A Comparison of Anterior Cervical Discectomy and Fusion versus Fusion Combined with Artificial Disc Replacement for Treating 3-Level Cervical Spondylotic Disease
Article information
Abstract
Objective
The purpose of this study is to evaluate the efficacy and safety of 3-level hybrid surgery (HS), which combines fusion and cervical disc replacement (CDR), compared to 3-level fusionin patient with cervical spondylosis involving 3 levels.
Methods
Patients in the anterior cervical discectomy and fusion (ACDF) group (n=30) underwent 3-level fusion and the HS group (n=19) underwent combined surgery with fusion and CDR. Clinical outcomes were evaluated using the visual analogue scale for the arm, the neck disability index (NDI), Odom criteria and postoperative complications. The cervical range of motion (ROM), fusion rate and adjacent segments degeneration were assessed with radiographs.
Results
Significant improvements in arm pain relief and functional outcome were observed in ACDF and HS group. The NDI in the HS group showed better improvement 6 months after surgery than that of the ACDF group. The ACDF group had a lower fusion rate, higher incidence of device related complications and radiological changes in adjacent segments compared with the HS group. The better recovery of cervical ROM was observed in HS group. However, that of the ACDF group was significantly decreased and did not recover.
Conclusion
The HS group was better than the ACDF group in terms of NDI, cervical ROM, fusion rate, incidence of postoperative complications and adjacent segment degeneration.
INTRODUCTION
Cervical spondylosis (CS) is a common pathological condition in elderly patients and is a frequent cause of disability and loss of productivity8,22). Surgical options to treat cervical spondylosis include anterior cervical discectomy and fusion or corpectomy (ACDF or ACC), posterior decompression (laminoplasty or laminectomy and fusion) and the combined anterior and posterior approach. However, in many cases, CS often involves multilevel lesions and surgical treatment can be challenging and complicated in multilevel CS. To date, the most effective and safest surgical treatment for patients with multilevel CS remains controversial. When the anterior approach is employed, multilevel ACDF or ACC are typically used and these techniques have already been proven to be effective and safe26). The anterior approach is very effective in resolving symptoms and improving nerve function. Most of all, many spine surgeons are familiar with this approach. In spite of these favorable factors, high pseudoarthrosis rate and device related complications are well-known problems and are often observed after multilevel ACDF2,20,28). Additionally, adjacent segment degeneration (ASD) has been described as a long term complication of ACDF because it alters the normal spinal biomechanics3,4,10). Some studies have reported that 2 level hybrid surgery (HS), consisting of cervical disc replacement (CDR) combined with ACDF, shows favorable clinical and radiological outcomes compared to 2 level fusion surgery24). However, there are only a few studies comparing 3-level ACDF and 3-level HS for the treatment of contiguous 3-level CS that spans more than 2 disc levels.
The purpose of this study was to compare the clinical and radiologic outcomes of patients with 3-level CS who were treated with CDR combined with ACDF (HS group) and 3-level ACDF (ACDF group).
MATERIALS AND METHODS
Patient populations and indications
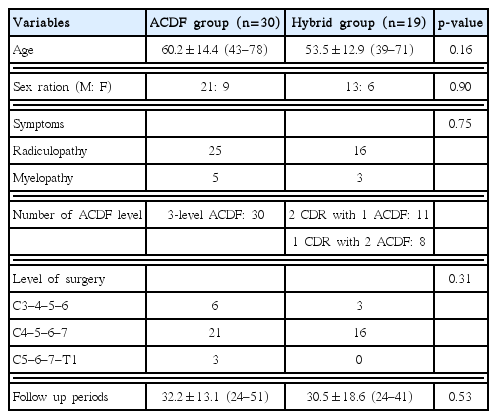
After institutional review board approval was obtained, a retrospective review of 49 patients who underwent surgical treatment for contiguous 3-level cervical spine lesions was performed. From January 2010 to January 2014, 49 patients (34/15 [males/females]) that underwent 3-level anterior cervical spine surgery were included in this study. The mean age was 57.8 years, ranging from 39 to 78 years. The demographic and clinical data for the 49 patients are summarized in Table 1. According to the surgical techniques, these patients were classified into 2 groups: ACDF group and HS group. HS was defined as a CDR combined with ACDF. Nineteen patients in the HS group were compared with 30 patients in the ACDF group. The ACDF group underwent fusion with a cervical plate system (Zephir plate; Medtronic, Memphis, TN, USA). In total disc replacement (TDR) group, 19 patients had 30 arthroplasties using Active-C disc® (B. Braun, Sheffield, UK) and Baguera C® (Spineart, Paris, France). All surgeries were performed by two surgeons in our institute.
