Usefulness of Oblique Lateral Interbody Fusion at L5–S1 Level Compared to Transforaminal Lumbar Interbody Fusion
Article information
Abstract
Objective
The use of oblique lateral interbody fusion at the L5–S1 level (OLIF51) is increasing, but no study has directly compared OLIF51 and transforaminal lumbar interbody fusion (TLIF) at the L5–S1 level. We evaluated the usefulness of OLIF51 by comparing clinical and radiologic outcomes with those of TLIF at the same L5–S1 level.
Methods
We retrospectively reviewed and compared 74 patients who underwent OLIF51 (OLIF51 group) and 74 who underwent TLIF at the L5–S1 level (TLIF51 group). Clinical outcomes were assessed with the visual analogue scale for back pain and leg pain and the Oswestry Disability Index. Mean disc height (MDH), foraminal height (FH), disc angle (DA), fusion rate, and subsidence rate were measured for radiologic outcomes.
Results
The OLIF51 group used significantly higher, wider, and larger-angled cages than the TLIF51 group (p<0.001). The postoperative MDH and FH were significantly greater in the OLIF51 group than in the TLIF51 group (p<0.001). The postoperative DA was significantly larger in the OLIF51 group than in the TLIF51 group by more than 10º (p<0.001). The fusion rate was 81.1% and 87.8% at postoperative 6 months in the OLIF51 and TLIF51 groups, respectively, and the TLIF51 group showed a higher fusion rate (p<0.05). The subsidence rate was 16.2% and 25.3% in the OLIF51 and TLIF51 groups, respectively, and the OLIF51 group showed a lower subsidence rate (p<0.05).
Conclusion
OLIF51 was more effective for the indirect decompression of foraminal stenosis, providing strong mechanical support with a larger cage, and making a greater lordotic angle with a high-angle cage than with TLIF.
INTRODUCTION
A variety of spinal fusion techniques have been developed and used to treat degenerative diseases of the lumbar spine. Posterior lumbar interbody fusion (PLIF), transforaminal lumbar interbody fusion (TLIF), anterior lumbar interbody fusion (ALIF), direct lateral interbody fusion (DLIF), and oblique lateral interbody fusion (OLIF) are surgical techniques aiming at common objectives of improvement of low back pain, radiculopathy, and instability. Numerous studies have been published comparing the radiologic and clinical outcomes of these methods [9,12,13].
TLIF, which was first described by Harms and Rolinger [8], has been widely used for several decades. It is a posterior approach that uses a facetectomy corridor and has benefits of safety, good outcomes, and high fusion rate. Surgeons prefer this approach because they can reduce dural retraction and enable direct neural decompression [4,7,8]. However, characteristic complications include posterior spinal muscle injury and cerebrospinal fluid (CSF) leakage [10,16]. Additionally, TLIF does not provide an adequate sagittal angle at the level of L5–S1 since it is difficult to insert a sufficiently high profile and large angled cage through the small facetectomy space [18]. A wellknown limitation of TLIF is the inability to create the sagittal angle at the L5–S1 level, which is considered the largest contributor to the lumbar lordotic angle.
Davis et al. [5] developed a new fusion technique at the L5–S1 level, i.e., OLIF at L5–S1 (OLIF51), in 2014. OLIF51 approaches the disc space using a left retroperitoneal extrapsoas route in an oblique lateral direction with the patient in right lateral decubitus position [21]. In contrast to the retroperitoneal extrapsoas approach for OLIF at L2–5 (OLIF25), OLIF51 uses the corridor under the bifurcation of the great abdominal vessels [21]. This approach corridor for OLIF51 enables insertion of a cage with a greater height and angle compared with that in TLIF [3,21,22].
We planned a study to evaluate the usefulness of OLIF51 by comparing clinical and radiologic outcomes with those of TLIF at the same L5–S1 level based on our recent experience.
MATERIALS AND METHODS
This single-center study enrolled patients who underwent TLIF (TLIF51 group) or OLIF (OLIF51 group) at the L5–S1 level and were followed up for more than 6 months. Two senior surgeons performed TLIF (YBK) or OLIF (SWP). Single-level or multilevel lumbosacral fusion cases including the L5–S1 level for degenerative spine disorders were enrolled. Surgery for fracture, infection, tumor, and congenital anomalies were excluded. Age, bone mineral density (BMD), cages used at the L5–S1 level, and main pathologic conditions were compared between the two groups. In addition, estimated blood loss (EBL) and operative time were compared among patients who underwent single-level fusion at the L5–S1 level. This study was reviewed and approved by the Institutional Review Board (Chung-Ang University Hospital IRB No. 1904-002-16257).
