Bone Cement-Augmented Percutaneous Short Segment Fixation: An Effective Treatment for Kummell's Disease?
Article information
Abstract
Objective
The aim of this prospective study was to evaluate the efficacy of bone cement-augmented percutaneous short segment fixation for treating Kummell's disease accompanied by severe osteoporosis.
Methods
From 2009 to 2013, ten patients with single-level Kummell's disease accompanied by severe osteoporosis were enrolled in this study. After postural reduction for 1-2 days, bone cement-augmented percutaneous short segment fixation was performed at one level above, one level below, and at the collapsed vertebra. Clinical results, radiological parameters, and related complications were assessed preoperatively and at 1 month and 12 months after surgery.
Results
Prior to surgery, the mean pain score on the visual analogue scale was 8.5±1.5. One month after the procedure, this score improved to 2.2±2.0 and the improvement was maintained at 12 months after surgery. The mean preoperative vertebral height loss was 48.2±10.5%, and the surgical procedure reduced this loss to 22.5±12.4%. In spite of some recurrent height loss, significant improvement was achieved at 12 months after surgery compared to preoperative values. The kyphotic angle improved significantly from 22.4±4.9° before the procedure to 10.1±3.8° after surgery and the improved angle was maintained at 12 months after surgery despite a slight correction loss. No patient sustained adjacent fractures after bone cement-augmented percutaneous short segment fixation during the follow-up period. Asymptomatic cement leakage into the paravertebral area was observed in one patient, but no major complications were seen.
Conclusion
Bone cement-augmented percutaneous short segment fixation can be an effective and safe procedure for Kummell's disease.
INTRODUCTION
Delayed post-traumatic vertebral collapse, characterized by painful kyphosis that develops several weeks or months following an injury after a symptom-free period, was first described by the German surgeon Hermann Kummell7). Multiple synonymous terms have been used to describe Kummell's disease, including delayed post-traumatic vertebral collapse, non-union of a compression fracture, vertebral osteonecrosis, and intravertebral pseudarthrosis611).
For Kummell's disease with persistent pain and without neurological symptoms, percutaneous vertebroplasty (VP) or balloon kyphoplasty (KP) has been known to achieve good results49). However, more recent studies hypothesize that the rate of osteolysis among patients with Kummell's disease is greater than the rate of bone callus formation. As a result, following VP or KP, accelerated osteolysis may occur and displace the bone cement, and bone cement augmentation procedures such as VP and KP alone for Kummell's disease, even without neurologic deficits, often result in bone cement displacement81314). Nowadays some good clinical outcomes are reported with bone cement augmented short segment fixation with thoracolumbar burst fractures regardless of osteoporosis5).
As far as the authors' knowledge, however, there is no report for Kummell's disease prospectively investigating the clinical outcome of bone cement augmented percutaneous short segment fixation.
The purpose of this study was to evaluate whether bone cement-augmented percutaneous screw fixation could be a standard treatment option for Kummell's disease without neurologic deficits.
MATERIALS AND METHODS
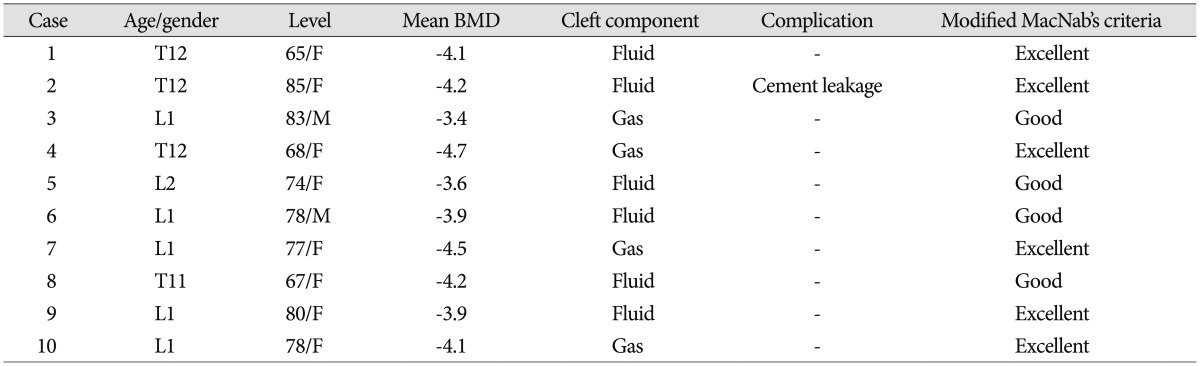
From 2009 to 2013, ten patients (2 males and 8 females) with Kummell's disease accompanied by severe osteoporosis were enrolled in this study. The inclusion criteria were 1) intact neurological status despite single-level Kummell's disease, 2) age 65 years and over, 3) severely osteoporotic spine (mean T-score on DEXA bone mineral densitometry at lumbar area<-3.0, and 4) newly diagnosed osteoporosis. Kummell's disease was diagnosed according to intravertebral cleft (IVC) signs on simple lateral radiographs and computed tomography (CT) or evidence of osteonecrosis with a fluid sign on magnetic resonance imaging (MRI) (Fig. 1). Patients with conditions requiring anterior decompression to ameliorate neurologic deficits, multiple compression fractures, or a history of previous vertebroplasty or spinal surgery were excluded.

