Real-World Impact of Modern Reperfusion Therapy for Acute Ischemic Stroke : A Nationwide Population-Based Data Study in Korea
Article information
Abstract
Objective
The treatment paradigm for acute ischemic stroke has undergone several major changes in the past decade, contributing to improved patient prognosis in clinical practice. However, the extent to which these changes have affected patient prognosis in the real-world is yet to be clarified. This study aimed to evaluate the real-world impact of modern reperfusion therapy for acute ischemic stroke using data from the National Health Insurance Service in Korea.
Methods
This study included patients aged 18–80 years who were admitted via the emergency room with an I63 code between 2011 and 2020. The rates of intravenous thrombolysis use and endovascular treatment according to the year of admission were investigated. Furthermore, the rates of decompressive craniectomy and 3-month mortality were also analyzed. The 10-year observational period was divided into three periods based on the 2015 guideline change as follows : prior, 2011–2014; transitional, 2015–2016; and modern, 2017–2020.
Results
A total of 307117 patients (mean age, 65.7±10.9 years) were included, and most patients were male (59.7%). The rate of endovascular treatment gradually increased during the study period from 0.71% in the prior period to 1.32% in the transitional period and finally to 1.85% in the modern period. Meanwhile, the 3-month mortality rate gradually decreased from 4.78% in the prior period to 4.03% in the transitional period and to 3.71% in the modern period.
Conclusion
In Korea, the mortality rate decreased as the rate of modern reperfusion therapy increased in patients with acute ischemic stroke. Overall, technical and scientific advances in reperfusion therapy have improved the outcome of patients with acute ischemic stroke in Korea.
INTRODUCTION
Changes in the treatment paradigm for reperfusion therapy for acute ischemic stroke have made a significant difference in clinical practice. Following the change to guidelines in 2015, it was essential for medical institutions to create an environment to proceed with emergent neurointervention for acute ischemic stroke patients [19]. Reperfusion therapy for acute ischemic stroke started with the use of tissue plasminogen activator in the mid-1990s, after the Food and Drug Administration approved its use in the United States [14]. However, drug availability has increased as the time window for intravenous thrombolysis (IVT) administration has also increased, from 3 to 4.5 hours, and age restrictions have been abandoned [4,6,26].
Endovascular reperfusion therapy started with the MERCI Retrieval System and Penumbra device in the 2000s, but failed to prove the efficacy [18,24]. However, five landmark randomized controlled studies published in 2015 demonstrated the effect of mechanical thrombectomy [2,3,5,7,20]. The indications for endovascular treatment have recently expanded to include the late-onset period, medium vessel occlusion, and large ischemic core [1,15,17,27]. These changes have occurred worldwide, including in Korea. However, the extent to which this sudden change in treatment paradigms has affected patient prognosis in the real-world is yet to be clarified.
Thus, the purpose of this study was to evaluate the realworld impact of modern reperfusion therapy on the prognosis of patients with acute ischemic stroke in Korea, using National Health Insurance Service (NHIS) data. We hypothesized that the increase in the use of modern reperfusion therapy would lead to a decrease in the rates of mortality and decompressive craniectomy surgery in patients with acute ischemic stroke.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Uijeongbu Eulji Medical Center (No. 2021-08-014) and was conducted according to the tenets of the Declaration of Helsinki.
Study design and patients
This was a nationwide retrospective observational study using NHIS data in Korea. The NHIS is a single insurer managed by the Korean government, and its database stores medical information, including diagnoses, procedures, surgeries, and drug prescriptions, of all 50 million citizens, collected from reimbursement claims data [11,25]. In this study, data were obtained from the NHIS under a confidentiality agreement for restrictive use of the data.
We identified patients with acute ischemic stroke aged 18–80 years who were admitted via the emergency room between January 2011 and December 2020 at general or tertiary general hospitals with a capacity of >100 beds. The patients were identified using the I63 disease code, which is the code for ‘cerebral infarction’. The exclusion criteria were as follows : admission through outpatient clinics or hospitals with <100 beds, and a second stroke during the study period. The use of IVT in patients with acute ischemic stroke was limited to those aged <80 years until December 2018, after which it became available for all ages. Therefore, patients aged >80 years were also excluded from the main study; however, given the trend of an increased incidence of acute ischemic stroke in elderly patients, the results of the evaluation of those aged >80 years are provided separately as Supplementary Table 1, Supplementary Fig. 1 and 2.
