Partial Pedicle Subtraction Osteotomy for Patients with Thoracolumbar Fractures : Comparative Study between Burst Fracture and Posttraumatic Kyphosis
Article information
Abstract
Objective
To evaluate the surgical outcomes of partial pedicle subtraction osteotomy (PPSO) in patients with thoracolumbar fractures and compare the outcomes of PPSO for burst fractures with those for posttraumatic kyphosis (PTK).
Methods
From June 2013 to May 2019, 20 consecutive adult patients underwent PPSO for thoracolumbar fractures at the levels of T10 to L2. Of these patients, 10 underwent surgery for acute fractures (burst fractures), and 10 for sequelae of thoracolumbar fractures (PTK). Outcomes of PPSO were evaluated and compared between the groups.
Results
Twenty patients (each 10 patients of burst fractures and PTK) with a mean age of 64.7±11.1 years were included. The mean follow-up period was 21.8±11.0 months. The mean correction of the thoracolumbar angle was -34.9°±18.1° (from 37.8°±20.5°preoperatively to 2.8°±15.2° postoperatively). The mean angular correction at the PPSO site was -38.4°±13.6° (from 35.5°±13.6° preoperatively to -2.9°±14.1° postoperatively). The mean preoperative sagittal vertical axis was 93.5±6.7 cm, which was improved to 37.6±35.0 cm postoperatively. The mean preoperative kyphotic angle at the PPSO site was significant greater in patients with PTK (44.8°±7.2°) than in patients with burst fractures (26.2°±12.2°, p=0.00). However, the mean postoperative PPSO angle did not differ between the two groups (-5.9°±15.7° in patients with burst fractures and 0.2°±12.4° in those with PTK, p=0.28). The mean angular correction at the PPSO site was significantly greater in patients with PTK (-44.6°±10.7°) than in those with burst fractures (-32.1°±13.7°, p=0.04). The mean operation time was 188.1±37.6 minutes, and the mean amount of surgical bleeding was 1030.0±533.2 mL. There were seven cases of perioperative complications occurred in five patients (25%), including one case (5%) of neurological deficit. The operation time, surgical bleeding, and complication rates did not differ between groups.
Conclusion
In cases of burst fracture, PPSO provided enough spinal cord decompression without corpectomy and produced sagittal correction superior to that achieved with corpectomy. In case of PTK, PPSO achieved satisfactory curve correction comparable to that achieved with conventional PSO, with less surgical time, less blood loss, and lower complication rates. PPSO could be a viable surgical option for both burst fractures and PTK.
INTRODUCTION
Thoracolumbar fractures account for about 90% of all spinal column fractures [11,18]. Approximately 10% to 20% of thoracolumbar fractures are burst fractures [10,15,23,28] and can be associated with neurological deficit and kyphotic deformity [31]. The ideal treatment for thoracolumbar burst fractures is still controversial [4,37,39].
Posttraumatic kyphosis (PTK) is a common sequela of acute thoracolumbar fracture and is caused by inappropriate conservative treatment, inadequate immobilization, premature weight bearing, incorrect surgical procedure and fixation, and improper choice of internal fixation devices [33,36]. Pedicle subtraction osteotomy (PSO) is a mainstay of treatment for PTK, producing excellent curve correction [17]. However, PSO is a technically demanding procedure, and the rate of perioperative complications is high.