The component of intravertebral cleft is divided into gas and fluid. A : Intravertebral gas at L1 level is a computed tomographic finding indicative of Kummell's disease. B : Intravertebral fluid filled cleft at L1 level on magnetic resonance imaging is also characteristic of Kummell's disease.
Surgical procedure
After sufficient explanation of procedure-related complications, postural reduction to achieve hyperextension was conducted for 1-2 days, using a soft roll under the collapsed vertebra with the patient in the supine position. This postural reduction generally restored most of the vertebral height of the fractured vertebra.
Bone cement-augmented percutaneous screw fixation confined to one level above, one level below, and at the collapsed vertebra itself was performed. Bone cement augmentation was achieved using polymethylmethacrylate (PMMA), which was injected under C-arm guidance through a vertebroplasty needle. Approximately 2.5 cc of PMMA was injected through each of the vertebroplasty needle, a total of 5 cc per vertebra.
Vertebral height loss was measured at the site of anterior collapse on lateral radiograph or sagittal CT scan. The vertebral heights were reported as fractions of anterior height between fractured vertebra and normal height of adjacent one level below the fractured vertebra. Kyphotic angle (Cobb's angle) was measured by drawing a straight line from the superior endplate of one level above the fractured body and a straight line from the inferior endplate of one level below the fractured body on a true lateral radiograph.
Imaging and clinical findings, including the involved level, vertebral height loss, evidence of local kyphosis, clinical outcomes, and complications were analyzed.
Statistical analysis
Statistical analysis was performed using SAS 6.12 (SAS Institute Inc., Cary, NC, USA). Mean value (MV) and standard deviation (SD) were calculated for all measurements. Comparisons between different time points were made using the Wilcoxon signed-rank test (Mann-whitney's U test). p values<0.05 were considered statistically significant.
RESULTS
All fractures occurred at the thoracolumbar junction. Anatomic distribution of the collapsed vertebrae was as follows : T11 (n=1), T12 (n=3), L1 (n=5), and L2 (n=1). Mean age of the patients was 75.4 years (range, 64-85 years). As mentioned above, all patients had severely osteoporotic spines, with a mean T-score of-4.06 (Table 1). Mean operation time was 52 minutes and no patient needed a drainage catheter or blood transfusion. All patients were able to ambulate at 24 hours after surgery wearing a thoracolumbosacral orthosis.
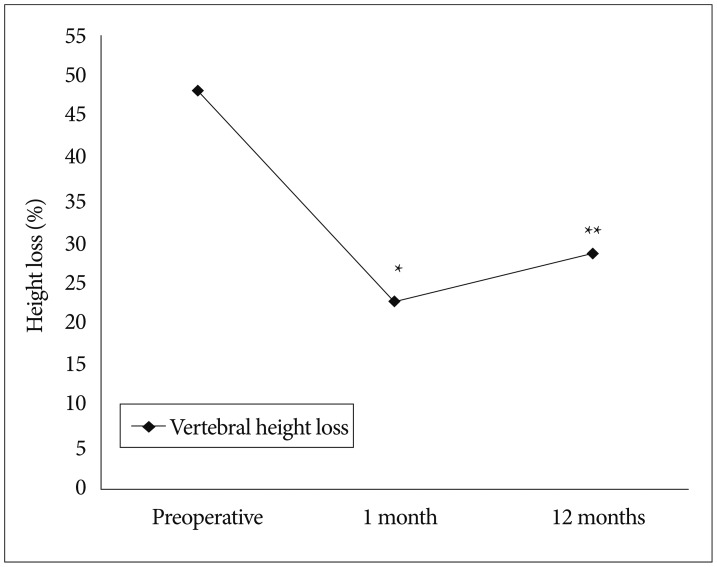
Restoration of vertebral height
Preoperatively, mean vertebral body height loss was 48.2±10.5%. Simple lateral radiographs taken 1 month after the surgical procedure showed that mean vertebral height loss was 22.5±12.4%. Despite significant improvement compared to the preoperative value, mean vertebral height loss was 28.5% at 12 months after surgery (p<0.05). During the follow-up period, vertebral height loss increased by 6.0 (Fig. 2).
