Angiographic Results of Wide-Necked Intracranial Aneurysms Treated with Coil Embolization : A Single Center Experience
Article information
Abstract
Objective
Endovascular treatment of wide-necked intracranial aneurysms is a challenge and the durability and the safety of these treated aneurysms remain unknown. The aim of this study was to evaluate the clinical and long-term angiographic results of wide-necked intracranial aneurysms treated with coil embolization.
Methods
Between January 2002 and December 2012, 53 wide-necked aneurysms treated with coil embolization were selected. Forty were female, and 13 were male. Twenty eight (52.8%) were ruptured aneurysms, and 25 (47.2%) were unruptured aneurysms. The patents' medical and radiological records were reviewed retrospectively.
Results
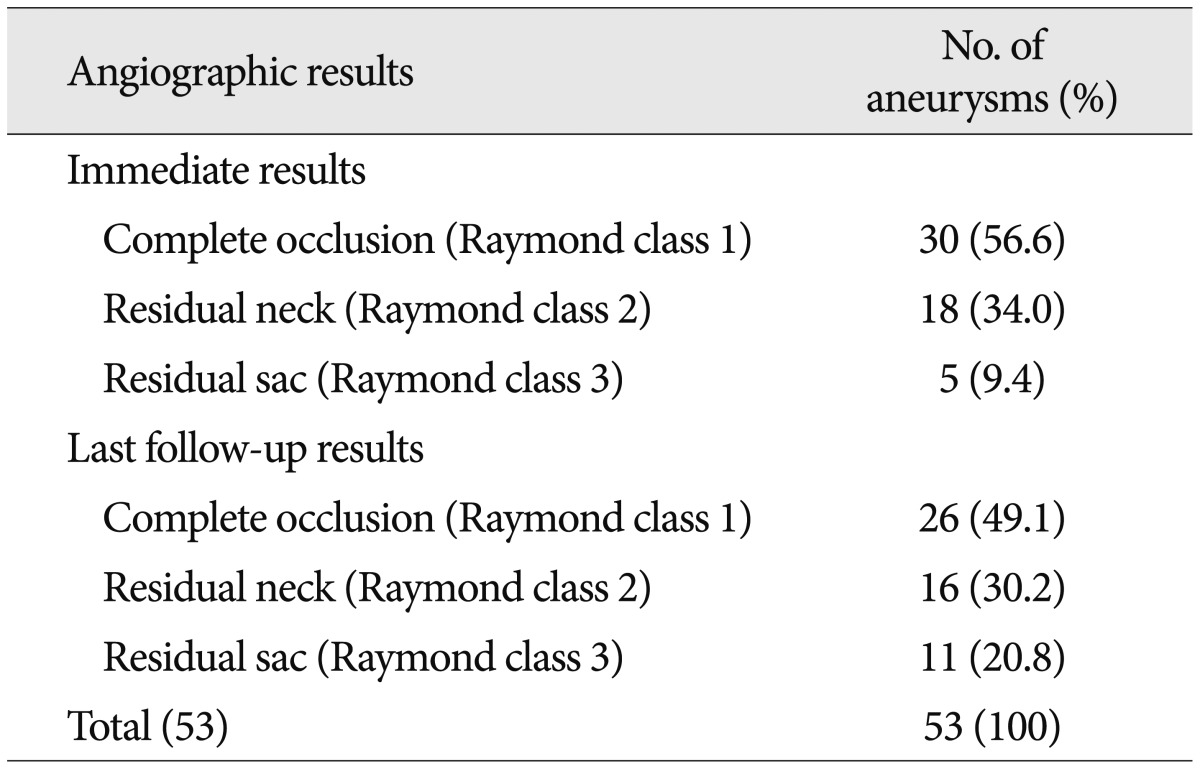
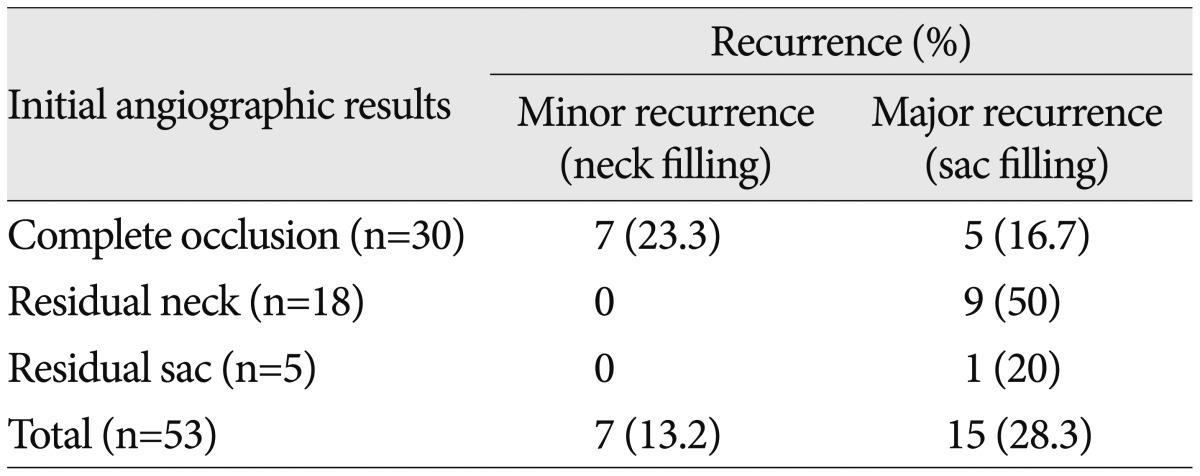
Of the 53 aneurysms, coiling alone was employed in 45 (84.9%) and stent-assisted coiling was done in 8 (15.1%). The initial angiographic results revealed Raymond class 1 (complete occlusion) in 30 (56.6%) cases, Raymond class 2 (residual neck) in 18 (34.0%) cases, and Raymond class 3 (residual sac) in 5 (9.4%) cases. The mean angiographic follow-up period was 37.9 months (12-120 months). At the last angiographies, Raymond class 1 was seen in 26 (49.1%) cases, Raymond class 2 in 16 (30.2%), and Raymond class 3 in 11 (20.8%). Angiographic recurrence occurred in 22 (41.5%) patients, with minor recurrence in 7 (13.2%) cases and major recurrence in 15 (28.3%). Retreatment was performed in 8 cases (15.1%). A suboptimal result on the initial angiography was a significant predictor of recurrence in this study (p=0.03).
Conclusion