We performed partial PSO (PPSO) for kyphotic deformity associated with thoracolumbar fractures, which were categorized as burst fractures, and for PTK. The aims of this study are to evaluate the surgical outcomes of PPSO in patients with thoracolumbar fractures and to compare the outcomes of PPSO for burst fractures with those for PTK.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board in Kyung Hee University Hospital at Gangdong (KHNMC 2021-01-005-001). From June 2013 to May 2019, 20 consecutive adult patients underwent PPSO for thoracolumbar fractures at the levels of T10 to L2 [38]. Of these patients, 10 underwent surgery for acute fractures (burst fractures), and 10 underwent surgery for sequelae of thoracolumbar fractures (PTK). Patients who underwent PPSO for infectious disease or for sagittal imbalance other than PTK (degenerative flatback or iatrogenic flatback syndrome) were excluded from this study. Patients who did not complete at least 1 year of followup were also excluded. For patients with burst fractures, the indication for PPSO was unstable fractures (more than a 50% loss of vertebral body height or more than 20° of angulation at the thoracolumbar junction) with compression of the spinal cord or cauda equina by a significant retropulsed fragment. The type of burst fracture was classified using AOSpine thoracolumbar spine injury classification system [13,35]. For patients with PTK, the indication for PPSO was significant local kyphosis (more than 30° angulation) with chronic intractable pain or progressive neurological deficits. All procedures were performed by a single surgeon at one academic institution.
Clinical assessment
Clinical data, including sex, age, time from initial injury to operation, primary or revision surgery status, comorbidities, American Society of Anesthesiologists classification, and mechanisms of injury, were collected retrospectively through medical chart review. Neurological status was measured by American Spinal Cord Injury Association (ASIA) classification [14,21]. The thoracolumbar angle (TL) was measured between the upper endplate of T10 and lower endplate of L2. The angle at the PPSO site was measured between the upper endplate of the adjacent upper vertebra and the lower endplate of the adjacent lower vertebra. The sagittal vertical axis (SVA), which was checked in patients who tolerated the upright position, was measured as the distance from the C7 sagittal plumb line to the perpendicular line running from the superior posterior corner of the S1 vertebral body. The proximal junctional angle was defined as the angle between the caudal endplate of the uppermost instrumented vertebrae to the cephalad endplate of the two supra-adjacent vertebrae above those vertebrae. Proximal junctional kyphosis was defined as a proximal junctional angle of more than 10° and at least 10° greater than the preoperative value. We documented operative details such as the number of fused segments, operation time, estimated blood loss, use of a distal laminar hook, and length of hospital stay. Perioperative complications and postoperative mechanical complications were also evaluated.
Operative techniques
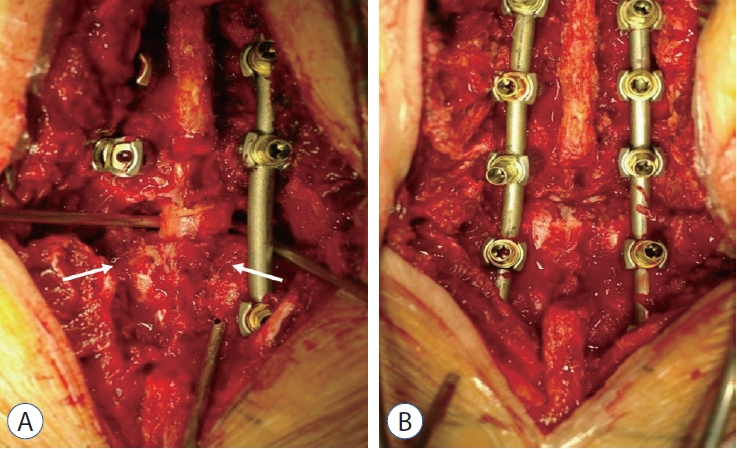
All procedures were performed under intraoperative neurophysiological monitoring. The operative procedure of PPSO was mostly similar to that of conventional PSO [3], however, the major differences were the extent of pedicle removal and of laminectomy. In PPSO, the inferior thin rim of the pedicle was preserved, and the lower half of the lamina, which was connected to the inferior rim of the pedicle, remained intact, without loss of structural integrity. Next, subtotal pediculectomy was performed, and wedge-shaped cancellous bone was removed. During this procedure, the retropulsed bone fragment compressing the spinal cord or cauda equina was also removed. After the bilateral cortical wall of the index vertebra was removed, the osteotomy site was closed gradually with careful inspection for dural kinking or compression (Fig. 1). After the completion of the closure of the osteotomy site, bone-to-bone contact of the posterior element was achieved (Fig. 2).