The patient inclusion criteria in both groups were: 1) patients must have cervical radiculopathy and/or myelopathy; 2) cervical spondylosis include degenerative disc disease, degenerative ligamentous disease and/or osteophyte formation and must be confirmed by cervical radiography, computed tomography (CT) and magnetic resonance imaging (MRI); and 3) cervical spine pathologies were 3 consecutive levels between C3 and T1 which had not responded to conservative treatment (medication for at least 6 weeks). Cases with more than 3 levels were excluded because the number of cases was small. In the HS group, at least one-level must meet the criteria for CDR among the multilevel lesions. According to the degree of degeneration in the cervical spine, fusion or CDR was selected. The degree of degeneration was determined by using preoperative dynamic radiographs, CT or MRI scans. If there were no motion, the presence of instability and severe degeneration, such as facet hypertrophy, ligament flavum hypertrophy and/or osteophyte formation in target level, ACDF was performed. If the target level met the CDR criteria, CDR was performed. Exclusion criteria included those currently accepted for ACDF or CDR.
Clinical and radiological outcomes evaluations
The reviewed clinical outcomes were evaluated based on the visual analogue scale (VAS) of the arm, the neck disability index (NDI) and the Odom’s criteria15). Pain intensity was rated from 0 to 10. The NDI scores varied from 0 to 50. The results were recalculated and expressed on a scale ranging from 0% (no disability) to 100% (maximum disability). Clinical outcome evaluation was performed before surgery and the routine postoperative interval was 1, 6, 12, and 24 months.
Preoperative dynamic radiographs, CT scanning and MRI were performed for all the patients. Postoperative dynamic radiographs were evaluated at the interval of 1, 6, 12, and 24 months. The cervical ROM was calculated based on the difference in Cobb angles between full flexion and full extension on the lateral radiograph with PACS workstation (Marosis; Marotech, Suncheon, Korea) (Fig. 1). Lordosis was expressed as a negative value and kyphosis was expressed as a positive. We checked the ROM twice and obtained the mean to reduce the error. The radiological change in the adjacent level after surgery was also evaluated. The ASD during the follow up periods was determined as follows: 1) increased or newly developed narrowing of the disc space; 2) new osteophyte formation or enlargement; and 3) new or enlarged calcification of the anterior longitudinal ligament.

The cervical ROM is defined as the difference in the Cobb angle between the lateral ˛exion (C2–C7 Cobb, α) and extension (C2–C7 Cobb, β) view. ROM: range of motion.
Complications were retrospectively reviewed via the medical records of each patient. The complications for all patients were investigated including surgery related complications (soft tissue swelling, infections, hematoma, dysphagia and hoarseness), device/graft-related complications (graft dislodgement, hardware breakage, screw pull out, and graft subsidence) and pseudoarthrosis. Pseudoarthrosis was defined when the following conditions were still observed 3 months after surgery: 1) radiolucent line or gap observed between the graft and end plate; 2) motion at the treated level observed on dynamic lateral X-ray views; and 3) bony bridging not observed between the graft and the endplate.
Statistical analysis
The comparison of group characteristic, functional outcome, complication rate and radiological change of adjacent degeneration between the groups after surgery was performed using Chi-square tests. Radiological values were checked 2 times and the mean values were used for statistical analysis. Continuous variables including NDI and ROM were expressed as mean±standard deviation. Independent t-test was used in analysis of clinical and radiological results. All the statistical analysis was performed with SPSS software version 15 (SPSS Inc., Chicago, IL, USA). p values <0.05 were considered statistically significant.
RESULTS
Over 5 years, forty nine patients with 3 consecutive levels of CS were treated with 3-level ACDF or 3-levels HS at our institution. Among 19 patients in HS group, 2-level TDR and 1-level ACDF was performed in 11 patients and 8 patients underwent 1-level TDR and 2-level ACDF. The mean clinical and radiological follow-up period ranged was 42.3 months (range, 24–51 months). A diagnosis of cervical radiculopathy and/or myelopathy was established in all patients. The male-to-female ratio was 34: 15 and the mean patient age was 57.8 years (range, 39–78 years). The operation time was investigated in the two groups. The operation time in the ACDF and HS group was 129.4±25.9 and 116.5±29.8 minutes. No significant difference was observed between the two groups (p>0.05). Clinical and radiological results were summarized in Table 2.