The predictor of recurrence in wide-necked aneurysms is a suboptimal result on the initial angiography. Long-term angiographic follow-up is recommended in wide-necked aneurysms.
INTRODUCTION
Marked advances in endovascular techniques have expanded the scope of treatment for complex intracranial aneurysms resulting in improved angiographic and clinical outcomes. Despite these marked advances, complex aneurysms, including wide-necked aneurysms, large or giant aneurysms, and fusiform aneurysms, remain a challenge. It is frequently difficult to obtain complete aneurysm occlusion with wide-necked aneurysms (≥4 mm or a dome-to-neck ratio of <2) due to their unfavorable geometry10,11,27). The relative higher risk of the implanted coils encroaching into the parent vessel in wide-necked 2015aneurysms precludes complete aneurysm occlusion and leads to incomplete occlusion. Initial incomplete occlusion is prone to coil compaction and recanalization, raising the possibility of retreatment. To increase the occlusion rate, balloon-assisted coiling (BAC) and stent-assisted coiling (SAC) were introduced7,16). Although these led to improved outcomes, the reported complete occlusion rate of BAC and SAC was not satisfactory in follow-up angiographies. Complete occlusion was seen in 71-72% of intracranial aneurysms treated with BAC21,23) and 57-61% in those treated with SAC5,14,22). Although recent studies have reported favorable results in complex aneurysms, the long-term durability and the safety of wide-necked intracranial aneurysms treated with coiling are still questionable. The aims of this study were to present our experiences with coil embolization of wide-necked intracranial aneurysms and their long-term angiographic and clinical results.