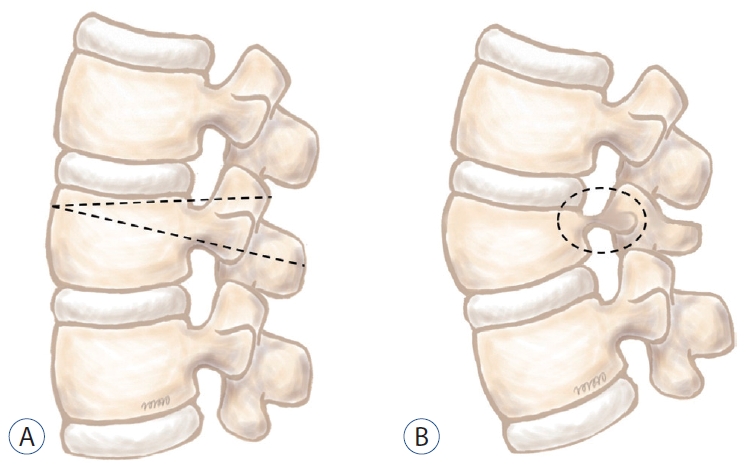
Diagram of partial pedicle subtraction osteotomy. A : After removal of upper part of lamina, vertebral body is resected with wedgeshaped fashion (dotted line). Lower rim of pedicle is preserved. B : After closure of osteotomy site, thin pedicle bridge (dotted circle) and part of the posterior element remained intact, providing enhanced structural integrity and better fusion bed.
Statistical analysis
For statistical analysis, we used SPSS version 22.0 (IBM, Corp., Armonk, NY, USA). The chi-square test was used for dichotomous data analysis. The Mann-Whitney U test was employed to analyze differences in categorical variables. A p-value of less than 0.05 was considered statistically significant.
RESULTS
Baseline characteristics
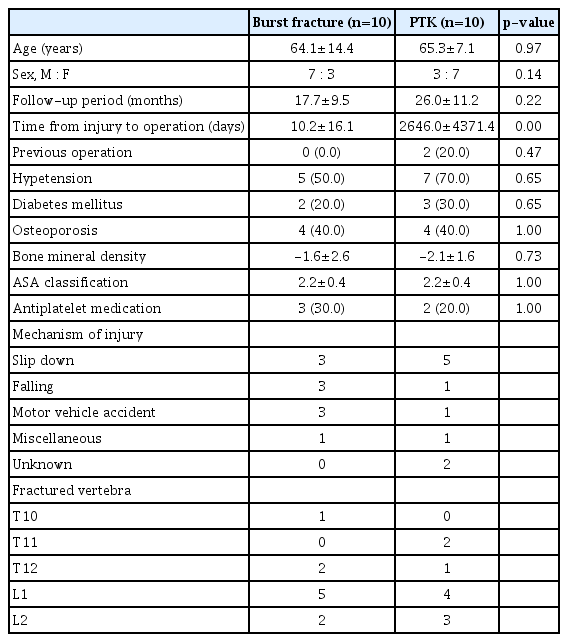
Data from 20 patients (10 men and 10 women) with a mean age of 64.7±11.1 years were evaluated (Table 1). The mean follow-up period was 21.8±11.0 months. The most common mechanism of injury was slip down (n=8), followed by motor vehicle accident (n=4) and falling (n=4). The level most commonly fractured was L1 (n=9), followed by L2 (n=5) and T12 (n=3). For 10 patients with burst fractures, most common fracture type was A4 (n=6), followed by B2 (n=3) and B1 (n=1), according to AOSpine thoracolumbar spine injury classification system.
Ten patients had burst fractures, and 10 had PTK. Age, sex, length of follow-up, and previous operation history did not differ significantly between the two groups. However, the mean time from initial injury to operation was significantly shorter in patients with burst fractures (10.2±16.1 days) than in patients with PTK (2646.0±4371.4 days; p=0.00). Comorbidities, including hypertension, diabetes mellitus, osteoporosis, and bone mineral density, did not differ significantly between the two groups nor did American Society of Anesthesiologists classification or proportion of patients taking antiplatelet medication.
