Chronic Lymphocytic Inflammation with Pontine Perivascular Enhancement Responsive to Steroids with a Significant Elevation of β-2 Microglobulin Levels
Article information
Abstract
Chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) is a relapsing-remitting disorder for which steroid administration is a key to control the progression. CLIPPERS can exhibit radiological features similar to malignant lymphoma, whose diagnosis is confounded by prior steroid administration. We report a case of CLIPPERS accompanied by abnormal elevation of β-2 microglobulin in the cerebrospinal fluid (CSF). A 62-year-old man started to experience numbness in all fingers of his left hand one year ago, which gradually extended to his body trunk and legs on both sides. Magnetic resonance imaging demonstrated numerous small enhancing spots scattered in his brain and spinal cord. CSF levels of β-2 microglobulin were elevated; although this often indicates central nervous system involvement in leukemia and lymphoma, the lesions were diagnosed as CLIPPERS based on the pathological findings from a biopsy specimen. We emphasize the importance of biopsy to differentiate between CLIPPERS and malignant lymphoma because the temporary radiological response to steroid might be the same in both diseases but the treatment strategies regarding the use of steroid are quite different.
INTRODUCTION
Since chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS) was first reported in 20107), approximately 50 cases have been described in the literature. Despite several recent case reports371012), the clinical presentation, methods of diagnosis, and pathogenesis of CLIPPERS have not been fully elucidated. Clinical symptoms frequently include a variety of focal neurological deficits1011), which complicates early diagnosis. There are no specific methods, such as serum chemistry or cerebrospinal fluid (CSF) examination, for diagnosis of CLIPPERS. Imaging studies are not definitive, particularly when initial magnetic resonance (MR) images show minimal abnormal findings12). These concerns render the diagnosis of CLIPPERS difficult. Here we report a case of CLIPPERS in which we experienced some diagnostic difficulties. We initially suspected malignant lymphoma because the level of β-2 microglobulin in the CSF were significantly elevated. A biopsy played a critical role in diagnosing CLIPPERS.
CASE REPORT
A 62-year-old man with no past medical history started to experience numbness in all fingers on his left hand one year ago. His numbness gradually extended to his fingers and lips on his right side, and ultimately to his body trunk and legs on both sides. He visited a neurologist at our institution. A detailed neurological examination showed bilateral facial numbness, mild dysarthria, abnormal feeling of tightness in the Th4 level, and mild bilateral cerebellar ataxia. No other cranial nerve deficits were noted. He had no motor paresis, and deep tendon reflexes were normal and symmetrical. Pathological reflexes, including Babinski and Chaddock reflexes were absent. A physical examination revealed no systemic abnormalities such as lymph node swelling.
A blood test revealed a normal complete blood count, no abnormal biochemistry, and no autoimmune antibodies, including antinuclear antibody, antineutrophilic cytoplasmic antibody, antithyroid peroxidase antibody, and anti-phospholipid antibody. Epstein-Barr virus was negative, and serum lactate dehydrogenase (LDH) levels were within normal limits. Analysis of the CSF demonstrated a slight increase in cell counts 22/3 and normal concentrations of protein (63 mg/dL) and glucose (69 mg/dL). However, it also showed a remarkable increase in the β-2 microglobulin level (up to 4144 µg/L). The oligoclonal band was not identified and CSF cytology was class I. CSF levels of LDH were slightly elevated (34 IU/L, normal ≤25). Amounts of immunoglobulins were also elevated : IgG, 11.7 mg/dL (0.2-4.0); IgA, 1.6 mg/dL (0.1-0.6); IgM, 0.8 mg/dL (0.03-0.06). MR images demonstrated diffuse abnormal small spotty lesions in the pons and cerebellum that had low intensity on T1-weighted images (Fig. 1A) and high intensity on T2-weighted images (Fig. 1B). T1-weighted images with gadolinium showed that the these lesions were enhanced (Fig. 1C). A few solitary enhanced spots were also identified in the deep white matter of the temporal and frontal lobes (Fig. 1D, E). Similar enhanced lesions were present in the spinal cord, as well (Fig. 1F). The size of the lesions in the pons and cerebellum, and spinal cord ranged from 1 mm to 5 mm while that of the spinal lesions were slightly larger. They were sparsely distributed in some areas and formed clusters in other areas. At this point, possible diagnoses included malignant lymphoma, intravascular malignant lymphoma, glioma, metastatic tumor, cerebrovascular angiitis, multiple sclerosis, sarcoidosis, central nervous system Behcet's disease, viral encephalitis, and rare pathologies such as CLIPPERS. Because multiple enhancements along the surface and the inside of the brain stem appeared to indicate perimedullary venous dilation, we performed a cerebral and spinal angiogram to eliminate cerebrovascular diseases such as a dural arteriovenous fistula. The angiogram did not detect any apparent abnormalities.