MATERIALS AND METHODS
Patient characteristics
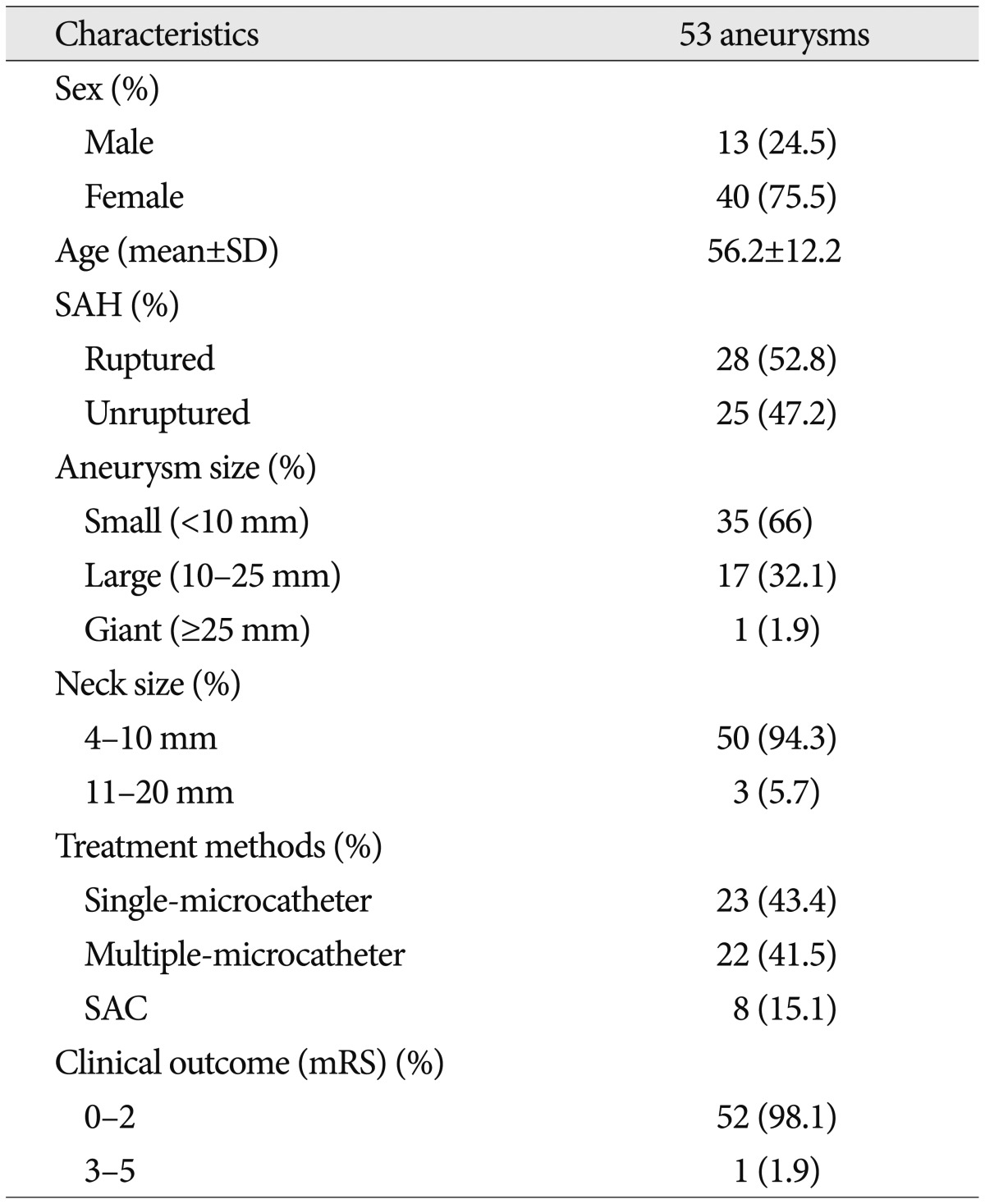
Between November 2002 and December 2010, endovascular treatments with coil embolization were performed on 320 aneurysms from 300 patients at our hospital. There were 121 aneurysms with wide necks measuring more than 4 mm and follow-up angiographies were performed in 86 aneurysms. Among them, only 53 wide-necked aneurysms had follow-up angiography of more than 12 months and these were selected for the study. Aneurysms were considered as wide-necked if the neck is ≥4 mm or the aneurysm has a dome-to-neck ratio of <2. Aneurysms with a narrow neck (less than 4 mm) were excluded. Of the 53 patients, 40 (75.5%) were female, and 13 were male. The mean age±SD was 56.2±12.2 years (range, 24-75). Twenty eight (52.8%) were ruptured aneurysms, and 25 (47.2%) were unruptured aneurysms. Reviewed characteristics included age, gender, aneurysm size, neck size, morphology, location, ruptured or unruptured nature, angiographic results and changes, procedure-related complications, and clinical outcome. The characteristics of the 53 aneurysms are described in Table 1.