Variable definition
Data on prescriptions, such as IVT, endovascular treatment, and surgical procedures, during the admission period were reviewed. IVT was defined as the prescription of tissue plasminogen activator during the admission period. Endovascular treatment was defined as the prescription of an endovascular treatment (M6631, M6633, M6630, M6635, M6636, and M6637; Supplementary Dataset 1) during the admission period. Craniectomy was identified using surgical prescription codes (N0331, N0332, N0333, S4621, S4622, and S4780; Supplementary Dataset 1) during the admission period. Mortality was defined as death within 3 months after the admission date. The rates of IVT, endovascular treatment, craniectomy, and mortality were calculated yearly from the admission date of 2011 to 2020.
Subgroup analysis by time period and hospital scale
The 10-year observation period was divided into three periods reflecting the time of the 2015 guideline change as follows : prior period, 2011–2014; transition period, 2015–2016; and modern period, 2017–2020. Hospitals were divided into tertiary general hospital and non-tertiary general hospital according to their size and quality of care provided, which were evaluated every 3 years by the Ministry of Health and Welfare. Tertiary general hospital is an approved hospital that meet the condition of Ministry of Health and Welfare which is specialized in severity of disease. Non-tertiary general hospital is a center with 100 or more beds with basic medical department.
Statistical analysis
Descriptive data are reported as the mean±standard deviation for continuous variables and as frequency (percentage) for categorical variables. Statistical comparisons of the use of IVT, endovascular treatment, craniectomy, and mortality rates among the observation years were performed using the analysis of variance and Kruskal-Wallis test. All statistical analyses were performed using Software Enterprise (version 7.1; SAS Institute Inc., Cary, NC, USA) and R Studio (version 4.0.5; R Foundation for Statistical Computing, Vienna, Austria). Statistical significance was set at p<0.05.
RESULTS
Patient characteristics
A total of 307117 patients were included. The characteristics of the study population are summarized in Table 1. The mean patient age was 65.7±10.9 years, and majority of the patients were male (59.7%). Tertiary general hospitals accounted for 24.2% of admitting institutions.
Trend in reperfusion therapy and mortality
The overall number of patients with acute ischemic stroke aged 18–80 years substantially decreased over time, especially among women. Fig. 1 displays the rates of IVT use, endovascular treatment, craniectomy, and mortality according to the year of admission. The use of IVT steadily increased from 1.37% in 2011 to 2.54% in 2020. The endovascular treatment rate also showed a steady increase between 2011 and 2014, and the slope increased between 2015 and 2020. The annual rate of craniectomy showed no significant differences during the study period. Meanwhile, the annual mortality rate gradually decreased from 5.18% in 2011 to 3.75% in 2020.
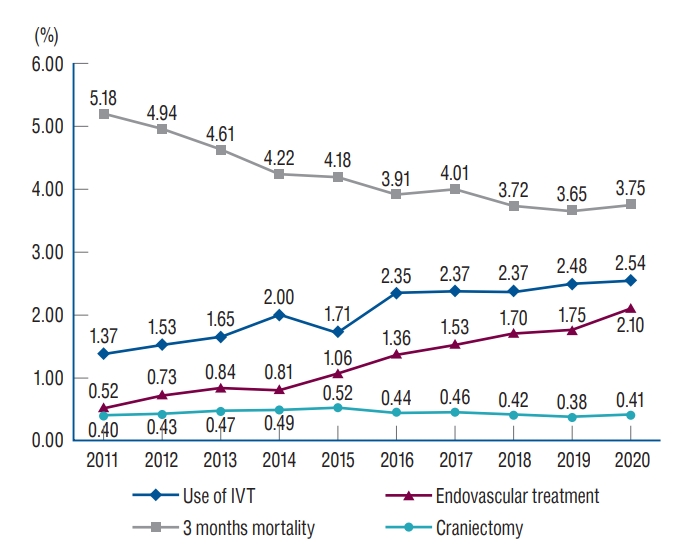
Annual trends in reperfusion therapy, craniectomy, and mortality among patients with acute ischemic stroke aged 18–80 years. IVT : intravenous thrombolysis.
Regarding trends in the three defined periods (Fig. 2), the mortality rate was decreased in the modern period (2017–2020), at 3.71%, from 4.78% in the prior period (2011–2014), ref lecting a decrease of approximately 22.4% (p<0.001). Meanwhile, the endovascular treatment rate was increased during the modern period (1.85%) from 0.71% during the prior period, reflecting a 2.61-fold increase. The rate of craniectomy showed a decreasing trend from 0.45% in the prior period to 0.40% in the modern period.