A series of brain MR images demonstrating enhancing lesions. The lesions were hypointense on T1-weighted images (A) and hyperintense on T2-weighted images (B). Small enhancing spots were distributed in the pons and cerebellum (C), temporal (D), and frontal (E) lobes, and spinal cord (F). Biopsy specimen was obtained from the lesions in the right cerebellum (G, arrow).
During the course of these examinations, the patient's symptoms rapidly progressed within a week, and bilateral lower cranial nerve dysfunction occurred. This dysfunction caused severe dysarthria, dysphagia, and respiratory distress that required emergency intubation followed by tracheostomy. Because some immunological disease was suspected, we had a careful discussion with neurologists and hematologists regarding the efficacy of steroid as a diagnostic therapy. However, use of steroid was considered inappropriate because malignant lymphoma had not been excluded. Therefore, we biopsied the enhanced cerebellar mass to obtain the correct diagnosis (Fig. 1G). With the aid of an intraoperative navigation system, a 1.5-cm square block was prepared. Pathological examination of the block showed that small lymphocytes had invaded all layers of the blood vessels in the white matter, whereas the structures of the cerebellar cortex and white matter were preserved (Fig. 2A). Closely aggregated cell invasions containing scattered histiocyte-like cells and plasma cells were observed in the vessel walls and the adjacent brain parenchyma. Immunohistochemistry showed a mixture of T cells and B cells (Fig. 2B, C), with dominancy of T cells in the brain parenchyma and of B cells in the perivascular areas. CD4-positive T cells were more prominent than CD8-positive T cells (Fig. 2D, E). These findings are consistent with the characteristics of CLIPPERS. The absence of monoclonal proliferation of lymphocytes and of small RNAs derived from Epstein-Barr virus support this diagnosis.
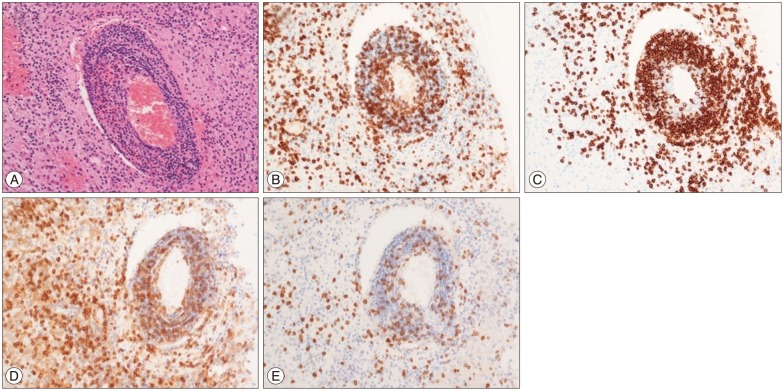
Photomicrographs of sections from the biopsy specimen. A : Small lymphocytes invaded all layers of the blood vessels in the white matter. B : The invasion of CD3-positive cells was noted. C : CD20-positive cells were dominantly distributed in the perivascular areas. D and E : CD4-positive T cells (D) were more prominent than CD8-positive T cells (E). Original magnifications are ×100 (A) and ×200 (B-E).
