Lying Down Instability Undetected on Standing Dynamic Radiographs
Article information
Abstract
It is well known that spinal instability should be evaluated in the standing lateral position. Standing dynamic flexion and extension radiographs are usually used to assess spinal instability. Here, we report a patient who experienced distraction instability while in the supine position rather than the standard standing position. To our knowledge, this is the first report of lying-down instability undetected on standing dynamic flexion and extension radiographs. We discuss the pathophysiological mechanism of this uncommon but possible entity and provide a review of the literature.
INTRODUCTION
Currently, simple lateral radiographs taken in the standing position are a useful diagnostic tool for spinal instability. Usually, it is assumed that flexion accentuates anterior displacement. Therefore, if a patient does not have any abnormalities or instability on dynamic images of the lumbar spine, including standing flexion and extension radiographs, we can conclude that the patient has no abnormalities associated with lumbar spine instability. In this report, we introduce an interesting case of occult instability with no obvious features on dynamic standing flexion and extension views, which was successfully identified with a recumbent lateral radiograph.
The objective of this report is to introduce lying down instability undetected on standing dynamic flexion and extension radiographs usually used to evaluate spinal instability. We reviewed the medical literature to identify the relevant studies concerning patients with distraction instability detected only on recumbent lateral radiographs.
CASE REPORT
A 61-year-old woman was admitted to our institute with a history of severe back pain and progressive difficulty in ambulation. Her symptoms gradually deteriorated, despite sustained rehabilitation and exercise. Five days before admission, she was unable to walk even 5 meters after arising from the floor. She experienced symptoms while in the supine position as well as during standing and sitting. She underwent decompression surgery at the L4–5 level 3 years ago because of spondylolisthesis.
The lowest T-score by dual-energy X-ray absorptiometry bone mineral densitometry was -3.9. A physical examination revealed no motor weakness or sensory change, but slight tenderness was present in the upper lumbar region. Plain radiographs showed a significant scoliotic curve and disc space narrowing at L2–3 and spondylolisthesis at L4–5, for which decompression surgery was performed 3 years ago. Plain lateral radiographs, including dynamic flexion and extension views, showed no significant instability at L2–3 (Fig. 1). Because of the patient's complaint of severe back pain even in the recumbent position, a simple lateral radiograph with the patient in the neutral supine position which had also aggravated her symptoms was obtained. It showed significant retrolisthesis and lying down instability at L2–3 (Fig. 2A).
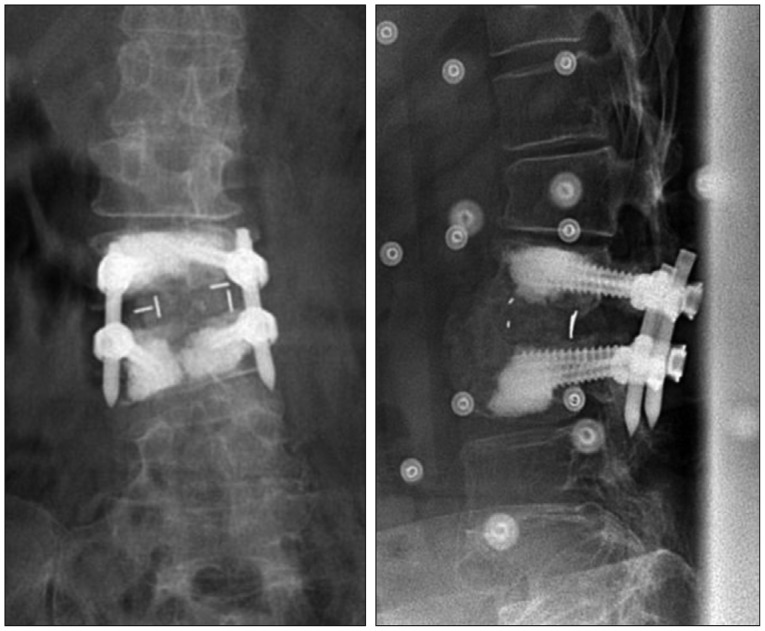
Simple lateral, flexion, and extension radiographs taken in the standing position show disc space narrowing without significant instability at L2–3.
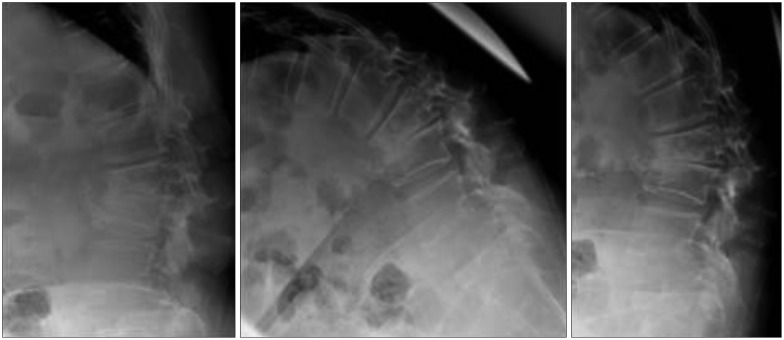
Simple lateral radiograph and T2-weighted magnetic resonance images taken in the recumbent position reveal significant instability at L2–3 level, with a fluid-filled disc space accompanying severe stenosis.