Procedures
Before 2007, a monoplane angiographic system with 3-dimensional reformatted images was employed in our hospital. Since then, a biplane flat panel digital subtraction angiographic unit has been used for the procedure. The procedure was performed under general anesthesia in all patients.
If an aneurysm had square shape or lobulations, multiple-microcatheter system was mainly used. To select the aneurysm, 10 series of microcatheters including Excelsior SL-10 (Boston Scientific, Fremont, CA, USA) and Prowler-10 (Cordis, Miami, FL, USA) were used. When using the coil emolization with a two-microcatheter system, these two microcathers were used simultaneously to distinguish between the two mirocatheter's distal markers. Of the 53 aneurysms, the single-microcatheter system was used in 23 cases and multiple-microcatheter system was employed in 22 cases.
SAC was adopted it an aneurysm shape was not suitable for multiple catheter system in 8 cases. Neuroform stent (Boston Scientific, Fremont, CA, USA), Enterprise stent (Codman, Raynham, MA, USA), and Solitaire stent (Ev3, Irvine, CA, USA) were used in this study. If SAC was anticipated, the patient was premedicated with 75 mg of clopidogrel daily and 100 mg of acetylsalicylic acid (ASA) daily 5 days prior to the procedure. Patients with subarachnoid hemorrhage scheduled to undergo SAC were given 300 mg of clopidogrel and 300 mg of ASA after general anesthesia. After the procedure, all patients took 75 mg of clopidogrel daily and 100 mg of ASA daily for at least 3 months. All the patients received systemic heparinization during the procedure. Various types of coils including Guglielmi detachable coils (Boston Sicentific, Fremont, CA, USA), MicroPlex coils (Micro-Vention, Aliso Viejo, CA, USA), Trufill-DCS (Cordis, Bridgewater, NJ, USA), and Axium (eV3, Irvine, CA, USA) were used in this study.
Angiographic results and follow-up
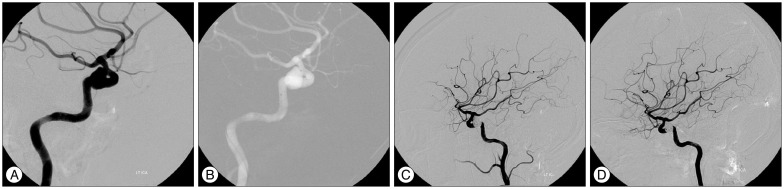
Angiography was scheduled at 6 months or 12 months, and the follow-up was scheduled at 1-2 year intervals after the treatment in all the patients if possible. The angiographic results were graded according to the Raymond Scale20). Raymond class I (complete occlusion) denotes complete obliteration of the aneurysm, including the neck. Raymond class 2 (residual neck) is defined as the presence of contrast filling in the neck. Raymond class 3 (residual sac) denotes the presence of any contrast filling of the sac. Angiographic recurrence was defined as any enlargement of contrast filling of the sac or contrast refilling of the neck in follow-up angiographies. To evaluate the stability and durability of the coil embolization, recurrences were subdivided into minor and major recurrence. A minor recurrence (Fig. 1) was defined as refilling of a neck that was previously completely occluded. A major recurrence (Fig. 2) was defined as refilling of a sac that was completely occluded initially or an increase in the filling of the sac. The mean follow-up period was 37.9 months (12-120 months).

Cerebral angiograms of a 44-year-old woman showing minor change. A : A left ICA angiogram shows a paraclinoid wide-necked aneurysm. B : An immediate angiogram after coil embolization shows near complete packing. C : An angiogram obtained 10 months later shows contrast filling in the aneurysm neck (minor change). D : A follow-up angiogram at 58 months shows neck filling, but no more severe compaction. ICA : internal carotid artery.