Clinical outcomes
The mean VAS scores for arm pain in the ACDF group significantly decreased from 6.7±0.7 preoperatively to 3.1±0.6 in 1 month, 2.8±0.5 in 6 months, 2.4±0.8 in 12 months, and 1.7±0.5 in 24 months after surgery. The corresponding mean VAS scores for arm pain in the HS group also significantly decreased from 6.5±0.9 preoperatively to 2.9±0.6, 2.5±0.7, 2.2±0.9, and 1.6±0.6, respectively. There was no significant difference between the VAS scores for arm pain between both groups at the last follow up (p>0.05) (Fig. 2).

The VAS score for arm pain was significantly decreased in both groups. No difference was observed between the two groups at the last follow up. VAS: visual analogue scale, ACDF: anterior cervical discectomy and fusion, HS: hybrid surgery, POD: post operation day.
Regarding the NDI score, the mean NDI score in the ACDF group significantly improved from 53.6±9.3% upon admission to 33.9±4.3% after 1 month, 31.9±3.2% after 6 months, 29.6±4.9% after 12 months, and 28.0±3.8% at 24 months (p<0.05). For the HS group, the corresponding mean NDI score significantly improved from 52.7±7.3% to 32.7±3.7%, 25.1±2.9%, 23.6±2.6%, and 22.3±3.4%, respectively (p<0.05). The HS group demonstrated better NDI relief than the ACDF group 6 months after surgery (p>0.05) (Fig. 3).

The HS group shows better NDI relief than the ACDF group 6 months after surgery (p<0.05). NDI: neck disability index, ACDF: anterior cervical discectomy and fusion, HS: hybrid surgery, POD: post operation day.
According to the Odom’s criteria, for the ACDF group, clinical outcomes were excellent in 5 patients, good in 19, fair in 4 and poor in 2. The corresponding Odom criteria for the HS group were as follows: excellent in 6 patients, good in 12, fair in 1 and poor in 0. There were significant functional improvements in both groups and no significant differences were observed between both groups (p>0.05).
Radiologic evaluation
The radiological outcomes were analyzed with the ROM of C2–C7 and were compared between the ACDF and HS groups. Fig. 4 shows the changes in the ROM for the cervical spine over the follow up periods. The ROM for C2–C7 in the ACDF group was significantly decreased from 54.2°±10.2° preoperatively to 25.3°±4.3° in 1 month, 27.4°±3.6° in 6 months, 29.5°±2.3° in 12 months, and 32.4°±3.5° at the last follow up (p<0.05). In the HS group, the corresponding cervical ROM also significantly decreased from 53.5°±7.0° preoperatively to 29.6°±7.3°, 34.3°±6.1°, 36.1°±6.7°, and 41.1°±8.3° at the last follow up (p<0.05). Comparing the ROM between the two groups, significant differences in ROM for C2–C7 were observed 6 months after surgery (Fig. 4).

The cervical ROM of the HS group showed faster recovery than that of the ACDF group. ROM: range of motion, HS: hybrid surgery, ACDF: anterior cervical discectomy and fusion, POD: post operation day.
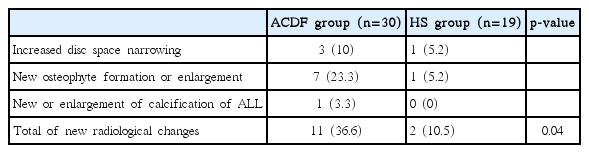
The incidence of ASD was analyzed according to the change in postoperative radiological imaging. Table 3 summarizes the radiological changes in adjacent segments in both groups at the last follow up after surgery. A total of 11 (36.6%) patients in the ACDF group experienced ASD during the follow up periods. In contrast, 2 (10.5%) patients with ASD were observed in the HS group. Radiographic ASD changes in the ACDF group were observed more frequently than in the HS group (p<0.05). Among thirteen ASD patients, none required second surgery due to symptomatic ASD.
The fusion rates in the ACDF group and the HS group were 70% (21 patients) and 94.7% (18 patients) at the last follow up. Significant difference was observed between both groups (p<0.05).
Complications
Postoperative dysphagia and device-related complications (plate migration, screw pull out, screw breakage and graft dislodgment) were more common in the ACDF group than the HS group. In the ACDF group, a total of 16 (53.3%) postoperative complications including dysphagia (6 cases, 20%), plate migration (5 cases, 16.6%), screw pull out (2 cases, 6.6%), screw breakage (1 case, 3.3%), and graft dislodgment (2 cases, 6.6%) occurred during the follow up periods. Among these patients, 3 patients required additional surgery for posterior screw fixation. In the HS group, postoperative complications including dysphagia (1 case, 5.2%) and plate migration (1 case, 5.2%) occurred during the follow up periods. No other complications were observed in the HS group. There was a significant difference in the incidence of device-related complications between the two groups (p<0.05).