Surgical technique
The TLIF51 group used unilateral open TLIF with a single polyetheretherketone (PEEK) cage (Capstone, Medtronic, Minneapolis, MN, USA), and autologous bone as a fusion material (Fig. 1A). We inserted an open pedicle screw and rod system (Zenius, Medyssey, Jecheon, Korea) using an interfascial approach at the surgical side and contralateral pedicle (Fig. 2A and B).

Comparison of cages used for each fusion technique, TLIF and OLIF. Perimeter cage was used in OLIF and Capstone cage was used in TLIF. Footprint size of Perimeter cage (right) is larger than the size of Capstone cage (left) (A). Cage angle and height of Perimeter cage (right) is larger than that of Capstone cage (left) (B). TLIF : transforaminal lumbar interbody fusion, OLIF : oblique lateral interbody fusion.

In TLIF51 groups, patients underwent mini-open surgery with a unilateral single cage and posterior pedicle screw fixation (A and B). In OLIF51 group, patients underwent minimally invasive surgery with a cage through a retroperitoneal approach at the left corridor via tubular retractor. And the percutaneous pedicle screw and rod system was used (C and D). TLIF51 : transforaminal lumbar interbody fusion at the L5–S1 level, OLIF51 : oblique lateral interbody fusion at the L5–S1 level.
The OLIF51 group used minimally invasive lumbar interbody fusion with a large round PEEK cage (Perimeter, Medtronic, Memphis, TN, USA) through a retroperitoneal approach at the left corridor using a tubular retractor (Fig. 1B). The cage was filled with demineralized bone matrix (DBM; Grafton; Medtronic) and a percutaneous pedicle screw and rod system (Longitude II, Medtronic) was used (Fig. 2C and D). In the OLIF51 group, patients with central canal stenosis underwent additional direct decompression using a minimally invasive unilateral approach with bilateral decompression technique, and other patients underwent indirect decompression only. However, both central and foraminal stenosis were decompressed directly in the TLIF51 group.
The OLIF51 approach uses an incision at two fingerbreadths anterior to the iliac crest, between the extension of the L5–S1 disc line and the vertical line from the L5–S1 disc center. Three abdominal muscle layers were dissected in a blunt manner, and then the retroperitoneal space was exposed.
The ureter is identified crossing medially over the left common iliac artery at the L5–S1 level, and a space is made between the ureter and the left common iliac artery. We could reach the disc space after retraction of the left common iliac vein to the left side. Three retractors (Hohmann, lateral, and cephalic retractors) were used to create a working space. After approaching the disc space, an incision was made on the left anterolateral side of the disc to create an annular window for the remaining half of the anterior longitudinal ligament (ALL) on the right side. The remaining contralateral half of the ALL was helpful for ligamentotactic effect and prevention of cage displacement during position change. Disc material was removed, and disc space was distracted with sequential insertion of trials. A cage filled with DBM was inserted to the center of the disc space. After changing the patient to a prone position, posterior fixation was performed with a percutaneous pedicle screw and rod system.
Clinical outcomes
We used the visual analog scale (VAS) for leg pain (VAS-L) and back pain (VAS-B) and the Oswestry Disability Index (ODI) to compare clinical outcomes between the two groups at preoperative and postoperative 6 months.
Radiographic measurements
Mean disc height (MDH), foraminal height (FH), and disc angle (DA) were measured in lateral simple radiographic images at preoperative and postoperative 6 months. MDH was defined as the mean value of the anterior height and posterior height between the L5 lower endplate and S1 upper endplate, and FH was defined as the height between the lower cortical line of the L5 pedicle and the upper line of the S1 pedicle. DA was measured in degrees between the lower endplate of the L5 body and the upper endplate of the S1 body. Fusion rate was evaluated using the fusion grading system of Bridwell [1]. According to this system, fu sion grades are defined as follows : grade 1, complete remodel ing with trabeculae across the disc space; grade 2, intact graft with no lucent lines observed between the graft and the adjacent endplates; grade 3, intact graft but a radiolucent line is present between the graft and an adjacent endplate; and grade 4, lu cency along an entire border of the graft or around a pedicle screw or subsidence of the graft. Grades 1 and 2 were considered solid fusion. Subsidence was defined as a decrease in height of more than 2 mm [14].
Two observations were made at an interval of at least 2 weeks by two neurosurgeons, and the mean values were used for the study.