Cerebral angiograms of a 69-year-old woman showing major change. A : A left ICA angiogram shows a ruptured large aneurysm arising from the posterior communicating artery. B : An angiogram obtained immediately after coil embolization shows near complete packing. C : A follow-up angiogram obtained 12 months later shows coil compaction and contrast filling in the aneurysm sac (major change). D : An angiogram immediately after second coil embolization shows mild neck filling. ICA : internal carotid artery.
Clinical outcomes and procedure-related complications
The clinical outcome was evaluated using the modified Rankin Scale (mRS)26). The following procedure-related complications were documented: thromboembolic events, intraoperative rupture or extravasation, occlusion of branching artery, and coil migration. Periprocedural morbidity was divided into temporary neurological deficits, permanent neurological deficits, and death.
Statistical analysis
Statistical analysis was performed with the Statistical Package for the Social Sciences software version 18.0 (SPSS Inc., Chicago, IL, USA). A Cox's proportional Hazard model was used to examine variables that may be associated with recurrence; including age, sex, the presence of subarachnoid hemorrhage, sac size (small or large), treatment methods (single-microcatheter, multiple-microcatheter, and SAC), immediate angiographic results (complete or incomplete), and aneurysm locations (bifurcation or side wall). A p value of <0.05 was considered statistically significant.
RESULTS
Small aneurysms (<10 mm) were encountered in 66% (n=35), large aneurysms in 32.1% (n=17), and giant aneurysms in 1.9% (n=1) of patients. Of the 53 aneurysms, coiling alone was employed in 45 (84.9%) and SAC in 8 (15.1%). The mean aneurysm size was 9.6±4.3 mm (range, 4.5-28 mm), and the mean neck width was 5.5±2.2 mm (range, 4-17 mm). The most frequent location of the aneurysms was the paraclinoid segment (n=14, 26.4%) followed by the posterior communicating artery (n=10, 18.9%), the anterior communicating artery (n=9, 17.0%), middle cerebral artery bifurcation (n=5, 9.4%), cavernous segment (n=4, 7.5%), basilar top (n=4, 7.5%), and others (n=7, 13.3%). The Hunt and Hess grades in the 28 ruptured cases were; grade 1-2 in 17 (60.7%) cases, grade 3 in 7 (25%), and grade 4-5 in 4 (14.3%).
Initial angiographic outcomes
Of the 53 aneurysms, the initial angiographic results revealed Raymond class 1 (complete occlusion) in 30 (56.6%) cases, Raymond class 2 (residual neck) in 18 (34%) cases, and Raymond class 3 (residual sac) in 5 (9.4%) cases (Table 2). Of the 45 aneurysms treated with coiling alone, 23 (51.1%) were treated with a single-microcatheter system, and 22 (48.9%) were treated with a multiple-microcatheter system. Of the 23 aneurysms treated with the single-microcatheter system, 12 (52.2%) showed complete occlusion, 10 (43.5%) showed a residual neck, and 1 (4.3%) showed a residual sac. In the 22 aneurysms treated with the multiple-microcatheter system, Raymond class 1 was seen in 13 (59.1%), Raymond class 2 in 7 (31.8%), and Raymond class 3 in 2 (9.1%). In the 8 aneurysms treated with SAC, Raymond class 1 was seen in 5 (62.5%), Raymond class 2 in 1 (12.5%), and Raymond class 3 in 2 (25%).
Follow-up angiographic outcomes
Nineteen (35.8%) aneurysms had follow-up angiographies within 12-23 months, 11 (20.8%) within 24-35 months, and 23 (43.3%) had follow-up angiographies more than 36 months (36-120 months) after the embolization. The mean follow-up period was 37.9 months (12-120 months). In the last angiographies, Raymond class 1 was observed in 26 (49.1%) cases, Raymond class 2 in 16 (30.2%), and Raymond class 3 in 11 (20.8%) (Table 2). Thirty one aneurysms (58.5%) demonstrated stable results, showing complete occlusion, unchanged remnant, and progressive thrombosis. Progressive thrombosis occurred in 7.5% (4 of 53) of cases (Fig. 3).