Radiographic outcomes
The radiographic outcomes are summarized in Table 2. All patients achieved solid fusion at the osteotomy site, in both groups. The mean preoperative TL was 37.8°±20.5°, which was corrected to a mean of 2.8°±15.2°. The mean correction of the TL was -34.9°±18.1°. The mean angular correction at the PPSO site was -38.4°±13.6° (from 35.5°±13.6° preoperatively to -2.9°±14.1° postoperatively). The mean preoperative SVA was 93.5±64.7 cm, which was improved to 37.6±35.0 cm postoperatively (Figs. 3 and 4).

A : A 60-year-old man presented with complete paraplegia after falling from fourstory building. Initial X-ray revealed L1 burst fracture with kyphotic deformity (26.0°). B : Postoperative X-ray at 3 months showed correction of local kyphosis to -14.0°. Note the remained thin pedicle after partial pedicle subrtraction osteotomy (arrow). C : Solid fusion was achieved at the last follow-up (postoperative 2 years) without loss of correction. D and E : Preoperative and posteoperative computed tomography showed removal of retropulsed fragment and decompression of spinal canal.
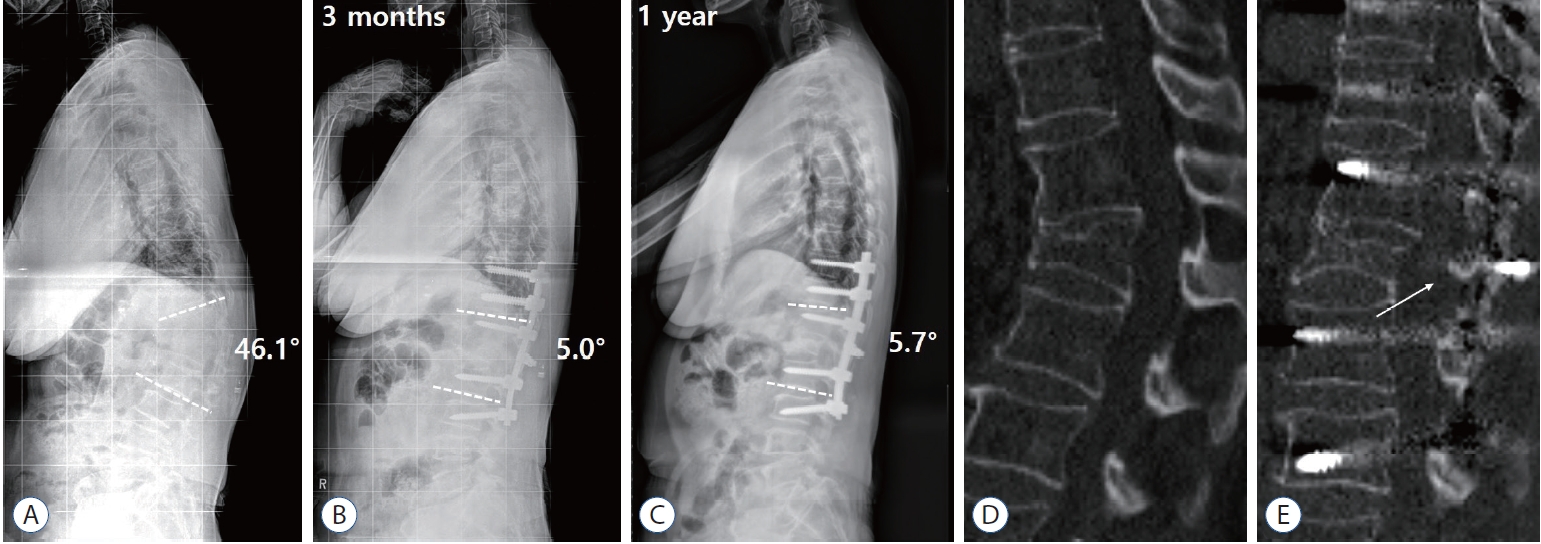
A : A 58-year-old woman presented with 10-year history of persistent pain on back and lower extremities after slip down. She also complained of progressive stooped posture on walking. Preoperative X-ray showed posttraumatic kyphosis at L1 (46.1°). B : Postoperative X-ray at 3 months showed improvement of kyphotic deformity (5.0°) with good sagittal alignment. C : Postoperavie X-ray at the last follow-up (postoperative 1 year) did not show loss of correction or junctional kyphosis. D : Preoperative computed tomography (CT) showed kyphotic deformity due to old trauma. E : Postoperative CT showed solid arthrodesis of osteotomized vertebra with part of intact posterior element (arrow).