Statistical analysis
Student’s t-test, the Mann-Whitney U test, and the chi-squared test were used to compare radiological and clinical outcomes of OLIF51 and TLIF51. Statistical significance was accepted for p-value <0.05. The intraclass correlation coefficient was checked to verify the intra-observer and inter-observer reliability of the radiologic measurements.
RESULTS
Demographic data
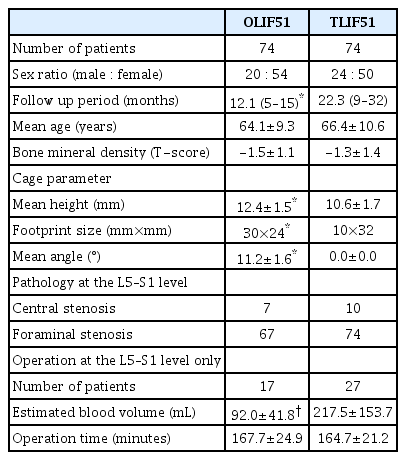
This study enrolled 74 patients in the OLIF51 group and 74 in the TLIF51 group (Table 1). Mean age and BMD were not significantly different between the groups. The ratio of central to foraminal stenosis was 7 : 67 in the OLIF51 group and 10 : 74 in the TLIF51 group, with no significant difference between the groups. Foraminal stenosis was the main pathology at the L5–S1 level in both groups. Five patients with central stenosis in the OLIF51 group underwent additional direct decompression. Mean height of the cage in the OLIF51 group was significantly greater than in the TLIF51 group (p<0.001). The footprint size of cages in the OLIF51 group was 30×24 mm, and the most-used cage angle was 12° (60 patients with 12° angled cage, 14 patients with 8° angled cage). The footprint size of cages in the TLIF51 group was 10×32 mm, and cage angle was 0°.
When we compared patients who underwent only single-level fusion at the L5–S1 level, EBL was less in the OLIF51 group than in the TLIF51 group (p<0.05), and operative time was not significantly different.
Clinical outcomes
VAS-L, VAS-B, and ODI improved significantly in both OLIF51 and TLIF51 groups. There was no significant difference between the groups (Table 2).
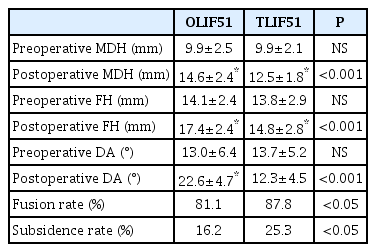
Radiological outcomes (Table 3)
There was no significant difference in the preoperative MDH and FH between OLIF 51 and TLIF 51 groups. The postoperative MDH was significantly greater than the preoperative value in each group (p<0.001). The postoperative MDH was significantly greater in the OLIF51 group than in the TLIF51 group (p<0.001). The postoperative FH was significantly greater than the preoperative value in each group (p<0.05). The postoperative FH was significantly greater in the OLIF51 group than in the TLIF51 group (p<0.05).
The preoperative DA showed no significant difference between the groups. The postoperative DA was significantly greater than the preoperative value in the OLIF51 group (p<0.001). However, there was no significant change in the TLIF51 group. Furthermore, the postoperative DA was significantly greater in the OLIF51 group than in the TLIF51 group by more than 10º (p<0.001).
The fusion rate was 81.1% at postoperative 6 months in the OLIF51 group compared to 87.8% in the TLIF group (p<0.05). Subsidence occurred less in the OLIF51 group than in the TLIF51 group, at 16.2% and 25.3%, respectively (p<0.05).
Complications
Minor injury to the common iliac vein occurred during the OLIF51 approach in the initial three cases, which was controlled with Gelfoam compression. One case of small peritoneal tearing was handled with simple sutures. There were no retrograde ejaculation, ureteral injury, or psoas symptoms. Postoperative ileus seemed to increase. Almost all patients who underwent OLIF51 showed ileus on the first postoperative day on simple abdominal X-ray. The postoperative ileus improved spontaneously during the next several days.
In the TLIF51 group, CSF leakage due to thecal sac injury and root injury was confirmed in three cases, and reoperation for epidural hematoma was performed in one case.
Inter-observer reliability and intra-observer reproducibility
In inter-observer agreement, the mean kappa value was 0.60 and the proportion of agreement was 81%. In intra-observer agreement, the mean kappa value was 0.73, with 86% agreement.
