subtotal corpectomy and circumferential reconstruction can provide stiffer fixation mechanical24).
However, our study is by no means suggesting that the single-stage posterior subtotal corpectomy and circumferential reconstruction should be the preferred treatment over other techniques; it is merely one of the surgical options. Our study had limitations, including a small sample size, a short follow up period in some of the patients, and the lack of a comparative study group. The more in-depth analysis and large number cases are needed.
CONCLUSION
The single-stage posterior subtotal corpectomy and circumferential reconstruction might be a safe and reliable surgical treatment option for unstable thoracolumbar burst fractures with load sharing scores ≥7. Because it provides effective circumferential spinal canal decompression in case of a neurologic deficit, complete kyphosis correction and maintenance of kyphosis correction, absence of risk carried by the anterior approach, facilitation of the placement of anterior and posterior fixation devices using only one approach, preservation of the anterior longitudinal ligament, repair of dural tears at the posterior side, less complications, and rigid enough biomechanical.