Spondylolisthesis Accompanying Bilateral Pedicle Stress Fracture at Two Vertebrae
Article information
Abstract
There has been no report of bilateral pedicle stress fractures involving two vertebrae. The authors describe a unique case of spondylolisthesis accompanying a bilateral pedicle stress fracture involving two vertebrae. De novo development of spondylolisthesis at the L5-S1 vertebrae accompanying a bilateral pedicle stress fracture at L4 and L5 was observed in a 70-year-old woman. The patient's medical history was unremarkable and she did not have any predisposing factors except severe osteoporosis. Interbody fusion with bone cement augmented screw fixation was performed. Surgical treatment resulted in good pain management and improved functional recovery.
INTRODUCTION
Bilateral pedicle stress fractures in the spine are uncommon and are generally associated with previous spine surgery or stress-related activities3-5,7,9,12). Bilateral pedicle stress fractures as well as defects due to congenital aplasia are quite rare etiologies for spondylolisthesis. To the authors' knowledge, only one case of spondylolisthesis has been previously described in the literature4). Here, we report a rare case of spondylolisthesis accompanying a bilateral pedicle stress fracture in two levels not associated with major trauma, previous spine surgery, or stress-related activity. No such case has been previously reported in the literature.
CASE REPORT
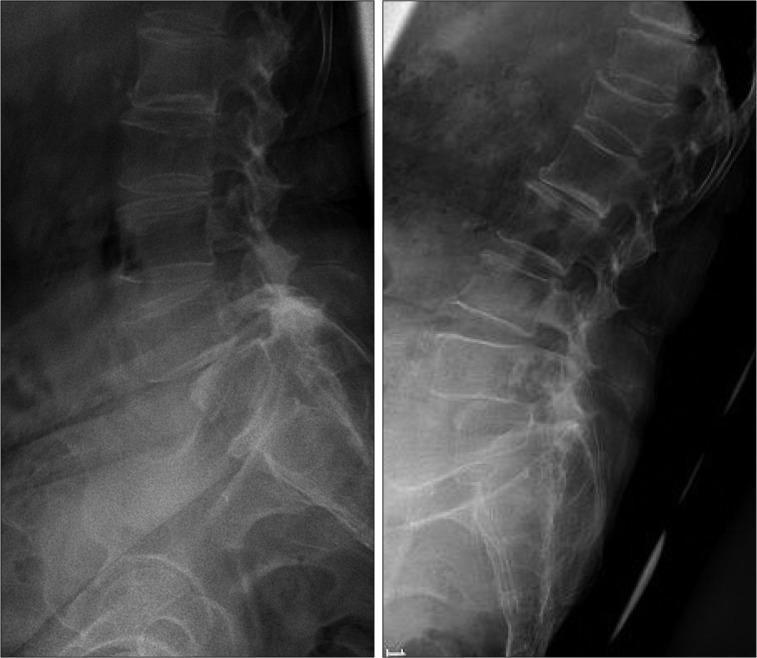
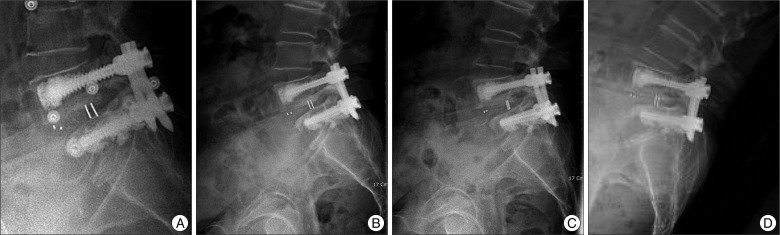
A 70-year-old woman with progressively worsening of lower back and leg pain for 2 years is presented. She had a history of mild back pain over the past several years but the leg pain had progressively increased without any traumatic episodes or spinal surgery. A review of the patient's past medical history showed that she had suffered from severe osteoporosis for 2 years and had taken bisphosphonate drug (FOSAMAX®) 70 mg once a week. Her condition worsened to the extent that she had not been able to walk for 3 weeks prior to admission. The leg pain radiated anteriorly to both thighs and laterally to the right calf. The back pain was worse with activites, and the patient experienced relief of pain by sitting or lying down. She had no paresthesia or muscle weakness of the legs, no bowel or bladder symptoms, and was able to straighten and raise her leg. Bone densitometry results indicated that her spine density as below average, and the mean T-score of the lumbar spine was -3.67. She had undergone menopause 20 years ago, and the patient had been healthy without prior medical concerns before admission except severe osteoporosis. Plain radiographs showed severe degenerative changes and Grade I spondylolisthesis at the L5-S1 vertebrae according to the Meyerding classification, but bilateral pedicle fractures were not clearly observed (Fig. 1). In the dynamic simple radiographs the instability at L4-L5 level was not evident. Computed tomographic (CT) scans and magnetic resonance imaging (MRI) confirmed the presence of a bilateral pedicle stress fracture of the L4 and L5 vertebrae, and an intact isthmus as well as a foraminal stensosis compressing the right L5 nerve root (Fig. 2). The patient underwent surgery using a posterior approach. After posterior segment removal and L5-S1 discectomy, interbody fusion using peek cages packed with autologous local bone chips were performed to provide anterior column support and bone cement-augmented screw fixation was done at L5-S1 level (Fig. 3A, B). The patient's postoperative course was uneventful. Her pain markedly decreased immediately after operation. At 12 months follow-up, she was pain free. Dynamic radiographs (flexion and extension) did not reveal any instability (Fig. 3C, D).
