Frequency and Characteristics of Paraclinoid Aneurysm in Ruptured Cerebral Aneurysms
Article information
Abstract
Objective
This study aimed to determine the frequency of paraclinoid aneurysms among ruptured cerebral aneurysms and compare paraclinoid aneurysms with other aneurysms to clarify the characteristics of ruptured paraclinoid aneurysms.
Methods
This study included 970 ruptured cerebral aneurysms treated at our hospital between 2003 and 2020.
Results
There were 15 cases (1.3%) of paraclinoid aneurysms with maximum diameters of 5–22 mm (mean±standard deviation [SD], 11.6±5.4 mm). Treatment consisted of clipping in four patients and endovascular treatment in 11. Factors significantly different in multivariate analysis for paraclinoid aneurysms compared with those for other aneurysms were a history of hypertension (odds ratio [OR], 1.2–9.8; p=0.021) and aneurysm ≥10 mm (OR, 7.5–390.3; p<0.001). The sites of paraclinoid aneurysm were ophthalmic artery type in nine patients, anterior wall type in five, medial wall type in one, and ventral wall type in zero. The medial wall type (22 mm) was significantly larger than the ophthalmic artery type (mean±SD, 7.2±2.0 mm) (p=0.003), and the anterior wall type (mean±SD, 12.2±4.8 mm) was significantly larger than the ophthalmic artery type (p=0.024).
Conclusion
This study showed a low frequency of paraclinoid aneurysms among ruptured cerebral aneurysms. Most were upward-facing with relatively large aneurysms, and no aneurysms were smaller than 5 mm. With recent advances in endovascular treatment devices, paraclinoid aneurysms are easily treatable. However, the treatment indication of each paraclinoid aneurysm should be carefully considered.
INTRODUCTION
Paraclinoid aneurysms are the most frequently observed type of unruptured cerebral aneurysm [4]. Identifying the risk of rupture is important to avoid excessive surgery for paraclinoid aneurysms. The natural history of unruptured paraclinoid aneurysms are not well-understood, although a few studies have reported a low frequency of ruptured paraclinoid aneurysms [11,13,18]. Comparatively, the frequency and characteristics of paraclinoid aneurysms among ruptured cerebral aneurysms can be used to estimate the likelihood of rupture of a paraclinoid aneurysm. However, there are few reports on the frequency of paraclinoid aneurysm among ruptured aneurysms [9].
This study aimed to determine the frequency of paraclinoid aneurysms among ruptured cerebral aneurysms treated at our institution and to compare paraclinoid aneurysms with other aneurysms to clarify the characteristics of ruptured paraclinoid aneurysms.
MATERIALS AND METHODS
This study was approved by the Clinical Research Review Committee of the Tokai University School of Medicine (approval No. 18R-038).
Patients population
A total of 1087 ruptured cerebral aneurysms treated at our hospital between 2003 and 2020 were included in this study. Vertebral dissecting aneurysms, blister-like aneurysms of the internal carotid artery (ICA), and severe cases that did not undergo surgery were excluded. Clinical findings including age, sex, history of hypertension and diabetes mellitus, World Federation of Neurosurgical Societies (WFNS) classification, treatment method (clipping/endovascular treatment), hydrocephalus, ventriculoperitoneal shunt, and modified Rankin Scale (mRS) score at discharge were evaluated from medical records. The treatment procedure was decided on a case-bycase basis following a discussion between an endovascular specialist and a craniotomy specialist.
Radiological evaluation
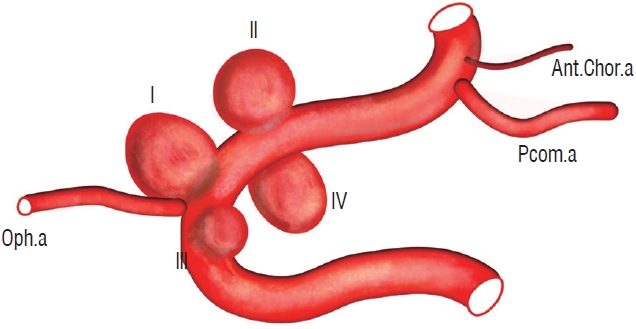
Head computed tomography (CT) revealed the Fisher grade at admission. The location and maximum diameter of the aneurysm were determined using digital subtraction angiogram (DSA). The aneurysm locations were divided into paraclinoid aneurysms and others. Paraclinoid aneurysms were classified using the Barami classification as follows [1] : ophthalmic artery type, anterior wall type, medial wall type, and ventral wall type (Fig. 1).
