Carpal Tunnel Syndrome Caused by Lipofibromatous Hamartoma of the Median Nerve
Article information
Abstract
Lipofibromatous hamartoma (LFH) is a rare tumor of the peripheral nerves, which usually involves the median nerve. The authors reported on two rare cases of carpal tunnel syndrome due to LFH of the median nerve. A 49-year-old female patient complained of the mass and symptoms consistent with LFH. Magnetic resonance imaging (MRI) showed typical LFH findings. The symptoms were successfully ameliorated with carpal tunnel release and external neurolysis. A 37-year-old female patient complained of weakening thumb abduction and the mass where the MRI showed atypical findings. Opponensplasty and debulking operations were performed after which thumb abduction was improved; however, neurological sequelae remained. LFH of the median nerve is managed on a case-by-case basis as treatment guidelines are not very clearly defined yet. However, the less invasive treatment such as carpal tunnel release and external neurolysis than more aggressive surgical treatment should be recommended as a treatment option.
INTRODUCTION
Lipofibromatous hamartoma (LFH) is a rare tumor of peripheral nerves that is characterized by an excessive proliferation of fibroadipose tissue, which infiltrates the epineural and perineural elements of peripheral nerves. The most commonly affected nerve is the median nerve, but it is also known to affect the radial nerve, ulnar nerve, and brachial plexus in the upper extremities [2]. LFH is considered congenital in origin and has been commonly associated with macrodactyly and other conditions at birth [4]. A few cases of LFH have been reported since Mason first described a case of LFH occurring in the median nerve in 1953 [4,8,11-13]. However, the cause and treatment for LFH have not yet been clearly defined. We reported two cases of secondary carpal tunnel syndrome (CTS) due to LFH on the median nerve.
CASE REPORT
Case 1
A 49-year-old woman presented to the hospital with numbness of the thumb, index, and middle fingers of the right hand without any history of trauma. The patient also complained of masses in the palm and wrist, which were first observed 7 years ago after an injection treatment for the numbness of the hand, and they gradually increased in size. The patient described the injection site as 2 cm above the wrist crease, but she could not remember the components of the injection. Physical examination revealed a mass of 2×3 cm in the thenar area of the right palm and another mass of 3×4 cm in the proximal region of the right radiocarpal joint (Fig. 1). The shape and size of the fingers were all normal. Hypoesthesia of the thumb, index finger, and middle finger was observed. Although Tinel’s sign of the carpal tunnel was positive, no atrophy of the thenar muscle was observed.
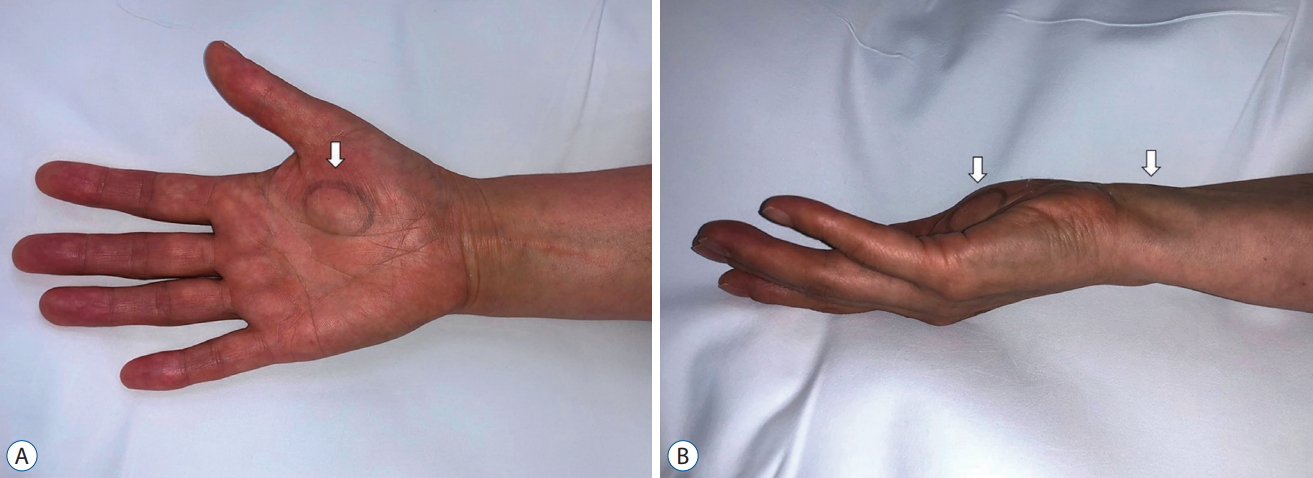
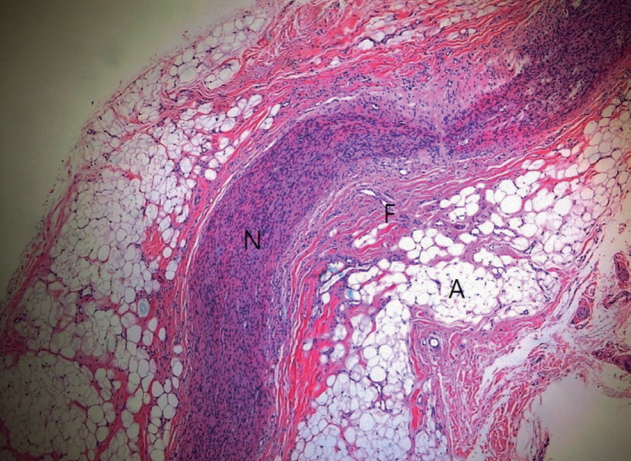
The clinical photographs (A and B) show a mass from the distal forearm to the palm of the hand (white arrows).