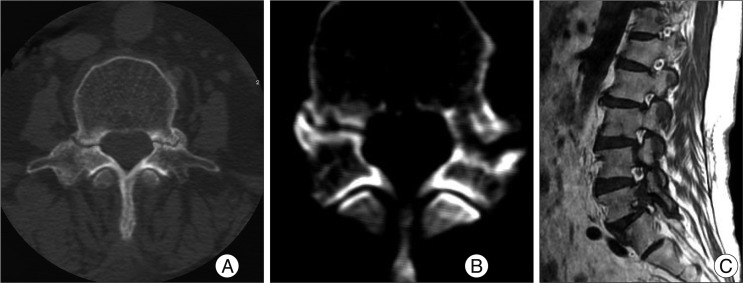
A and B : Axial computed tomographic scan reveal bilateral pedicle stress tractures at L4 (A) and L5 (B). C : T2 weighted magnetic resonance image shows bilateral pedicle stress fracture at L4 and L5 (arrows) and foraminal stenosis caused by spondylolisthesis.
DISCUSSION
During the past century, the etiology of spondylolisthesis has been extensively discussed in the literature. This can be categorized into several types : congenital, isthmic, degenerative, traumatic, and pathologic with alteration of the bone structure (e.g., osteoporosis, Paget's disease, osteolytic tumors, and iatrogenic spondylolisthesis)11). Repetitive mechanical stress fractures in the posterior elements are usually located in the pars interarticularis or, to a substantially lesser extent, in the pedicle. The pedicle has greater intrinsic strength and a shorter moment arm from the vertebral body, and can therefore resist greater cyclic shear forces 3). As a result, the pedicle is not common location of posterior elements fractures. Rather, they are more frequently observed in the isthmus, corresponding to the weakest zone.
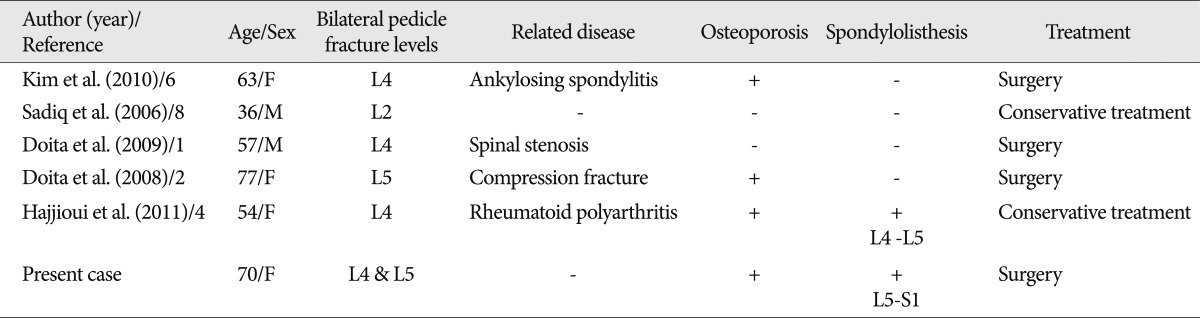
Bilateral pedicle stress fractures in the lumbar spine are quite rare and very few cases have been reported in the literature. Most of these fractures are associated with underlying causative factors, such as previous spine surgery or stress-related activities7,11). To the best of our knowledge, there has not been a previously reported case of spondylolisthesis accompanying a bilateral pedicle stress fracture involving two vertebrae. Currently, only five cases of bilateral pedicle stress fractures have been described occurring independent of the above-mentioned etiologies1,2,4,6,8). Among these, only one case was accompanied by spondylolisthesis (Table 1). Our patient did not have any predisposing risk factors for pedicle fractures except severe osteoporosis. Osteoporotic bone loss resulting in material and structural changes of the bone leads to an increased risk of stress fractures due to the weaken structure of the spinal bones. Tabrizi and Bouchard10) reported axial osteoporosis caused stress fractures of the pedicles and produce a spondylollisthesis in the 73-year old female patient. Stress fractures can develop after minor trauma or even in the absence of any specific trauma6). In our patient, the pedicle fracture appeared to be old given the sclerosis observed at the fracture margins along with pseudoarthosis. Thus, we speculate that continuous fatiguing stresses caused the microfractures on the osteoporotic pedicles. The three cases of bilateral stress pedicle fractures reported in the literature were treated with surgery, and two patients underwent conservative treatment. Our patient presented with spondylolisthesis with foraminal stenosis, and was treated with bone cement-augmented screw fixation and interbody fusion.
CONCLUSION
We report a unique case of spondylolisthesis accompanying a bilateral pedicle stress fracture in two vertebrae occurring in the absence of major trauma, previous spine surgery, or stress-related activity. Continuous fatiguing stresses to osteoporotic pedicles may have caused this rare occurrence of spondylolisthesis.