DISCUSSION
In the present study, we evaluated the efficacy and safety of HS in 3-level CS compared to 3-level ACDF. Multilevel ACDF has some problems including the device related complications and high pseudoarthrosis rate even when an anterior plate is used20,28). More importantly, it is possible that the consecutive 3-level fusion may increase excessive motion and accentuate the degeneration of the remaining mobile segment compare to the single level fusion7,16).
CDR was devised to compensate for the disadvantages of ACDF9,17–19,21). Recently, ACDF is gradually being replaced by CDR as the surgical option for managing single level cervical disease. However, Auerbach et al.1) reported that only 43% of patients with cervical spine disease met the CDR criteria, or if the indications were expanded to include the treatment of ASD, the percentage of qualifiers rose to 47%.
In multilevel CS, there are limited studies about the efficacy of multilevel CDR and the biomechanics that affect the normal cervical spine motion. In order to overcome these problems related to multilevel ACDF or CDR, HS was devised. The basic concept of HS is that not all affected disc levels show the same degree of degeneration. Therefore, it is reasonable to tailor the most suitable procedure according to the status of the affected levels.
In the present study, comparison of the clinical and radiological results of ACDF versus the HS group with at least 2-year follow-up is presented. The operation time for the HS group was similar to that for the ACDF group. The clinical outcomes including VAS for arm pain, NDI and Odom’s criteria were significantly improved postoperatively compared to the preoperative status in all patient regardless to surgical methods. Consequently, both surgeries are effective for reducing radicular pain and restoring function. We speculate that this was the result of nerve root decompression rather than the specific technique – ACDF versus hybrid surgery – used. Particularly, NDI in the HS group showed better improvement than in the ACDF group, which was consistent with previous studies13,21). Regarding the radiological results, cervical ROM significantly decreased in both groups after surgery compared to the preoperative status. In the ACDF group, it was more significantly decreased than in the HS group. However, the ROM decrease in the HS group was limited to 6 months after surgery and gradually recovered and maintained during the follow up periods. Shin et al.24) reported that HS in 2-level CSD is superior to 2-level ACDF in terms of clinical and radiological outcomes. Kang et al.8) also reported that the combination of 2-level TDR with 1 level ACDF is comparable to 2-level ACCF in 3-level CSD. Our results are very similar to those of previous studies in that the 3-level HS group demonstrated better neck pain relief and radiological outcomes than the 3-level ACDF group. This may be associated with the preservation of the range of motion at the treated level and may be the basis for better clinical and radiological outcomes.
Regarding the complications, our study showed a higher incidence of device related complications including plate migration, screw pull out, screw breakage and graft dislodgement in the ACDF group than the HS group. This means that anterior plating alone lacks sufficient fixation power to immobilize the multilevel anterior cervical fixation. Some surgeons recommend combined anterior and posterior fixations for patients with multilevel CS to decrease these complications11,14,23,25,27). In our cases, additional posterior fixations were needed and 3 cases of posterior screw fixation were performed in the ACDF group during the follow up periods. However, additional posterior surgery runs the risk of surgical morbidity and additional expenses due to the long operative time and hospital stay. It may also lead to unnecessary postoperative neck pain for the patients. We suppose HS may reduce the compensatory movement or intradiscal pressure on adjacent segments. Additionally, HS may have a smaller hardware/graft-spine interface than 3-level fusion. Theoretically, it will help to decrease the stress to the graft and plate and reduce device related complications.
Postoperative radiologic changes of adjacent levels in both groups were also investigated. Our results showed that ASD changes were more common in the ACDF group than in the HS group, in close agreement with previous studies on the incidence of ASD after fusion5,6,12,18). Symptomatic ASD were not observed and no second revision surgery was needed during the follow up periods. We concluded that 2 years of follow up was not enough to observe the radiological changes in adjacent levels to convert to the symptomatic adjacent segment disease. A longer follow-up period is needed to evaluate the incidence of adjacent segment disease after multilevel ACDF.
This study has some limitations. First, this clinical study is a retrospective cases series. Second, in HS group, the surgical method and types of artificial discs are not homogeneous. Thirds, the number of patients was small and the follow up period was too short to draw a firm conclusion. A randomized controlled trial will be needed to evaluate these procedures in the future.
CONCLUSION
This result indicated that 3-level HS is an effective and safe procedure compared to 3-level ACDF in terms of NDI, fusion rate, restoration of ROM, reducing adjacent segment degeneration and complication rate. The selection of these surgical options must be considered first according to the degree of degeneration at each level and the location of the pathology.