Radiographs did not reveal clear shading of soft tissue masses and no abnormalities were observed in the bones and the adjacent joints. Electromyogram tests to identify neurological abnormalities indicated CTS of a moderate degree in the American Association of Electrodiagnostic Medicine (AAEM) classification. Magnetic resonance imaging (MRI) was conducted to determine the appearance of the mass. The coronal MRI scan revealed fusiform swelling of the median nerve from the distal forearm to the distal palmar area, and the carpal tunnel median nerve was pressed into an hourglass-shape by the transverse carpal ligament. In the axial cut, the mass was shown as an oval shape, and the T1-weighted image had a “coaxial cable-like” appearance due to a low-intensity nerve fascicle within the high-intensity adipose tissues. In the coronal and sagittal cuts, the mass had a “spaghetti-like” image (Fig. 2).
Magnetic resonance imaging findings. A : The axial T1-weighted image shows the displacement of the flexor tendon and palmar protrusion of the flexor retinaculum due to an enlarged median nerve (white arrow). B and C : The sagittal and coronal sections demonstrate the fusiform or hourglass enlargement of the median nerve (white arrows) with low-signal intensity nerve bundles embedded in hyperintense adipose tissue.
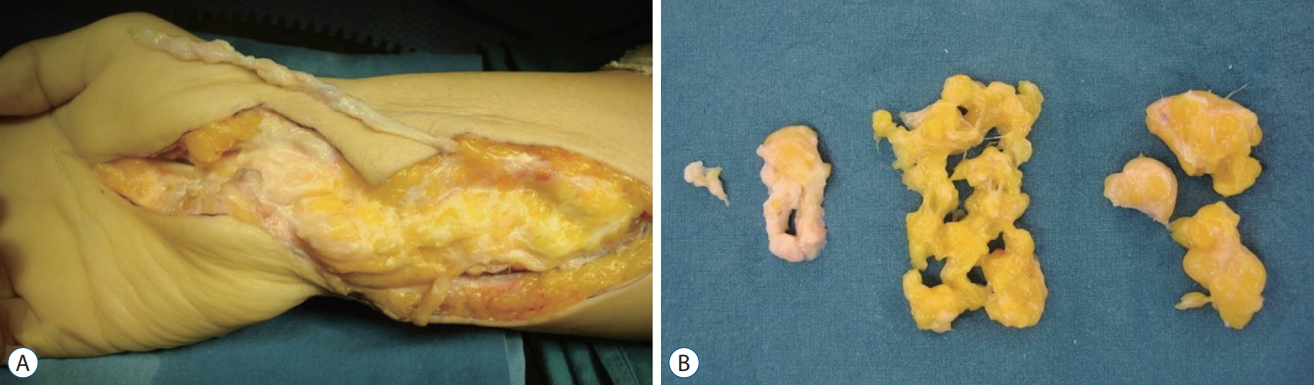
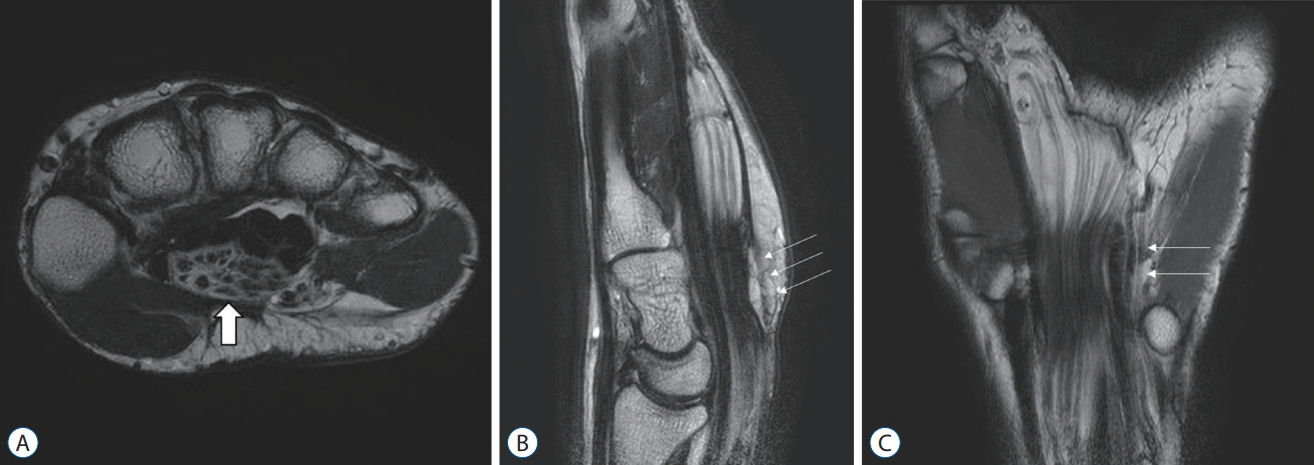