Cerebral angiograms of a 62-year-old woman showing better change (progressive thrombosis). A and B : A left ICA angiogram reveals a superior hypophysial artery aneurysm identified incidentally. C : An angiogram immediately after coil embolization with double microcatheters reveals neck filling. D : A follow-up angiogram performed 6 months later reveals progressive thrombosis. ICA : internal carotid artery.
In the last follow-up angiographies of the 23 aneurysms treated with the single-microcatheter system, 11 (47.8%) showed Raymond class 1, 8 (34.8%) showed Raymond class 2, and 4 (17.4%) showed Raymond class 3. In the 22 aneurysms treated using the multiple-microcatheter system, Raymond class 1 was seen in 9 (40.9%), Raymond class 2 in 7 (31.8%), and Raymond class 3 in 6 (27.3%). In the 8 aneurysms treated with SAC, Raymond class 1 was seen in 6 (75%), Raymond class 2 in 1 (12.5%), and Raymond class 3 in 1 (12.5%).
Angiographic recurrence was identified in 22 (41.5%) aneurysms. Fifteen (28.3%) aneurysms showed major recurrence and 7 (13.2%) aneurysms minor recurrence (Table 3). In major recurrence group, 5 aneurysms (9.4%) that showed complete occlusion on the initial follow-up angiogram developed major recurrence and 9 aneurysms (17%) with residual neck on the initial follow-up angiogram had major recurrence.
There were 9 (17%) recurrences among aneurysms treated with the single-microcatheter system and 6 (11.3) of the aneurysms treated with multiple-microcatheter system. There was no recurrence in aneurysms treated with SAC. But, there was no statistically significant difference according to treatment methods (p=0.18). Only the suboptimal initial angiographic result reached statistical significance by Cox's proportional Hazard model analysis (p=0.03) (Table 4).
Recurrences were treated with coil embolization or surgical neck clipping if there was more than 30% increase in coil compaction. Retreatments were done in 15.1% (8/53) of cases. Of the 8 retreated aneurysms, 7 had coil embolization and 1 had neck clipping. Among the 7 retreated aneurysms, the last angiography showed complete occlusion in 4, residual neck in 2, and residual sac in 1.
Illustrative cases
Case 1
A 69-year-old woman presented with severe headache. Her left internal carotid artery angiogram showed a ruptured large aneurysm arising from the posterior communicating artery (Fig. 2A). The patient underwent coil embolization and the aneurysm was obliterated near completely (Fig. 2B). A follow-up angiogram performed 12 months later revealed coil compaction and contrast filling in the aneurysms sac, which means major change (Fig. 2C). Re-embolization was done and the control angiogram showed mild neck filling (Fig. 2D).
Case 2
A 39-year-old man presented with subarachnoid hemorrhage with a Hunt and Hess grade 3. An anterior communicating artery aneurysm was demonstrated on diagnostic angiogram (Fig 4A). Coil embolization was performed and the aneurysm was totally occluded (Fig. 4B). The aneurysm was seen minor change at the 24-month follow-up and no more changes at 50-month follow-up (Fig. 4C, D). However, major change was detected at 120 months follow-up angiogram (Fig. 4E, F), and the patient underwent surgical clipping (Fig. 4G).
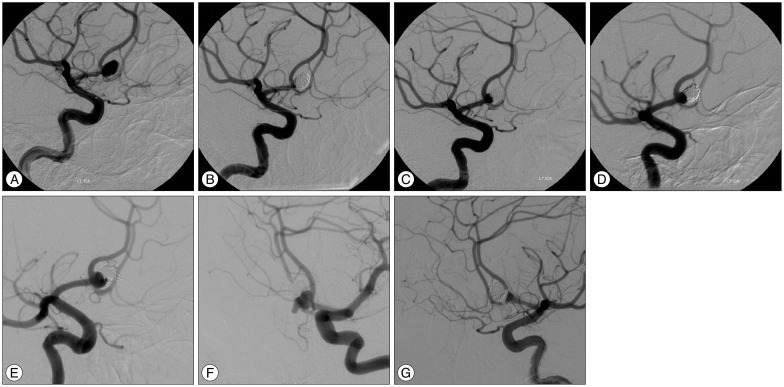
Cerebral angiograms of a 39-year-old man treated with coil embolization and surgical clipping. A : A left ICA angiogram shows a ruptured anterior communicating artery aneurysm. B : An immediate angiogram after coil embolization shows complete occlusion. C and D : Contrast filling in the aneurysm neck is seen at the angiogram performed 24 months later and no severe change at 50 month follow-up. E and F : A follow-up angiogram 120 months later reveals more compaction with a bleb. G : After surgical clipping, the angiogram shows totally obliterated aneurysm. ICA : internal carotid artery.