Statistical analysis
Student’s t-test or Mann-Whitney U test was used to compare continuous variables, while the chi-square test or Fisher’s exact test was used for categorical variables. Numerical data are expressed as the mean±standard deviation. Multiple logistic regression analysis was used for multivariate analysis, factors with p<0.1 in univariate analysis were used as independent factors, and all factors with p<0.05 in stepwise subtraction were retained in the final model. Results with p<0.05 were considered significant in this study. The analysis software used was IBM SPSS statistics ver. 26 (IBM, Armonk, NY, USA).
RESULTS
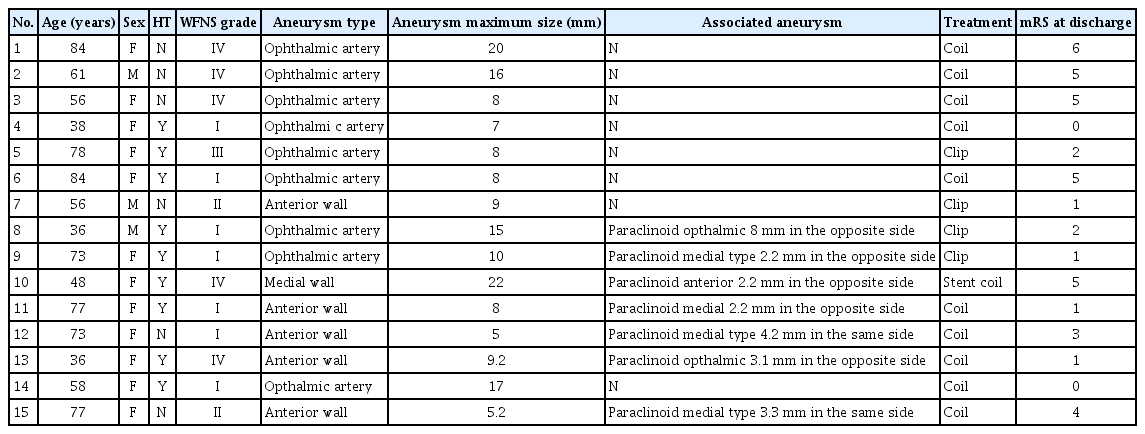
Among the 1087 patients with ruptured cerebral aneurysms, 970 were included in this study. We excluded were 56 patients who had vertebral artery dissecting aneurysms, 15 patients who had ICA blister-like aneurysms, and 46 patients who did not undergo surgery because of their severe disease status. Paraclinoid aneurysms were observed in 15 patients (1.3%) (Table 1). The mean age was 62.3 years, three were males and 12 were females, and nine of the 15 patients had a history of hypertension. The WFNS classification was I-II in nine patients, III in one, and IV-V in five. Fisher grades were 1, 2, 3, 4 in one, four, nine, and one patient, respectively. The maximum aneurysm diameter ranged from 5 to 22 mm (11.6 ±5.4 mm). Treatment consisted of clipping in four patients and endovascular treatment in 11 patients. All four patients who underwent clipping underwent clinoidectomy while securing the cervical ICA. After 2013, all patients underwent endovascular treatment. Of the 11 patients who underwent endovascular treatment, three were treated with a single catheter technique, seven with balloon-assisted embolization, and one with stent-assisted embolization. The outcomes at discharge were mRS 0–2 in eight patients, mRS 3–5 in six patients, and mRS 6 in one patient. Seven of the 15 patients (46%) had aneurysms associated with other aneurysms, all of which were paraclinoid aneurysms, either of another ipsilateral type or the contralateral paraclinoid aneurysm.