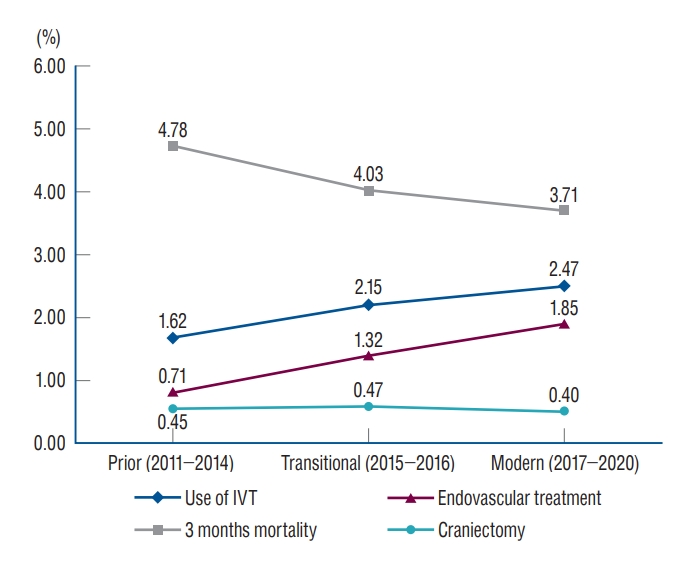
Trends in reperfusion therapy, craniectomy, and mortality according to the study period among patients with acute ischemic stroke. IVT : intravenous thrombolysis.
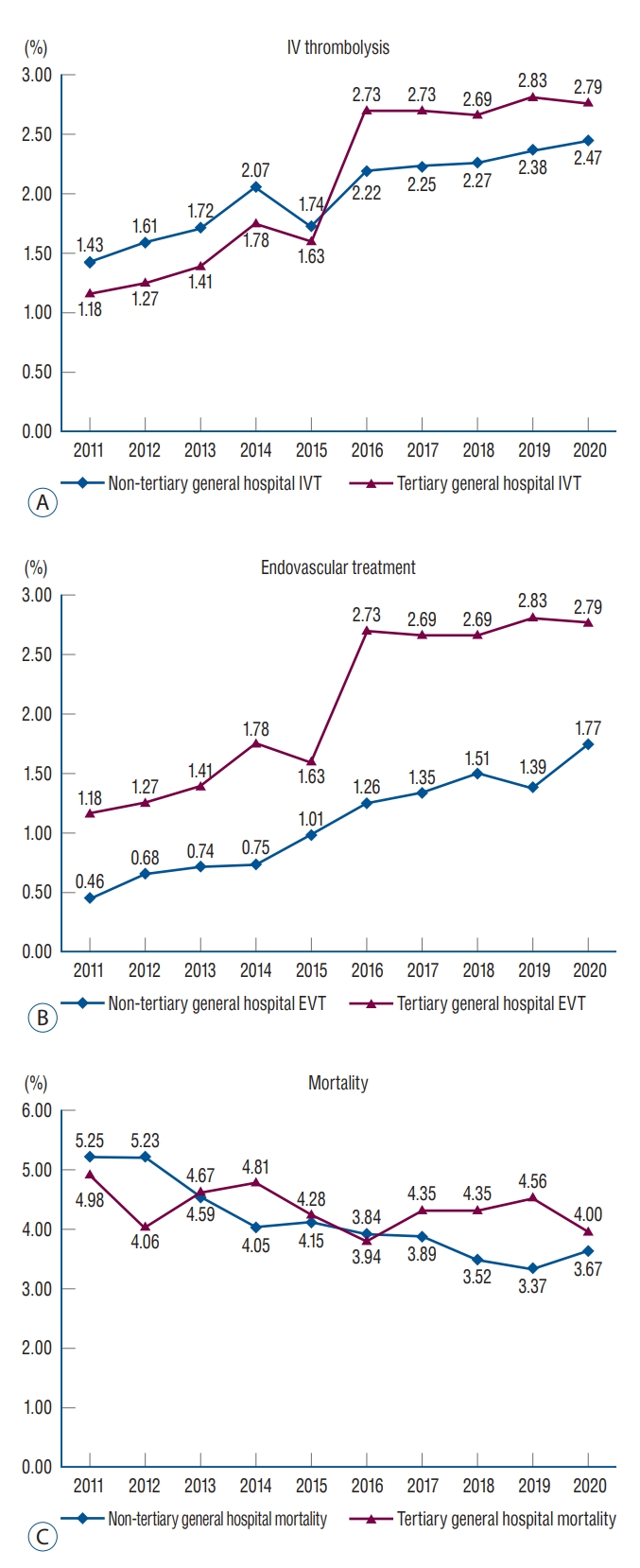
Subgroup analysis according to the type of the hospital (Fig. 3) showed that tertiary general hospital experienced a sudden increase in both IVT and endovascular treatment in 2015. However, non-tertiary general hospital showed a comparatively smaller increase after 2015, with a steady increase until 2020. The mortality rate decreased from 4.98% in 2011 to 4.00% in 2020 at tertiary general hospital. Non-tertiary general hospital showed a greater reduction in mortality rates than did tertiary general hospital (5.25% in 2011 vs. 3.67% in 2020).