The mean preoperative TL was significantly greater in patients with PTK (48.5°±16.7°) than in patients with burst fractures (27.0°±18.7°; p=0.02). However, the postoperative TL did not differ between patients with burst fractures and those with PTK (0.9°±17.5° vs. 4.7°±13.0°; p=0.17). The mean preoperative kyphotic angle at the PPSO site was significant greater in patients with PTK (44.8°±7.2°) than in patients with burst fractures (26.2°±12.2°; p=0.00). However, the mean postoperative PPSO angle did not differ between the two groups (-5.9°±15.7° in patients with burst fractures and 0.2°±12.4° in those with PTK; p=0.28). The mean angular correction at the PPSO site was significantly greater in patients with PTK (-44.6°±10.7°) than in those with burst fractures (-32.1°±13.7°; p=0.04). The mean postoperative SVA did not differ between the two groups (p=0.90).
Surgical outcomes
The operative details are summarized in Table 3. The mean number of instrumented vertebrae was 5.7±1.0. In nine patients (47.4%), distal laminar hooks were applied to augment distal screws. Among all patients, the mean operation time was 188.1±37.6 minutes, the mean amount of surgical bleeding was 1030.0±533.2 mL, and the mean length of hospital stay was 24.0±9.2 days.
Patients with burst fractures showed no significant differences from patients with PTK with regard to the number of instrumented vertebrae (5.6±1.0 vs. 5.8±1.0; p=0.63), application of distal hooks (55.6% vs. 40.0%; p=0.66), operation time (187.3±40.8 minutes vs. 188.9±36.5 minutes; p=0.93), amount of surgical bleeding (1070.0±537.6 mL vs. 990.0±554.7 mL; p=0.74), or length of hospital stay (21.3±9.8 days vs. 26.6±8.3 days; p=0.12).
Surgical complications
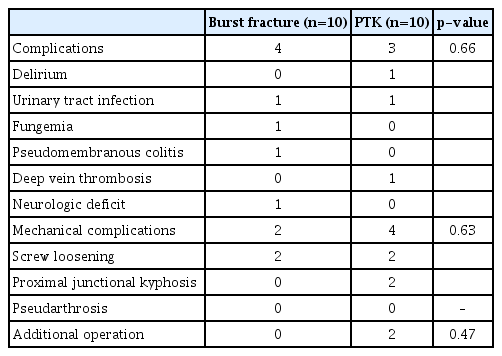
Seven cases of perioperative complications occurred in five patients (25%). These complications included neurological deficit in one patient (5%) with PTK (Table 4). Of the patients with burst fractures, one had a urinary tract infection, one had fungemia, one had pseudomembranous colitis, and one had deep vein thrombosis. Of the patients with PTK, one had delirium, one had a urinary tract infection, and one had neurological deficit. The complication rates among patients with burst fractures and among those with PTK did not differ significantly (p=0.66).
Postoperative mechanical complications included four cases of screw loosening (in two patients with burst fractures and two with PTK) and two cases of proximal junctional kyphosis (both in patients with PTK). Pseudarthrosis did not occur. The rates of mechanical complications in the two groups did not differ (p=0.63).