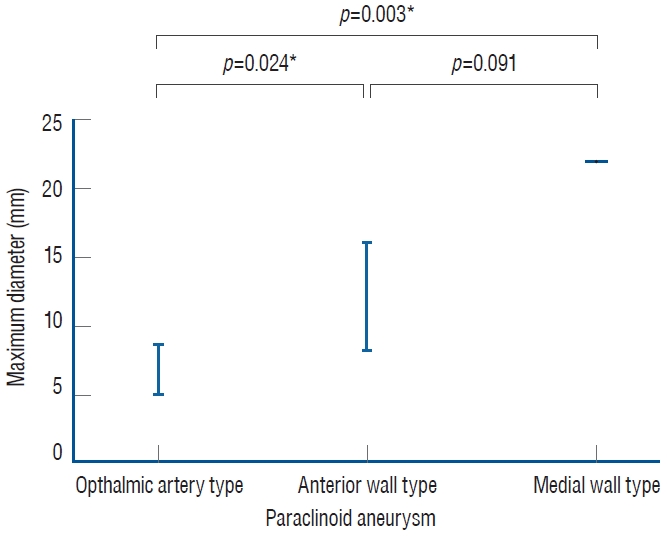
A comparison of paraclinoid and other aneurysms is shown in Table 2. Factors significantly different in univariate analysis for paraclinoid aneurysm compared with those for other aneurysms were a history of hypertension (p=0.026), maximum diameter (p=0.009, ruptured paraclinoid aneurysm 11.1±5.4 mm, other ruptured cerebral aneurysms 6.1±3.5 mm), aneurysm size >10 mm (p=0.004), and more endovascular treatment (p=0.009). Factors that differed significantly in the multivariate analysis were history of hypertension (odds ratio [OR], 1.2–9.8; p=0.021) and aneurysm ≥10 mm (OR, 7.5–390.3; p<0.001).
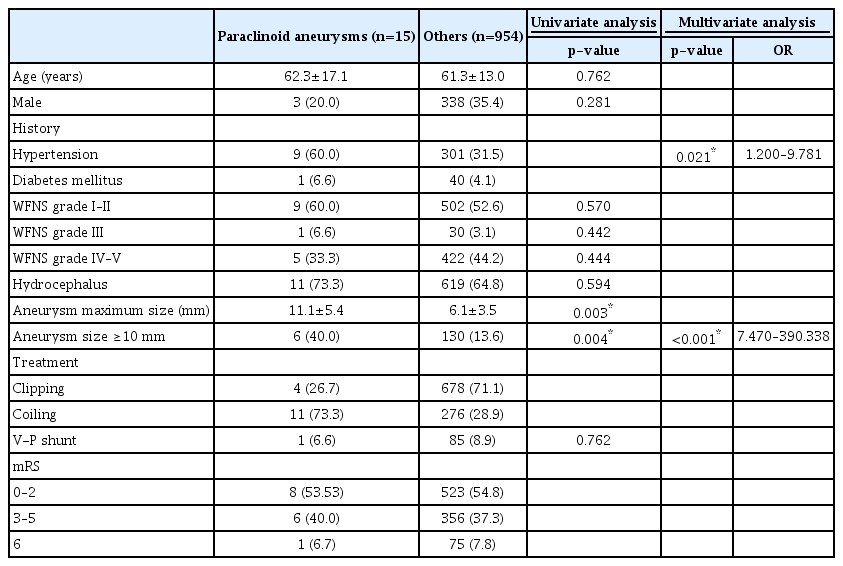
The location of the paraclinoid aneurysm was ophthalmic artery type in nine patients, anterior wall type in five, medial wall type in one, and ventral wall type in zero. Aneurysm size according to location is shown in Fig. 2. The medial wall type (22 mm) was significantly larger than the ophthalmic artery type (7.2±2.0 mm) (p=0.003). The anterior wall type (12.2±4.8 mm) was significantly larger than the ophthalmic artery type (p=0.024).