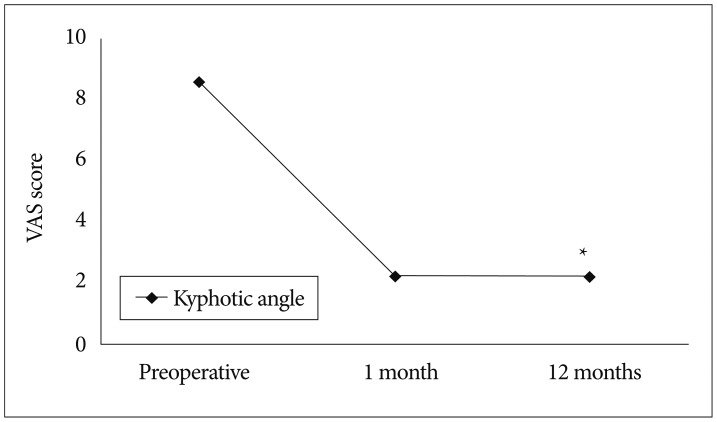
Overall reduction of kyphotic deformity
The kyphotic angle improved significantly from 22.4±4.9° before surgery to 10.1±3.8° at 1 month after surgery. The improved alignment, as observed on a true lateral X-ray, was maintained at 12 months after surgery in spite of some correction loss (Fig. 3).
Clinical outcomes
At 12 months after surgery, all patients achieved a good or excellent outcome according to modified MacNab's criteria. Prior to surgery, the mean pain score (visual analogue scale) was 8.5±1.5. This score decreased to 2.2±2.0 at 1 month after surgery and it was maintained at 12 months after the procedure (Fig. 4).
Asymptomatic cement leakage into the paravertebral area through venous channel was observed in one patient (Fig. 5). However, no major complications such as spinal cord compression, pulmonary embolism, or serious infection were observed in any patient (Fig. 6).

Osteoporotic compression fracture with an intravertebral cleft at the T12 level in a 85-year-old female. A : T2-weighted magnetic resonance image reveals a fluid filled IVC, indicative of Kummell's disease. B and C : Simple radiographs after bone cement-augmented percutneous short segment screw fixation show restored vertebral height and improved kyphotic deformity in spite of cement leakage through venous channel (arrow). D and E : Simple radiographs taken at 12 months after surgery show some aggravation of kyphosis.
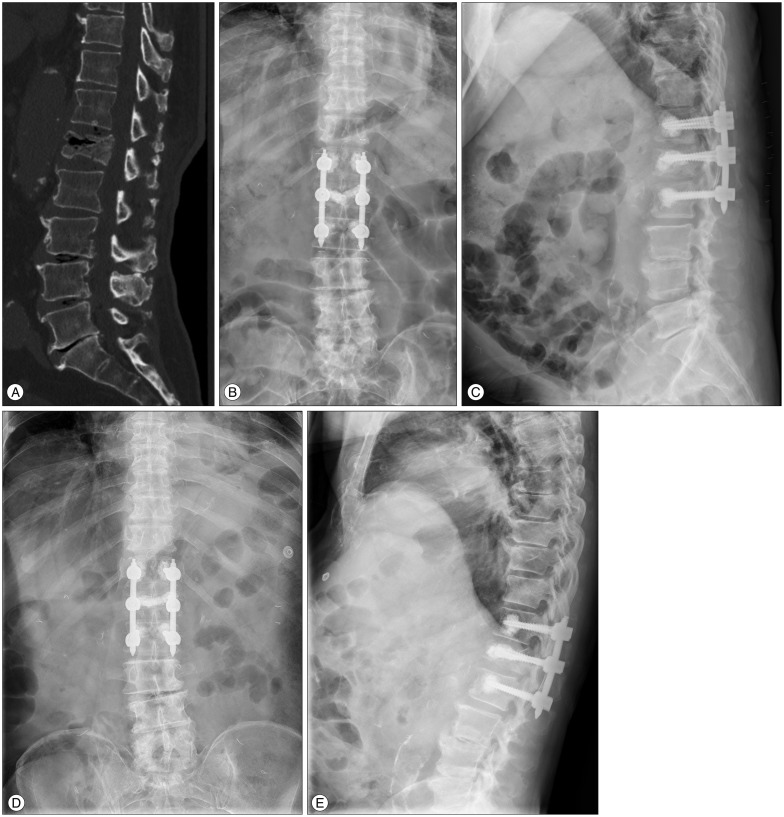
Osteoporotic compression fracture with an intravertebral cleft (IVC) at the L1 level in a 83-year-old male. A : Computed tomography scan shows a gas filled IVC, indicative of Kummell's disease. B and C : Simple radiographs after bone cement-augmented percutaneous short segment screw fixation show restored vertebral height and improved kyphotic deformity. D and E : Simple radiographs taken at 12 months after surgery reveal a well-maintained kyphotic angle.