Two patients with PTK required additional surgery postoperatively. One of these patients suffered from postoperative weakness in both lower extremities. Postoperative computed tomography showed a remnant bone cement material within the anterior spinal canal at the PPSO site. After the bone cement material was removed during revision surgery, leg strength was improved, and the patient was able to walk independently with some aid (ASIA class D). The other patient complained of persistent back pain at the operation site over the cross-link. After the cross-link was removed, the back pain resolved. No patients with burst fractures required additional surgery. The proportion of patients who underwent additional surgery was not statistically different between groups (p=0.47).
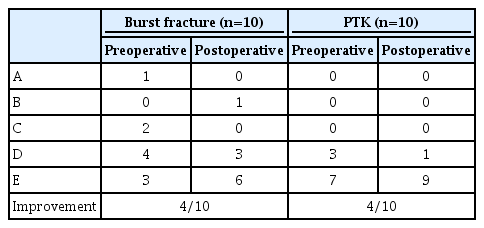
Neurological outcomes
Four patients (40%) in each group showed improved neurological status postoperatively (Table 5). In one patient with PTK, neurological status deteriorated postoperatively (ASIA class E preoperatively and ASIA class D postoperatively), but no patient with burst fractures showed neurological deterioration. The two groups showed no significant differences in preoperative and postoperative ASIA classes (p=0.06 and p=0.25, respectively).
DISCUSSION
We analyzed the radiographic and clinical results of PPSO performed on patients with burst fractures and PTK. PPSO produced satisfactory correction of kyphosis and clinical outcomes in both groups of patients. The degree of kyphotic deformity, measured by preoperative TL and PPSO angles, was greater in patients with PTK than in those with burst fractures, but the final radiographic results were equally satisfactory in both groups. The direct comparison of outcomes for burst fractures and PTK may be questionable. However, with regard to kyphotic deformity, both pathological entities are on the same spectrum of PTK, as described by Munting [29] Indeed, all patients with burst fractures showed a significant degree of local kyphosis (26.2°±12.2°). This means that sagittal realignment is as important as neural decompression and stabilization.
In surgery for burst fractures, an anterior approach, a posterior approach, and a combined (circumferential) approach may be used [12,22,27]. Although the mode of treatment is controversial, corpectomy would be considered regardless of the approach in cases of severe spinal cord compression and neurological deficit [26,31]. The advantages of the anterior approach are good exposure for the direct decompression of the spinal canal, good reconstruction of the anterior and middle portions of the spinal column, provision of solid fusion, and better establishment of sagittal realignment [31]. However, this approach entails a higher risk of injury to the visceral structure, and circumferential reconstruction is mandatory for the injury of the posterior tension band [9,15]. The posterior stabilization technique is familiar to spine surgeons, but it is harder to achieve adequate sagittal realignment with this approach than with the anterior approach, and postoperative progression of kyphosis can occur [5,32].
We suggest several advantages of PPSO over anterior or posterior corpectomy in cases of burst fractures. First, through poster column shortening, the amount of correction that we achieved (32.1°±13.7° at the PPSO site) was greater than that previously reported for corpectomy (ranging from 10° to 20°) [26,31,32]. Rather, surgeons should be careful not to overcorrect the osteotomy site, because burst fracture can often be highly unstable. Second, problems associated with the posterior approach, such as loss of correction or instrument failure, could be minimized by solid arthrodesis through complete closure of the posterior column [5,32]. Finally, the complications associated with corpectomy, including visceral injury (during anterior corpectomy) or root injury (during posterior corpectomy), can be avoided with PPSO. Although the amount of kyphotic deformity caused by burst fractures is generally less than that of PTK, iatrogenic flatback deformity can progress as a result of insufficient sagittal correction of burst fractures [5,25,32]. Therefore, PPSO is an alternative to corpectomy in the treatment of burst fractures accompanied by significant sagittal malalignment and spinal cord compression.