Postoperatively, based on the diagnosis, the patient received steroid therapy (two courses of 500 mg intravenous methylprednisolone for five consecutive days). Oral prednisone was initiated at 50 mg/day and tapered to 5 mg/day. Apparent improvement was noted on MR images obtained two months after steroid administration. The patient's neurological deficits showed gradual improvement over the course of three months. After six months of rehabilitation, he was discharged with a slight gait disturbance. He was neurologically intact on prednisone 5 mg/day on a 1.5-year follow-up with no sign of recurrence (Fig. 3).
DISCUSSION
CLIPPERS is a recognized clinical entity first reported in 2010 by Pittock et al.7). Because of the paucity of data, its diagnostic criteria have not been fully established3). CLIPPERS is often indirectly diagnosed by excluding central nervous system lymphoma, cerebrovascular disease, and other immunological disorders such as angiitis10). Radiological features are important in the diagnosis of CLIPPERS. Pittock et al.7) summarized eight cases of CLIPPERS, in which they observed punctate and curvilinear enhancements peppering the pons and extending variably into the medulla and midbrain. Because CLIPPERS often involves the cerebellar region, as observed in our case, Simon et al.10) proposed renaming the syndrome "chronic lymphocytic inflammation with 'pontocerebellar' perivascular enhancement responsive to steroid". However, CLIPPERS is accompanied by supratentorial enhancing lesions as well in 60-75% of cases, and enhanced lesions are frequently dispersed throughout the CNS1011). Because CLIPPERS can occur in any region of the CNS, its symptoms and their ways of progression can widely vary. Although gait ataxia and diplopia that gradually develop are the most common symptoms in the literature, our case shows that serious respiratory dysfunction that requires a tracheostomy can occur due to rapidly progressing bulbar and/or pseudobulbar palsy.
It is critical to differentiate malignant lymphoma from CLIPPERS because the treatment strategies are completely different. CLIPPERS is a relapsing-remitting disorder whose progression is controlled by steroid administration12). Because the effect of the prolonged corticosteroid therapy to prevent the relapse is largely unknown11), long-term follow-up is necessary for CLIPPERS.
On the other hand, steroid administration for malignant lymphoma based on misjudgment for CLIPPERS might complicate diagnosis of malignant lymphoma, which can result in nonperformance or serious delay of requisite chemotherapy or radiation. Despite the importance of proper diagnosis, there are no specific serological or viral markers in the peripheral blood or CSF that can help diagnose CLIPPERS. While CSF tests for β-2 microglobulin, LDH isozyme 5, and immunoglobulin heavy chain re-arrangement are useful for diagnosis of CNS lymphoma9), their usefulness for diagnosis of CLIPPERS is largely unknown. In our case, we had some difficulty excluding the possibility of malignant lymphoma because CSF levels of β-2 microglobulin were elevated. Although such increases can occur nonspecifically156), they often indicate CNS involvement in leukemia and lymphoma4). Buttmann et al.3) reported a case of CLIPPERS in which β-2 microglobulin levels were normal, but no other reports on CLIPPERS include β-2 microglobulin measurements. Based on our case, accumulation of β-2 microglobulin in the CSF should not exclude the possibility of CLIPPERS. Although innovative techniques such as proteomics8) and microRNA analysis of the CSF2) may be useful in distinguishing lymphoma from CLIPPERS, Pittock et al.7) states that biopsy results are fundamental if biopsies can be performed safely8). Our case highlights the importance of pathological confirmation to differentiate CLIPPERS from CNS lymphoma.
CONCLUSION
Abnormal elevation of β-2 microglobulin in the CSF can be observed in CLIPPERS as well. Biopsy to differentiate between CLIPPERS and malignant lymphoma is essential because the temporary radiological response to steroid might be the same in both diseases but the treatment strategies regarding the use of steroid are quite different.
Acknowledgements
The authors thank Dr. Atsushi Abe of Department of Radiology, Saitama Medical Center/University, for his advice on radiological examinations and Drs. Shinya Narukawa and Kyoichi Nomura of Department of Neurology, Saitama Medical Center/University, for their critical reviewing of the manuscript.