Due to the tumor being on the median nerve and the resulting diagnosis of secondary CTS, surgical treatment was decided. A 12-cm zigzag longitudinal incision was made alongside the mass, from the distal forearm to the palmar area. After dissecting the subcutaneous tissues, the mass was identified distally along the normal median nerve in the proximal region. No infiltrations into the surrounding tissues were observed. The outer membrane of the mass was formed along the epineurium of the median nerve and a bright yellow sausage-like mass was exposed. The mass was severely compressed in the carpal tunnel. In the area of carpal tunnel, we made an additional curved incision parallel to the thenar crease approximately 6 cm in length. The transverse carpal ligament was carefully released along the ulnar border, avoiding damage to the median nerve and its recurrent branch. We tried to make an incision on the epineurium and perform internal neurolysis, but the mass and median nerve could not be separated (Fig. 3). A small portion of the epineurium was excised for biopsy. The final histological examination confirmed the diagnosis of LFH (Fig. 4). Numbness disappeared after the operation. There was no change in the size of the mass throughout the 12-month post-operative follow-up examinations, but the patient was satisfied with the absence of numbness.
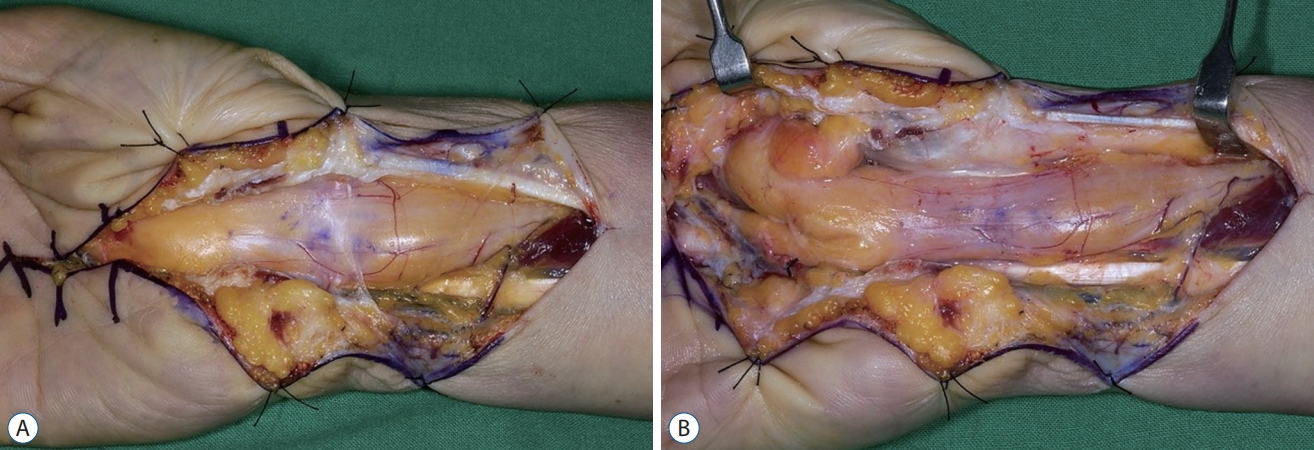
Intraoperative photographs. A : The enlarged median nerve with fibroadipose tissue proliferation. B : After external neurolysis.