The mainstay of surgical treatment for PTK is posteriorbased osteotomy, and PSO became the principal means of correction [33]. PSO is a powerful method of treating rigid kyphotic deformity, and in most previous studies, investigators reported an amount of correction ranging from 30° to 40° [2,6,19,30]. Despite such powerful correction, however, PSO is still a technically demanding procedure for spine surgeons. In this study, PPSO took less surgical time than did conventional PSO. Furthermore, blood loss was decreased, and the rates of perioperative complications were lower [2,7,16,41]. Furthermore, by remaining a thin shell of lower margin of pedicle, satisfactory curve correction comparable to PSO could be obtained. During PSO, complete excision of pedicle (especially medial and lower margin), poses possibility of root injury and dural tear. Authors think that remaining cortical shell of pedicle could decrease the risk of neural injury without significant loss of correction amount. Moreover, because a thin cortical bridge connected the osteotomized vertebral body to the posterior element, PPSO provided better structural stability for the osteotomized vertebra for solid arthrodesis. Complete closure of the posterior element, which is sometimes not possible in PSO with wide laminectomy [20], enhances fusion, and this is another advantage of PPSO because total laminectomy is unnecessary. Therefore, we believe that PPSO is an alternative to PSO in cases in which total laminectomy is not required for extensive spinal cord decompression.
Because conventional PSO is a technically demanding procedure, high rates of perioperative complications have been reported in previous studies [3,6,8,19]. Daubs et al. [7] reported that of 65 patients, 25 (38.4%) suffered from minor or major perioperative complications, including neurologic deficits in four (6.2%). Auerbach et al. [1] demonstrated that 38% (33/87) and 53% (46/87) of PSO procedures were associated with major and minor complications, respectively. In our study, PPSO was associated with a lower rate of perioperative complications (25%) than in previous studies of conventional PSO. Nevertheless, several studies of PSO performed exclusively for PTK demonstrated lower complication rates, ranging from 5% to 15% [25,30,40,42]. However, the mean ages in those studies were the 40s, as opposed to 64.7 years in this study. Because the older age is a well-known risk factor for perioperative complications of deformity surgery [24,34], we believe that different patients’ characteristics may account for the lower rates of perioperative complications in those studies.
We have described our experiences of managing burst fractures and PTK with PPSO. In cases of burst fracture, PPSO provided enough spinal cord decompression without corpectomy and produced sagittal correction superior to that achieved with corpectomy. In cases of PTK, PPSO achieved satisfactory curve correction comparable with that achieved with conventional PSO, with less surgical time, less blood loss, and lower complication rates. Moreover, the retained thin pedicle bridge and part of the posterior element enhanced structural integrity and provided better fusion until solid arthrodesis was performed.
This study is limited by its retrospective nature without randomization. The small sample size and relatively short period of follow-up were other limitations. Lastly, this study did not contain patient-reported outcomes such as Scoliosis Research Society questionnaire or Oswestry disability index. This is because such questionnaire could not be conducted in most patients with burst fractures, who required urgent surgical treatment. Therefore, further study with a larger population would be necessary to validate our findings.
CONCLUSION
Patients with thoracolumbar injuries, categorized as burst fractures and PTK, underwent surgery with PPSO. In cases of burst fracture, PPSO provided enough spinal cord decompression without corpectomy and produced sagittal correction superior to that achieved with corpectomy. In case of PTK, PPSO achieved satisfactory curve correction comparable to that achieved with conventional PSO, with less surgical time, less blood loss, and lower complication rates. Moreover, the retained thin pedicle bridge and part of the posterior element enhanced structural integrity and provided better fusion bed until solid arthrodesis was performed. PPSO could be a viable surgical option for both burst fractures and PTK.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
This type of study does not require informed consent.
AUTHOR CONTRIBUTIONS
Conceptualization : HYC, DJJ
Data curation : HYC
Formal analysis : HYC
Methodology : HYC
Project administration : DJJ
Visualization : HYC
Writing - original draft : HYC
Writing - review & editing : HYC, DJJ