DISCUSSION
Main findings
The prognostic impact of modern reperfusion therapy for acute ischemic stroke is yet to be clarified. This study found that the rate of reperfusion therapy (IVT, thrombectomy) increased significantly following the 2015 guideline changes, and this led to a decrease in mortality. The rate of endovascular treatment showed a 2.6-fold increase from 0.71% during the prior period (2011–2014) to 1.85% during the modern period (2017–2020). The 3-month mortality decreased by approximately 22.4%, from 4.78% during the prior period to 3.71% during the modern period.
Decreasing trend in ischemic stroke among patients aged <80 years
The number of patients with acute ischemic stroke aged <80 years has gradually decreased, particularly among women, consistent with that observed in a previous study [10]. It is hypothesized that an increased awareness of stroke prevention and treatment of cardiovascular risk factors led to a decrease in the total incidence of ischemic stroke. Further, Korea’s regular health examination policy has also contributed to this phenomenon. In Korea, citizens aged >40 years are advised to undergo national health examinations at intervals of 1–2 years, and the cost is assumed by the government.
Trend in the use of reperfusion therapy
The rate of IVT use significantly increased between 2015 and 2016 but plateaued thereafter. This trend may be related to the changes in insurance coverage policy in Korea. Previously, IVT was only allowed within 3 hours of symptom onset, but the time window was expanded to within 4.5 hours in January 2014. Furthermore, the age limit of <80 years was revised in December 2018 to allow IVT use for all ages. The government strongly recommends the administration of IVT within 1 hour from emergency room arrival, and this is used as an important indicator for the evaluation of hospital quality [12].
Endovascular treatment for acute ischemic stroke has remarkably increased, starting with the MERCI retrieval system in 2005 from the United States [24]. The penumbra device developed in 2008 failed to achieve superior prognostic benefit to IVT [18]. However, after the failure of first-generation devices, the stent-retriever technique was proven to achieve better recanalization than the MERCI system [16,21]. Recent studies have shown better recanalization rates with the stent retriever and contact aspiration, as well as with the combination of both techniques [13]. Administration of intra-arterial anti-thrombotic agents, balloon angioplasty, and stent insertion also provide more treatment options for complicated cases [9]. In Korea, the penumbra device was first approved as an endovascular treatment for acute ischemic stroke in 2010, and usage of a stentretriever system was allowed in 2013. Prior to the change to the guidelines in 2015, mechanical thrombectomy use was restricted to experienced centers in Korea.
The current study found that the rate of endovascular treatment for acute ischemic stroke has gradually increased since 2015. The data showed that tertiary general hospital more rapidly adapted to the new guidelines than did non-tertiary general hospital. However, non-tertiary general hospital has steadily followed the trend of modern reperfusion therapy since 2015. The endovascular treatment rate was higher in tertiary general hospital, and this was presumed to be due to the greater concentration of patients with severe symptoms in these centers.
Trend in mortality rate after the guideline change
Overall, the 3-month mortality rate showed a decrease of >20% from the prior period to the modern period. Interestingly, the reduction in mortality was higher in non-tertiary general hospital. In total, 75.8% of all patients in Korea were treated in non-tertiary hospital These centers appeared to play a more prominent role in the decrease in mortality, which may be related to the characteristics of the diseases requiring urgent treatment in these centers. In Korea, the number of centers, especially non-tertiary hospital, that provide endovascular treatment for patients with acute ischemic stroke has gradually increased [10]. This may have significantly contributed to the observed reduction in mortality, in that patients with acute ischemic stroke can be treated in community-based centers and no longer need to be transferred to tertiary centers. The role of community-based center is an important issue to be considered when improving the overall quality of medical care provided to patients with acute ischemic stroke.