Case 2
A 37-year-old woman was admitted due to muscle weakness in her left thumb and a mass in her left forearm. The patient reported having had surgery, the details of which she could not remember, on her left wrist when she was a child. Since then, she had developed thumb abduction weakness and experienced dysesthesia. Physical examination confirmed the 3 cm post-surgical incision wound alongside the right palmer side of the thenar crease. Severe atrophy of the thenar muscle and a 4.5×10 cm mass on the palmar side of the distal forearm was observed. The left thumb, index, and middle fingers had hypoesthesia. Tinel’s sign test was positive on the carpal tunnel. There was a weakness of thumb opposition.
Simple radiography showed an increased shading of soft tissues. An electromyogram test indicated CTS of a severe degree in the AAEM classification. An MRI was performed to confirm the mass properties. In the sagittal and coronal section of the MRI scan, ‘fusiform swelling’ of the median nerve was observed. In addition, in the axial T1-weighted image at the distal forearm level, a nerve fascicle with low signal intensity was located eccentrically inside the mass, and the fat tissue with high signal intensity protruded from the nerve and expanded to adjacent muscles (Fig. 5).
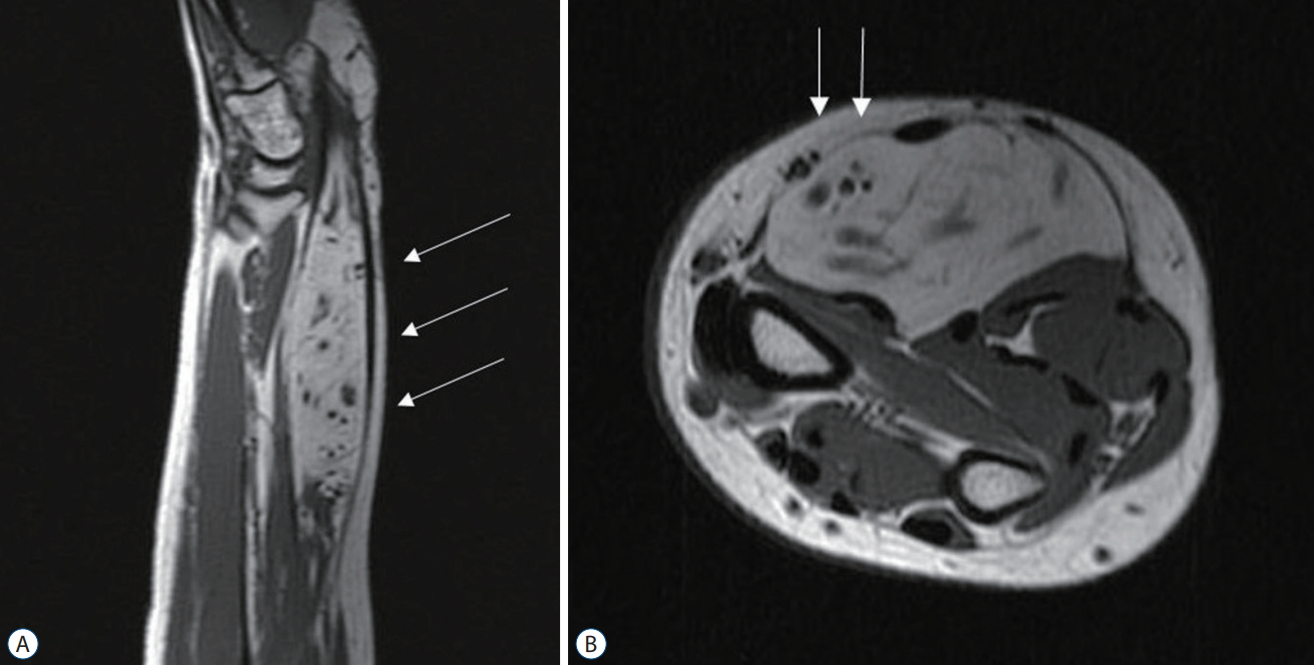
Magnetic resonance imaging finding. A : The sagittal section demonstrates fusiform enlargement of the median nerve (white arrows). B : The axial T1-weighted image shows the distribution of low-intensity nerve bundles was eccentric (white arrows).