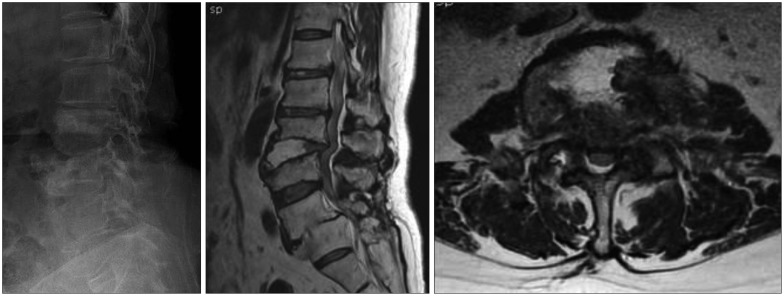
Magnetic resonance imaging (MRI), which also was performed with the patient in the recumbent position, revealed severe stenosis with retrolisthesis at L2–3 (Fig. 2B). T2-weighted image of the disc space showed high signal intensity, suggesting a fluid-filled disc. The patient underwent posterior lumbar interbody fusion with screw fixation at L2–3 (Fig. 3). After surgery, complete pain relief was achieved and the patient was able to ambulate without difficulty; she complained only of mild back stiffness 12 months after surgery.
DISCUSSION
The development of bipedalism in humans determined a series of peculiar changes in spinal anatomy and biomechanics. These changes include the verticalization of the pelvis and the development of the spinal sagittal curvatures, i.e., lumbar lordosis and thoracic kyphosis, which are specific to humans10). As a result, human posture is continuously subject to the effects of gravity in positions other than that of recumbent15).
As gravity acts on all parts of the body, one's entire weight can be considered as concentrated at a point where the gravitational pull on one side of the body is equal to the pull on the other side. This point is the body's center of gravity and any change of body position can leads to change the center of gravity7). When the spine is flexed forward or backward, the center of gravity shifts anteriorly and posteriorly, respectively. Through these changes, joint instability is easily evaluated by the use of flexion and extension lateral radiographic views of the spine in patients with spondylolisthesis and retrolisthesis. When patients with spondylolisthesis flex the spine, the center of gravity moves anteriorly and leads to anterior slippage of the unstable vertebra. In contrast to spondylolisthesis, when patients with retrolisthesis flex the spine, compensation of the unstable vertebra through anterior slippage of the vertebra is induced. Extension of the spine leads to posterior slippage of the vertebra and exaggerated instability in patients with retrolisthesis7). Spinal loads incorporate gravity and the corresponding stabilizing vertical action of muscles acting on vertebrae. It is then assumed that the principal component of the resultant loads on the vertebral bodies lies close to the direction of gravity.
In posture-dependent degenerative spinal disorders, weight-bearing postures resulting in axial load and compressive force contribute to change the morphology of the spine. Flexion and extension radiographs are commonly used to assess spinal instability in patients with spondylolisthesis6).
In patients with spondylolytic spondylolisthesis, the pars defect disconnects the vertebral body from the inferior articular process. The loss of this posterior stabilizing element causes the vertebra to be susceptible to excessive forward translation during spinal flexion8).
Our patient had no spondylolysis, but retrolisthesis was present at L2–3. No significant instability was seen on standard standing dynamic flexion and extension radiographs. Kanayama et al.4) found that distraction instability were highly related to disc angle in flexion and range of motion, and the cases with segmental kyphosis in flexion had lower distraction stiffness in their intraoperative biomechanical assessment. Alternatively, severity of slip and facet tropism were unlikely related to the lumbar distraction instability. In addition, as Tencer et al.9) reported, an intervertebral disc is the major load-bearing element in flexion and axial compression. Our patient complained of severe back pain and she could not extend the spine correctly. We could not detect spinal instability on dynamic flexion and extension radiographs. We checked the simple lateral X-ray and MRI taken in the supine position. In the supine position, the gravity and body weight compress the unstable vertebra perpendicularly, which leads to distraction instability. Consequently, we could identify the instability through those studies taken in the supine position.
In the recumbent position, when compared to flexion, the anterior column is subjected to a distractive force, whereas the posterior column is subjected to a compressive force3).
Generally, we identify spine instability through the dynamic flexion and extension radiographic views with the patient in the standing position. However, if a patient can not assume a correct dynamic posture because of severe pain and there are few differences between lateral and dynamic lateral radiographic views, as with our patient, then the possibility of distraction instability should be considered. We believe that this report is of interest in some aspects. First, it is simple and economical procedure with no additional procedures or provocation. Second, the effect of musculature on the spinal instability can be diminished in the supine position. Actually, D'Andrea et al.2) reported that supine-prone position is mandatory for performing a dynamic X-ray examination instead of a standard examination in the upright standing position, in extension and in flexion. The higher degree of instability was noticed in the supine-prone. As a matter of course, whole spine radiographs and translateral view can help us evaluate the global sagittal balance and instability, especially for the kyphosis. The effort to evaluate these decisive radiologic information through whole spine radiographs is necessary.
CONCLUSION
A simple lateral radiograph taken in a recumbent position can help overcome the limitations of dynamic flexion and extension views, which may overlook distraction instability.