Comparisons of paraclinoid aneurysm types. The maximum diameters of the ophthalmic artery type, the medial wall type, and the anterior wall type, were 7.2±2.0 mm (mean±standard deviation), 22 mm, and 12.2±4.8 mm. The medial wall type was significantly larger than the ophthalmic artery type (p=0.003), and the anterior wall type was significantly larger than the ophthalmic artery type (p=0.024). *Indicates a significant difference of p<0.05.
Illustrative case 1
Herein, we report a didactic case in which a paraclinoid aneurysm was presumably diagnosed as a ruptured aneurysm and treated; however, an aneurysm in another location, had ruptured (Fig. 3). A woman in her 70s was admitted to our hospital as an emergency case because she lost consciousness after experiencing a headache. On arrival at the hospital with a Glasgow coma scale score of 10 (E, 3; V, 1; M, 6), no paresis was observed. Head CT showed a thick subarachnoid hemorrhage (SAH) in the basal cistern. DSA showed a left medial wall type paraclinoid aneurysm (3.6×3.0 mm), the left ICA cavernous aneurysm (2.9×2.3 mm), and a left ICA-posterior communicating artery (Pcom) aneurysm (1.1×0.9 mm). We decided to treat the medial wall type paraclinoid aneurysm, which was supposed to be a ruptured aneurysm based on the size of the aneurysm. Endovascular treatment was performed the same day using a single catheter technique to embolize the medial wall type aneurysm. DSA ten days after the procedure showed an enlarged ICA-Pcom aneurysm (3.1×3.6 mm). Subsequently, the ruptured aneurysm was revealed to be an ICA-Pcom aneurysm. Emergency endovascular treatment was performed to embolize the aneurysm. The patient had a cerebral infarction due to cerebral vasospasm in the perioperative period and was transferred to a rehabilitation hospital after 2 months, with an mRS score of 4.
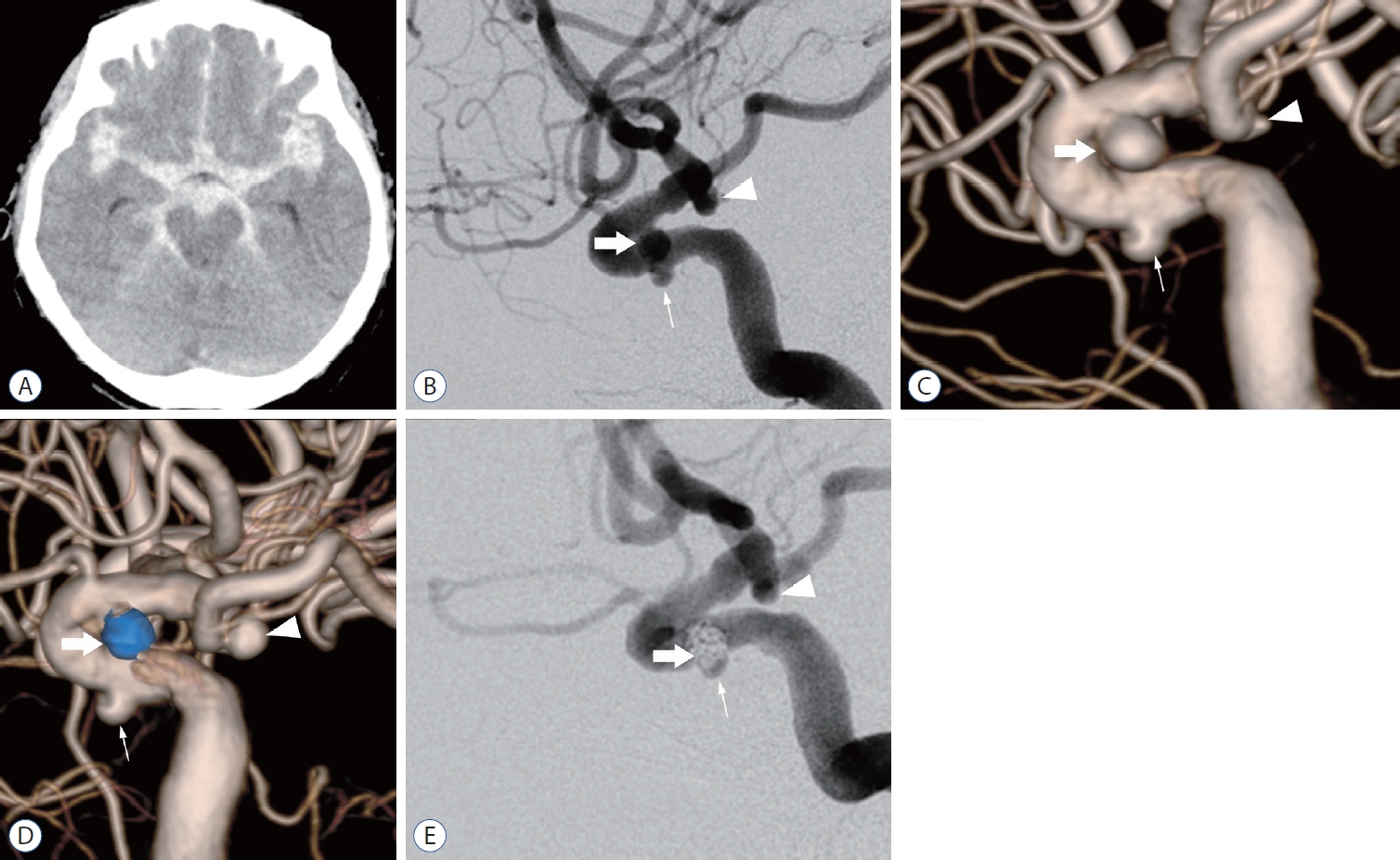