Clinical outcomes and complications
Fifty-two patients had favorable outcomes (mRS of 0-2) and 1 had fair outcome (mRS of 3). There were 6 (11.3%) procedure-related complications. Thromboembolism was documented in 2 (3.7%) cases. Among them, one was resolved with heparin, and the other resulted in cerebral infarction. Intraoperative aneurysm rupture occurred in 2 (3.7%) cases and all patients recovered without neurologic deficits. There was one case of ophthalmic artery occlusion occurring after the procedure, but the flow through the ophthalmic artery was restored at the follow-up angiography. Coil migration occurred in 1 case, which was removed by a snare and no neurologic deficit was seen after the procedure.
DISCUSSION
Predictors of the recurrence of wide-necked aneurysms
Recurrence in follow-up angiography is a major concern in endovascular treatment of wide-necked intracranial aneurysms. Several factors are regarded as predictors of aneurysm recurrence, including suboptimal initial angiographic result, aneurysm size, neck size, and ruptured lesions2,6,18,20,24,25). Raymond et al.20) reported the incidence and determining factors of angiographic recurrences after endovascular treatment of aneurysms. In their report, significant predictors of a recurrence were aneurysm size ≥10 mm, treatment during the acute phase of rupture, incomplete occlusions and duration of follow-up. In a large series of 916 aneurysms treated with coil embolizations, the overall recanalization rate was 20.9% and recanalization was related to the size of the dome and neck of the aneurysm17). According to Thornton et al.25), the final complete occlusion rate was 61% after more than 6 months of follow-up in a series of 141 aneurysms. Recurrence of the aneurysms occurred in 1.8% of cases completely occluded initially and in 28% of cases incompletely occluded. However, they did not categorize the aneurysms according to neck size and the mean neck size was 3.3 mm (1.5-8 mm) in their study. In our study, the aneurysm size, treatment methods, and anatomic site were not significantly related to angiographic recurrence. Only the suboptimal initial angiographic result was a significant predictor of recurrence in this study (p=0.03). The fact that all aneurysms selected in this study had wide necks (more than 4 mm) may account for these differences.
Adjunctive stent-assisted coiling
Incomplete occlusions including neck remnants or sac filling on the initial angiography has been considered a strong predictor of recurrence17). Advanced devices and techniques including BAC and SAC have been available since the mid-1990s to overcome technical limitations in treating wide-necked aneurysms7,16). Adjunctive stent deployment across the wide aneurysm neck allows for the packing of more coils and increased stability of the coil mass within the aneurismal sac. Hemodynamic modification between the aneurysm and the parent artery leads to profound thrombosis of the aneurysm. The rationale behind stent deployment in the treatment of wide-necked aneurysms is that the stent provides a scaffold for neointimal overgrowth of the implant and the coils in the neck region, thereby reducing any recurrence. However, antiplatelet therapy has to be administered in SAC, and this limits its application in cases of ruptured aneurysms. Neurointerventionists are also reluctant to use SAC due to the possibility of immediate or delayed in-stent stenosis. Several angiographic follow-up studies reported that SAC significantly reduced the recurrence rate compared with coiling alone (16.2% versus 34.4%, respectively)1,3,4,8,9,19). Piotin et al.19) reported angiographic results in 216 consecutive aneurysms treated with SAC. For small aneurysms, the recurrence rate of stented aneurysms was significantly lower than in nonstented aneurysms. Despite using stents, the reduction in the recurrence rates of larger aneurysms (reduced from 55.1% in the non-stent group to 32.6% in the stented group), was not satisfactory. Murayama et al.17) compared the angiographic recurrence of those treated in the first half of their series (1990-1995) with those in the second half (1996-2002) and found no significant improvements in large aneurysms (33.7% and 37.7%, respectively). These results show that SAC might be helpful in reducing the recurrence rate of small aneurysms with wide necks. However, recurrence rates remain disappointing, especially the recurrence rate of large aneurysms with wide necks. There was no major recurrence among the 8 aneurysms treated with SAC in the present study. Slight compaction was present in 1 patient who had a large aneurysm and initial result of Raymond 3. Two aneurysms showed progressive thrombosis. Even though no major recurrence developed in SAC group, there was no statistically significant difference according to treatment methods (p=0.18).