Surgical treatment was determined under the diagnosis of severe CTS caused by a mass in the median nerve resulting in a disorder of thumb opposition. A 14-cm zigzag longitudinal incision was made alongside the mass, and then peeled to expose the palmar fascia. The palmaris longus tendon was dissected up to the midpalmar portion, while leaving the palmar aponeurosis attached for the longest length possible. After dissecting the subcutaneous tissues, the mass was identified distally along the normal median nerve in the proximal region. In the area of carpal tunnel, we made an additional curved incision parallel to the thenar crease. The transverse carpal ligament was carefully released along the ulnar border, avoiding damage to the median nerve and its recurrent branch. Care should be taken to avoid injury to the superficial palmar artery arch. Then, an internal neurolysis and debulking operation was performed to remove the yellow tumor tissue as much as possible by peeling off the mass while paying special attention not to damage nerve fascicles. Subsequently, the palmaris longus tendon was extruded through the subcutaneous tunnel to the radial side of the metacarpophalangeal joint of the thumb and sutured to the abductor pollicis brevis attachment (Fig. 6). While the thumb was abducted, the first metacarpal and the metacarpal bone were fixed with Kirschner wire and splint was applied. The final histological examination of the resected tumor tissue confirmed the diagnosis of LFH. After the surgery, the patient wore a thumb splint for 4 weeks and a brace for 4 weeks. The Kirschner wire was removed 8 weeks after the surgery. No increase in the size of the mass showed 10 months after the surgery. The patient said that thumb abduction was improved greatly after the operation, however, the hypoesthesia of the thumb and index finger persisted.
DISCUSSION
LFH is a rare condition in which normal forms of adipose and fibrous tissues diffusely infiltrate the peripheral nerve [13]. This condition occurs in patients at a relatively young age. Of the reported cases, approximately 71% of patients presented with LFH before the age of 30 and 33% of patients developed LFH immediately after birth or within the first year. Macrodactyly around the median nerve was present in 30% of LFH patients [2]. However, there was no association with family history [13]. Several studies report that pressure from the flexor retinaculum and transverse carpal ligament causes microtrauma to the median nerve, leading to LFH [4,9]. Reports of trauma before the onset of symptoms and the early age of onset support the speculation of posttraumatic and congenital etiologies for LFH [3,13]. Previous trauma to the affected area, such as laceration before the onset of symptoms or surgeries for other types of tumors was observed in 8% of the patients while another 14% of LFH patients had received surgery to the affected area for similar conditions. In our cases, the first case had a history of injection on her right wrist 7 years before the operation, and the second had surgery on her left wrist in childhood. However, it is very difficult to determine how injection or surgery is involved in the development of LFH.
The most common symptoms in patients with LFH are enlarging masses on the distal forearm, wrist, palm, or digits [13]. Tumors gradually increase in size and neuropathy from median nerve compression presents in varying degrees. The chief complaints of the patients in this report were numbness of the thumb, index, and middle fingers and weakness of thumb abduction. The complaint about the development of mass is subsequently reported.
Differential diagnosis should include other tumors on the median nerve such as ganglion cysts, lipomas, and traumatic neuromas. Neurofibromas and schwannomas, which may become malignant, could also present in a similar manner. Differentiation from malignant conditions, such as liposarcoma and malignant peripheral nerve sheath tumor, is also necessary. In LFH, fibrofatty tissue infiltrates the nerve fascicle, making it difficult to separate the tumors and the nerves, while schwannoma is encapsulated and can be easily isolated from the normal nerves. However, neurofibromatosis is difficult to distinguish visually from LFH with macrodactyly, as both are not encapsulated and exhibit mesenchymal overgrowth following a nerve distribution. However, the lack of neurocutaneous manifestations and family history allows the differentiation of LFH from neurofibromatosis. Moreover, the two can be further distinguished histologically, as neurofibromatosis elicits tumefaction of the nerve while LFH is associated with the proliferation of fibrofatty tissue, leading to infiltration between the nerve fibers [11,13].