A didactic case of enlargement of a ruptured internal carotid artery (ICA)-posterior communicating artery (Pcom) aneurysm was revealed after embolization of a paraclinoid aneurysm following subarachnoid hemorrhage (SAH). A : A head computed tomogram showing thick SAH in the basal cistern. B and C : Lateral image of the preoperative left ICA angiogram (C : 3-dimensional digital subtraction angiogram, 3-DDSA). The medial wall type paraclinoid aneurysm is 3.6×3.0 mm (thick white arrow), and the left ICA cavernous aneurysm is 2.9×2.3 mm (thin white arrow). ICA-Pcom aneurysm (white arrowhead) with a size of 1.1×0.9 mm is observed. D : Left ICA 3-DDSA 10 days after 1st embolization. The embolized medial wall type paraclinoid aneurysm (thick white arrow) and ICA cavernous aneurysm (thin white arrow) are unchanged, but the ICA-Pcom aneurysm (white arrowhead) enlarges to 3.1×3.6 mm. E : Lateral image of the left ICA angiogram after 2nd embolization. The white arrowhead indicates coils inserted into the ICA-Pcom aneurysm, and the white arrows indicate the preserved posterior communicating artery. The thick white arrow indicates embolized medial wall-type paraclinoid aneurysm, and the thin white arrow indicates ICA cavernous aneurysm.
Illustrative case 2
Herein, we report a case of a typical ruptured paraclinoid aneurysm with a size greater than 10 mm. A 61-year-old woman, who suffered from a sudden onset headache, was taken to the emergency room by ambulance. On arrival, she showed no neurological deficit. A CT scan demonstrated SAH (Fig. 4A). A cerebral angiogram revealed a paraclinoid aneurysm of ophthalmic type with a maximum diameter of 17 mm (Fig. 4B and C). The patient underwent endovascular coil embolization using a balloon-assisted technique (Fig. 4D). She was discharged to home without any deficit 1 month later.

A typical ruptured paraclinoid aneurysm case with a size more than 10 mm. A : A head computed tomogram showing thin subarachnoid hemorrhage in the left Sylvian fissure (white arrow). B : A left internal carotid artery (ICA) angiogram (lateral view) showing an ophthalmic artery type paraclinoid aneurysm with a diameter of 17 mm (white arrowhead). A white arrow indicates the ophthalmic artery. C : A left ICA 3-dimensional angiogram revealing a relationship between an aneurysm (white arrowhead) and the ophthalmic artery (white arrow). D : A left ICA angiogram after embolization showing the disappearance of the aneurysm filled with coils (white arrowhead). The ophthalmic artery is preserved (white arrow).