Multiple-microcatheter system
The technique of using multiple-catheter system is a useful method for coil embolization of wide-necked aneurysms10,12,13). If an adjunctive technique was needed, we prefer using the multiple-catheter system over the SAC. The advantages of using a multiple-catheter system instead of SAC are as follows : 1) no additional bulky devices are required; 2) it can be used to make a basket frame in the early stages of the procedure, without injuring the parent artery or branches; 3) long-term use of antiplatelet agents is not required because no permanent device remains inside the parent artery. In addition, the multiple-microcatheter system can be useful in cases of subarachnoid hemorrhage because antiplatelet agents do not have to be administered preoperatively. For these reasons, we mainly use the multiple-catheter system. Twenty two (41.5%) aneurysms were treated with the multiple microcatheter system in this study. Of these, 19 aneurysms were treated with double microcatheters, and 3 aneurysms were treated with 3 microcatheters. Among these, major recurrence was seen in 6 cases at the last follow-up. Extravasation developed during the procedure in one case treated with double-microcatheter system, but the patient was discharged without any neurological deficits.
Changes on angiography over time and follow-up periods
One of the major concerns of this study is the stability of coil embolization in wide-necked intracranial aneurysms. Determining angiographic changes in aneurysms on follow-up is important to ascertain whether retreatment is needed. We distinguished minor changes from major changes. Stable changes require no retreatment. Angiographic changes were observed in 41.3% of cases in this study, with minor changes seen in 13.2% and major changes in 28.3%. Major change was seen in 16.7% (5/30) of cases in the Raymond class 1 group and in 50% (9/18) of cases in the Raymond class 2 group. These results are similar to another report20). According to Raymond et al.20) reported, that the recurrence was found in 38.3% of cases in the compete occlusion group and 45.5% of cases in the residual neck group in long-term (>1 year) follow-up angiograms. Minor changes were seen in 23.3% (7/30) of cases in the complete occlusion group, which were regarded as stable. There was, however, no case of minor change in the Raymond 2 or 3 groups.
The length of the angiographic follow-up period is important in the detection of recurrence. In a series of 173 aneurysms, the recurrence rate was 19.6% at the 6-month follow-up. The l-year cumulative recurrence rate was 13.3% and long-term cumulative recurrent rate was 20.4% (12-54 months)15). In their series, 70.3% (19/27) of all recurrences were detected within 6 months. However, in another study, only 48% of recurrences were detected at the 6-month follow-up while 96.9% were detected at 36 months20). In the present study, major recurrence was detected in 13.3% (2/15) of patients within 6 months and in 73.3% (11/15) of patients within 36 months. The recurrence rate after 36 months was 0-3.1% in the previous two studies. The occurrence rate was 9.4% (5/53) and the detection rate of recurrence was 26.7% after 36 months in this study.
The mean time of the detection of recurrence was 35.6 months (follow-up periods, 20-120 months) in the group with minor changes and 20.5 months (follow-up periods, 15-113 months) in the group with major changes. Considering the development of recurrence even after 36 months, we suggest that follow-up angiographies should be performed for at least 36 months. Limitations of this study are : its retrospective design, lack of uniformity in the angiographic follow-up periods, and relatively few cases of SAC.
CONCLUSION
This angiographic follow-up study of 53 wide-necked aneurysms was able to detect major angiographic recurrence in 28.3% of cases. A suboptimal result on initial angiography was a significant predictor of recurrence (p=0.03). Long-term angiographic follow-up of more than 36 months is recommended in wide-necked intracranial aneurysms.