The introduction of endovascular therapy for patients with acute ischemic stroke has resulted in many positive changes in clinical practice. The most important change is the hyper-alertness of clinicians during the acute period of the disease. Given that it is necessary to determine the need for reperfusion therapy, consultation with a neurologist is essential in the acute period. In Korea, considerable effort has been devoted to the management of patients with acute ischemia. The Health Insurance Review and Assessment Service periodically evaluates the adequacy of acute treatment for patients with stroke and encourages the establishment of a specialized stroke unit. The combination of these factors appears to have led to a decrease in mortality.
The current study confirmed the trend of clinical improvement in patients with acute ischemic stroke, using real-world nationwide health insurance data. However, contrary to our expectations, the craniectomy rate did not show a significant decrease, despite the increase in the use of reperfusion therapy. A more thorough evaluation of patients with malignant cerebral edema was limited as the decision to undergo craniectomy surgery was affected not only by scientific evidence, but also by ethical and economic issues. Another reason is that there are still many patients who are delayed in diagnosis and treatment initiation for acute ischemic stroke. Systemic policy improvement is important in addressing this problem.
Treatment trend and results in elderly patients over 80 years of age
Abrupt increase of IVT use was detected between 2018 and 2019, because of insurance policy change which allowed the use in elderly (>80) patients (Supplementary Fig. 1). Endovascular treatment has increased steadily from 2014 and plateaued after 2019 (Supplementary Figs. 1 and 2). The 3-month mortality rate decreased from prior period (2011–2014) to transition period (2015–2016), when the endovascular treatment began to increase (14.63% to 13.22%). It is assumed that the endovascular treatment contributed more to the reduction in mortality compared to IVT use in elderly patients.
This study has unavoidable limitations owing to the use of insurance claims data, which were not originally collected for research purposes. Patients with acute ischemic stroke shoulder only 5% of medical expenses. Therefore, there is a possibility of an overestimation of the diagnosis. However, given that acute ischemic stroke is covered by the NHIS, there is also the advantage of a low possibility of missing records. The patients included in study was limited to patients matching age (18–80 years), hospital size, and hospitalization route to select patients with acute ischemic stroke. It is presumed that there may have been inappropriate patient dropouts due to recording errors. Therefore, the total number of patients in study is small compared to previous study [8,22,23]. Exclusion of patients with recurrent ischemic stroke may have led to the exclusion of severe symptom patients, resulting in a reduced rate of reperfusion therapy. Further, the identification of IVT use, endovascular treatment, and craniectomy relied on prescription data. As the identification of reperfusion therapy and craniectomy was based on prescription records, it was impossible to include non-prescription treatments. A detailed analysis was not possible due to the lack of information on disease severity and the techniques of endovascular treatment such as contact aspiration or stent retriever. Alternative methods such as intracranial and extracranial stenting or balloon angioplasty was also impossible to distinguish with reimbursement data. Although modified Rankin Scale is most appropriate for measuring patient clinical outcome, it has a limitation that only 3 months mortality was used. There is also a possibility of recording errors. Finally, only East Asian Koreans were evaluated, and elderly patients aged >80 years were excluded owing to the insurance coverage policy.
CONCLUSION
Changes in the guidelines for the management of patients with acute ischemic stroke have resulted in an increase in the use of reperfusion therapy and a reduction in mortality in real-world practice in Korea. Although tertiary general hospital adjusted rapidly to the new guidelines, non-tertiary general hospital had a more prominent contribution to the decrease in mortality. Our data suggest that community-based hospital play a more important role in improving the overall prognosis of patients with acute ischemic stroke.
Notes
Conflicts of interest
No potential conflicts of interest relevant to this study exist.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : YKP, BHY, JHK; Data curation : YKP; Formal analysis : YDW, HIK; Funding acquisition : YKP; Methodology : YKP, BHY; Project administration : JHK; Visualization : YDW; Writing - original draft : YKP; Writing - review & editing : JHK, HIK
Data sharing
None
Preprint
None
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (NRF-2022R1G1A1010805).
Supplementary materials
The online-only data supplement is available with this article at https://doi.org/10.3340/jkns.2023.0133.
Characteristics of patients aged >80 years
Annual trends in reperfusion therapy and craniectomy for patients with acute ischemic stroke aged >80 years. Patients aged >80 years who are admitted with acute ischemic stroke (I63 code) via the emergency room between January 2011 and December 2020 at any general or tertiary general hospital with >100 beds were included. The research method is the same as that in the main study. IVT : intravenous thrombolysis.
Annual trends in 3-month mortality by study period for patients with acute ischemic stroke aged >80 years. IVT : intravenous thrombolysis.
Codes of claims data