Simple radiographs do not reveal any abnormalities in LFH other than the expansion of the soft tissues. In LFH with macrodactyly, phalangeal bony hypertrophy may be observed. MRI is a critical tool for the diagnosis of LFH. MRI findings that are characteristics of LFH include displacement of the flexor retinaculum and adjacent tendons due to hypertrophy of the median nerve viewed in the axial cut; the appearance of coaxial cables with low-intensity nerve bundles embedded within high-intensity adipose tissue along the median nerve as viewed in the T1-weighted images; and an hourglass appearance caused by fusiform swelling of the median nerve and compression by the transverse carpal ligament, as well as spaghetti-shaped nerve bundles surrounded by adipose tissues inside the median nerves as viewed in the coronal and sagittal cuts. Not all LFH have the same MRI findings. Toms et al. [14] reported three cases in which, unlike other LFH, nerve bundles were eccentrically located. In their cases, the tumors had large cross-sections of 2.2, 4.5, and 17 cm2, respectively. As in our second case of a large LFH, the nerve bundle may be eccentrically located in the MRI scan, not in a coaxial cable shape [14].
Biopsy provides a definitive diagnosis of LFH. Histological analysis shows a normal appearance of nerve fibers while fibroblasts and mature adipocytes separate the nerve fascicles and infiltrate the space between the epineurium and perineurium. Although routine nerve biopsy is very helpful for diagnosis, it is not recommended as functional sequelae may be a consequence. The biopsy can be performed on a non-lethal nerve branch or through limited epineurotomy [2]. The biopsy was performed only on parts of the epineurium in case 1.
Treatment options for median nerve LFH include a wide range of options, from close observation to complete nerve resection. In the absence of any neurologic symptoms, close observation has been advocated [10]. However, most authors advocate carpal tunnel release to decompress the median nerve in symptomatic patients [1,4]. Complete tumor excision can eliminate the risk of malignancy and the likelihood of a recurrence [6]. However, sensory and functional impairments and formation of painful neuroma may arise post-operatively, and this procedure is rarely recommended for the treatment of benign LFH. Silverman and Enzinger [12] reported persistent neurologic abnormality in one out of five patients who underwent incisional biopsy and four out of 12 patients who underwent excisional biopsy. Debulking the tumor has unpredictable outcomes with some authors reporting minimal functional sequelae and others documenting permanent neurologic deficit [5,7,15]. In our second case, the tumor tissue was excised with great care not to damage the nerve fascicle. However, at the final follow-up, the patient complained that hypoesthesia of the thumb, index finger, and the sensory distribution area of the median nerve remained. Thus, current treatment options have moved toward a more conservative approach. “Conservative approach” does not mean a non-surgical approach. It refers to the less invasive treatment such as carpal tunnel release and external neurolysis than more aggressive surgical treatment (e.g., complete tumor excision, debulking surgery, invasive intraneural dissection). Tahiri et al. [13] also mentioned the conservative approach as follows in a similar way to the authors' thoughts. Expectant management can be offered for patients with asymptomatic swelling without neurologic impairment and open carpal tunnel release is the mainstay of treatment for the patients with neurological abnormalities. Microsurgical dissection is also possible but generates disappointing results.
Patients with asymptomatic tumors can be observed without intervention. However, spontaneous regression of the tumor is uncommon and a gradual increase in size leads to compressive neuropathy. Carpal tunnel release may be performed as a preventive measure in asymptomatic patients with a large tumor. And external neurolysis, in addition to carpal tunnel release, can be a good remedy even for patients with large tumors [13]. The chief complaint in case 1 was the numbness of the hand. Therefore, the patient was very satisfied with carpal tunnel release and external neurolysis only.
CONCLUSION
These cases demonstrates the surgical treatment of LFH of the median nerve. Symptoms of compressive neuropathy of the median nerve do not require routine MRI. However, MRI examination is required for diagnosis when a mass is present in the wrist, similar to the current cases, and the MRI findings may allow a presurgical diagnosis of LFH. LFH infiltrates into the nerves of the normal adipose tissues and the fibrous tissues, making it difficult to separate the tumor from the nerves. Moreover, the biopsy of the tumor or its removal may aggravate neurological symptoms. Because of the rarity of the entity, the treatment of LFH is guided by the severity of the symptoms on a case-by-case basis. The conservative approach such as carpal tunnel release and external neurolysis should be recommended as treatment options.
Notes
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.
AUTHOR CONTRIBUTIONS
Data curation : SWS, IJP
Formal analysis : YK
Methodology : YK
Project administration : CJ
Writing - original draft : YTR
Writing - review & editing : IJP
Acknowledgements
We thank Chang Deok Weon, a medical photographer of Bucheon St. Mary’s hospital, the Catholic University of Korea for helping in preparing the photo.