DISCUSSION
The study demonstrated that paraclinoid aneurysms accounted for 1.3% of ruptured aneurysms and that 40% of ruptured paraclinoid aneurysms were larger than 10 mm. To the best of our knowledge, this is the first reported study revealing that ruptured paraclinoid aneurysms are significantly larger than 10 mm compared to another ruptured aneurysms.
Frequency of paraclinoid aneurysm among both unruptured and ruptured cerebral aneurysms
The prevalence of unruptured cerebral aneurysms in Japan was reported to be 4.32% in those over 22 old and greater than 6% in those over 60 years old, with the prevalence increasing with age [4]. Paraclinoid aneurysms were the most common type (45.7%) [4]. However, ruptured paraclinoid aneurysms account for 1.4–5% of all ruptured cerebral aneurysms, which is lower than that of theanother aneurysms [9,10,13].
The natural history of paraclinoid aneurysms is unclear. Fukaya et al. reported that 119 patients with paraclinoid aneurysm with diameters of 2–9 mm showed no enlargement, shape change, or rupture of the aneurysm during a mean follow-up period of 5.2 years by magnetic resonance imaging (MRI) [2]. Kalluri et al. [7] reported on 290 patients with unruptured cerebral aneurysms of carotid caves <4 mm who were observed for a mean of 3.3 years; they noted no ruptured aneurysms. Jeon et al. [5] reported SAH in two (0.35%) of 568 patients with unruptured paraclinoid aneurysms <5 mm and enlargement in 17 patients (3.0%) after 35.4 months of follow-up. These reports have described paraclinoid aneurysms of less than 10 mm [2,5-7]. However, there have been no reports of unruptured paraclinoid aneurysms measuring ≥5 mm. In UCAS-Japan, the rupture rate of ICA aneurysms, excluding ICA-Pcom aneurysms, was lower than that of other cerebral aneurysms [18]. The reason for this was the presence of paraclinoid aneurysms along with other ICA aneurysms. There have been many reports of clipping and endovascular treatment for paraclinoid aneurysms [1,9,14]; however, the natural history of unruptured paraclinoid aneurysms has seldom been reported.
The frequency of paraclinoid aneurysm among ruptured cerebral aneurysms can be used to estimate the likelihood of paraclinoid aneurysm rupture. However, few reports have indicated the frequency of paraclinoid aneurysms in SAH. In this study, ruptured paraclinoid aneurysms were observed in 15 of 1087 patients (1.3%). Loumiotis et al. [9] reported that 33 of 367 (8.9%) ruptured aneurysms were paraclinoid aneurysms. Nguyen et al. [11] also reported that 62 of 682 (9.0%) ruptured cerebral aneurysms were paraclinoid aneurysms, which was higher than the rate of ruptured aneurysms in the present study. The difference in the frequency might be explained by the different races of the study subjects, because the occurrence rates of SAH differed among races, and the statistics of aneurysmal rupture supposedly depend on races [3].
Comparison of paraclinoid aneurysms and other ruptured cerebral aneurysms
In this study, the size of the ruptured paraclinoid aneurysms was 11.1±5.4 mm, significantly larger than that of other ruptured cerebral aneurysms (6.1±3.5 mm). Ruptured paraclinoid aneurysms were significantly larger than those with a maximum diameter of 10 mm. Oh et al. [12] compared 228 unruptured paraclinoid aneurysms with 25 ruptured paraclinoid aneurysms and found that the ruptured paraclinoid aneurysms accounted for more aneurysms larger than 10 mm; the results were similar to our report.
The present study showed a high frequency of other aneurysms associated with ruptured paraclinoid aneurysms, which was found in seven of 15 patients (46%) with ruptured paraclinoid aneurysms. Kinouchi et al. [8] studied on paraclinoid aneurysms in seven of 1164 patients treated for cerebral aneurysms (two ruptured and five unruptured aneurysms). Among the seven patients with paraclinoid aneurysms, five patients (71%; one ruptured and four unruptured aneurysms) showed multiple aneurysms, in which a frequency of multiple aneurysms was higher than a frequency in our study [8]. Regarding multiple aneurysms in entire intracranial locations, Sturiale et al. [16] reported that associated other location aneurysms were found in 62 of 265 patients (23%) with ruptured cerebral aneurysms. Ruptured paraclinoid aneurysms may be more frequently associated with other cerebral aneurysms than aneurysms in other locations.