DISCUSSION
Osteoporotic compression fractures are the most common spinal disorder in elderly patients. Most compression fractures heal within a few weeks or months, and it is believed that in most cases, they do not result in severe clinical problems9).
Kummell's disease, by definition, is a spinal disorder characterized by vertebral body avascular necrosis occurring in a delayed fashion after minor trauma. It evolves according to the following 3 phases : 1) back pain consequent to minor trauma, which progressively subsides, leading to an asymptomatic period; 2) recurrence of pain weeks to months after the initial insult; and 3) appearance of kyphotic spine deformities without any further trauma. All 3 phases must present progressively to lead to the diagnosis of Kummell's disease. A classic finding is the presence of an intravertebral vacuum cleft on plain radiograph, better appreciated on anteroposterior view, on CT or MRI10).
Cases of Kummell's disease with prolonged severe back pain refractory to conservative treatment, with or without neurologic deficits, require surgical treatment. Surgical approaches for Kummell's disease differ between patients with neurological symptoms and those without neurological symptoms. For neurologically impaired patients, the aim of surgery is to decompress the spinal cord, restore the spinal physiological curvature, and maintain spinal stability. The surgical modes include anterior, posterior, or combined anterior and posterior approaches12).
For patients without neurological symptoms, the objective is to eliminate motion at the fracture site and restore the spinal curvature. Certain authors have reported that for Kummell's disease without neurological symptoms, VP or KP achieves good clinical results12). This assumes that pain relief can be expected if the IVC is filled with bone cement and stabilized because unstable fractures and motion within the IVC produce severe and persistent pain.
However, Heo et al.3) assert that bone cement augmentation procedure alone for treating Kummell's disease is associated with recurrent collapse as well as dislodged or fragmented bone cement. They reported that the incidence of recollapse after VP was significantly higher in patients with IVC (28.6%) than in those without IVC (1.2%). Furthermore, Kummell's disease may present with cortical breakage or cord compression, both of which are contraindications for cement augmentation14). Lee et al.9) reported in their clinical study that restored vertebral heights and corrected kyphotic angles were reaggravated, suggesting that vertebral osteonecrosis progresses after a bone cement augmentation procedure alone. They concluded that stabilization by open surgery should be considered as another option for Kummell's disease without neurologic deficits. Patients with Kummell's disease are usually elderly and have severe osteoporotic spines; thus, multisegment fixation with bone fusion by a posterior approach should generally be considered performed. However, this requires extensive dissection of paraspinal muscles of the back and resection of posterior elements of the spine, making it difficult to preserve motion segments. Moreover, elderly patients do not easily tolerate a long level fusion, and failure to support the anterior column can lead to the eventual loss of correction and instrument failure. Therefore, the development of a minimally invasive and effective treatment is required. For Kummell's disease without neurologic deficits, we performed bone cement-augmented percutaneous short segment fixation. This surgical method provides several advantages over long level fixation. The main advantage is that it more effectively preserves motion segments. Second, it minimizes posterior pedicle screw stress through anterior support provided by the vertebral bone cement. Third, it results in immediate pain relief due to stabilization with elimination of donor site pain, reduction in blood loss, and decrease in operation time. However, the preservation of segmental instability obtained by screw fixation may be not easily achieved in Kummell's disease in spite of cement augmentation. Vertebral collapse or screw loosening may occur more frequently after bone cement augmented screw fixation alone. Moreover, these problems may be more significant in patients with severe osteoporosis. As a result, careful and serial follow-up is necessary. Strict postoperative spinal bracing and control of osteoporosis are also helpful for preventing vertebral collapse or screw loosening.
In the current study, we used PMMA for bone cement augmentation, which achieved effective pain relief and good postoperative kyphosis correction. At 12 months after surgery, slight loss of kyphosis corrections were observed compared with measurements at 1 month after the surgery, but the differences were not statistically significant. Thus bone cement augmented percutaneous short segment fixation can be an effective treatment for Kummell's disease without neurologic deficits. However, in spite of acceptable clinical outcome, this study has some limitations. Despite statistically significance, ten patients are rather small group for such a clinical study and twelve months are too short period to confirm our results. Randomized prospective clinical trials with longer observation periods in larger populations are necessary to confirm our results.
CONCLUSION
Bone cement-augmented percutaneous short segment fixation can be useful for the treatment of Kummell's disease without neurologic deficits in elderly. This technique was found to produce excellent pain relief and correction of kyphotic deformities.