DISCUSSION
OLIF51 has various advantages by using a lateral retroperitoneal approach [17,19,21,22]. First, the abdominal structures move downward due to gravity in the lateral position, and the access corridor is increased as a result. Therefore, it is possible to approach the disc space with less peritoneal retraction compared to that in ALIF. Second, long level lumbar interbody fusions from L1 to S1 can be performed in a single position, because OLIF25 and OLIF51 use the same lateral position without hip bending. Third, unilateral blunt dissection and retraction of the hypogastric sympathetic plexus in the OLIF51 approach is the same as that used to prevent hypogastric sympathetic plexus injury in the anterior approach to the L5–S1 level, and can reduce the risk of postoperative retrograde ejaculation. Additionally, according to our study, the most frequent pathologic condition was foraminal stenosis at the L5–S1 level in both groups. As foraminal stenosis is a good indication for indirect decompression through an increase in disc height, OLIF51 seems to be quite useful for the L5–S1 level where foraminal stenosis is the main problem.
The OLIF51 group showed a statistically significant increase in MDH and FH compared to the TLIF51 group, and the postoperative DA was significantly greater in the OLIF51 group. These results are predictable because of the differences in surgical technique and cage features. OLIF51 provides easy access and sufficient space for insertion of a high profile and large angle cage in the L5–S1 disc space. On the other hand, it is very hard to increase disc height by inserting a large cage in TLIF due to obstacles such as the facet joints, dural sac, and nerve roots. The cage used for OLIF51 has a high profile (8–16 mm) and angle (6–12º), and a large footprint (30×24 mm), all of which are significantly greater than the cages for TLIF. However, the mean postoperative DA of 22.6±4.7° at L5–S1 level in OLIF51 was greater than the reported normal range for the L5–S1 DA of 14.13° [2]. This may result in an adverse effect, in which foraminal stenosis rather than indirect foraminal decompression is the outcome. The possibility of foraminal stenosis due to increased DA can be overcome by inserting a high-profile cage. The higher postoperative DA at the L5–S1 level may be helpful for prevention of iatrogenic flat back and may provide sagittal correction for degenerative flat back syndrome.
The fusion rate was higher in the TLIF51 group than in the OLIF51 group, which was related to the choice of fusion material. A prior study reported that autologous bone resulted in a higher fusion rate than DBM [6]. However, since OLIF51 has an advantage to insert a larger cage than TLIF, a better fusion rate could be expected through long-term follow-up studies. Subsidence was significantly less in the OLIF51 group than in the TLIF51 group. Le et al. [11] reported a lower rate of subsidence with use of a wider intervertebral cage, and our results showed similar trends. According to our data, use of a wider cage in OLIF51 than that in TLIF at L5–S1 resulted in increased mechanical stability and less cage subsidence.
There were no major complications with OLIF51, but postoperative ileus seemed to increase. The postoperative ileus improved spontaneously after several days. Early ambulation on the first postoperative day and parenteral nutrition for 2 days were recommended to prevent postoperative ileus in our hospital. Previous reports of psoas symptoms, a characteristic feature of the transpsoas approach, were not found in the OLIF51 group [17,20]. In the first three cases, minor injury to the iliac vein was considered related to the introduction of a new technique.
Since our retrospective study was a short-term investigation with a relatively small number of patients, long-term and larger-scale prospective studies are needed for more comprehensive evaluation. Each surgeon performed only TLIF or OLIF51 exclusively, which may result in bias. According to previous studies, percutaneous screw system and open pedicle screw system have not been reported to cause any significant difference to lumbosacral sagittal angle [15]. We preserved the contralateral half of the ALL. However, the outcomes of OLIF51 may have been quite different with total removal of the ALL or use of anterior plate and screw fixation. In addition, the absence of postoperative retrograde ejaculation may be related to the age and sex distribution in our study, which included predominantly elderly male or female patients. Since subsidence and fusion rates were evaluated in a relatively short period with postoperative 6-month radiographs, prospective long-term studies are needed for a more accurate evaluation.
CONCLUSION
Both OLIF51 and TLIF at the L5–S1 level showed good clinical and radiological outcomes. However, OLIF51 was more effective for indirect decompression of foraminal stenosis, providing strong mechanical support with a larger cage, and making a greater lordotic angle with a high-angle cage than with TLIF.
Notes
No potential conflict of interest relevant to this article was reported.
INFORMED CONSENT
Informed consent was obtained from all individual participants included in this study.
AUTHOR CONTRIBUTIONS
Conceptualization : HYM, SWP
Data curation : HYM
Formal analysis : HYM
Methodology : SWP, MJK
Project administration : SWP
Visualization : HYM
Writing - original draft : HYM
Writing - review & editing : HYM, SWP, MJK, YBK