Comparison of paraclinoid aneurysms in different locations
In this study, the location of the ruptured paraclinoid aneurysm was five anterior wall types, nine ophthalmic artery types, one medial wall type, and zero ventral wall type out of 15 patients. Fourteen patients (93.3%) upward-facing aneurysms. Oh et al. [12] reported that of 228 unruptured paraclinoid aneurysms, 125 (51%) were of the medial wall type. Sorimachi et al. [15] also reviewed 140 cases of unruptured cerebral aneurysms treated endovascularly and reported 29 anterior wall types, 18 ophthalmic artery types, one ventral wall type, and 78 medial wall type aneurysms. Rupture of a medial wall type aneurysm, commonly found as an unruptured cerebral aneurysms, occurred in only one of the 15 patients in this study.
In the present study, the size of ruptured paraclinoid aneurysms ranged from 5 to 22 mm (11.1±5.4 mm), and there were no ruptured paraclinoid aneurysms smaller than 5 mm. The mean of aneurysm sizes in the ophthalmic artery type, anterior wall type and medial wall type were 7.2, 12.2, and 22 mm, respectively. Only one medial wall-type aneurysm showed the largest maximum diameter, significantly larger than the ophthalmic artery type (p=0.003).
In the present study, nine of the 15 cases (60%) were of the ophthalmic artery type, while five (33%) were of the anterior wall type, which may have reflected this anatomic feature. Among paraclinoid aneurysms, ophthalmic artery and anterior wall types may be considered for treatment. However, the medial and ventral wall types should be carefully considered as the indication for treatment. On the other hand, a medial wall type might cause visual field impairment due to optic nerve compression. Therefore, a particular size needs to be treated for purposes other than rupture prevention. As demonstrated in the illustrative case 1 presented hererin, because small sized paraclinoid aneurysms seldom rupture, it was necessary to consider the possibility that an aneurysm other than a paraclinoid aneurysm might have ruptured, even if the other aneurysm was small.
In the present study, a relatively large size, a high proportion of hypertension, and no ruptured cases of ventral wall aneurysms were the clinical characteristics of rupture paraclinoid aneurysms. Paraclinoid aneurysms, especially ventral wall type aneurysms, are mainly covered by a hard structure such as the dura mater or bone, which probably limits the growth of the aneurysm and prevents its rupture. This structural feature could lead seldom the rupture of ventral wall aneurysms. Among paraclinoid aneurysms, an upward-facing paraclinoid aneurysm not surrounded by structures such as the dura mater or bone was reported to be at risk of rupture [12]. Depending on the location, the ophthalmic artery type also has areas not covered by the dural ring. Both the large size of a cerebral aneurysm and hypertension are well-known risk factors for rupture of a cerebral aneurysms [17]. In comparison to the other location aneurysms, paraclinoid aneurysms are less likely to rupture due to this structural feature, therefore, paraclinoid aneurysms might less frequently rupture until predisposed risk factors, including large-size aneurysm and hypertension, exist.
CONCLUSION
Among the 970 ruptured cerebral aneurysms, a frequency of paraclinoid aneurysms was only 1.3%, and more than 90% of the ruptured paraclinoid aneurysms belonged to either ophthalmic artery type or anterior wall type. No ruptured paraclinoid aneurysms were smaller than 5 mm. Indication for the paraclinoid aneurysm treatment should be carefully considered, especially when the aneurysm is located in the medial wall or the ventral wall of the ICA.
Notes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : HS; Data curation : HS, KY, AH, TS; Formal analysis : TS; Methodology : HS; Project administration : TS; Visualization : HS; Writing - original draft : HS; Writing - review & editing : HS, KY, AH, TS
Data sharing
None
Preprint
None