Outcome of Gamma Knife Thalamotomy in Patients with an Intractable Tremor
Article information
Abstract
Objective
Tremor is a common movement disorder that interferes with daily living. Since the medication for tremor has some limitations, surgical intervention is needed in many patients. In certain patients who cannot undergo aggressive surgical intervention, Gamma Knife thalamotomy (GKT) is a safe and effective alternative.
Methods
From June 2012 to August 2013, 7 patients with an intractable tremor underwent GKT. Four of these 7 patients had medical comorbidities, and 3 patients refused to undergo traditional surgery. Each patient was evaluated with the modified Fahn-Tolosa-Marin tremor rating scale (TRS) along with analysis of handwriting samples. All of the patients underwent GKT with a maximal dose of 130 Gy to the left ventralis intermedius (VIM) nucleus of the thalamus. Follow-up brain MRI was performed after 3 to 8 months of GKT, and evaluation with the TRS was also performed.
Results
Six patients showed objective improvement in the TRS score. Excluding one patient who demonstrated tremor progression, there was 28.9% improvement in the TRS score. However, five patients showed subjective improvement in their symptoms. On comparing the TRS scores between follow-up periods of more and less than 4 months, the follow-up TRS score at more than 4 months of GKT was significantly improved compared to that at less than 4 months of GKT. Follow-up MRI showed radiosurgical changes in 5 patients.
Conclusion
GKT with a maximal dose of 130 Gy to the VIM is a safe procedure that can replace other surgical procedures.
INTRODUCTION
Tremor is a common movement disorder that can interfere with daily living and impair the quality of life9). Medical treatment may help relieve the symptoms, but many patients either become unresponsive to the medication or suffer side effects from the medication. Ventralis intermedius (VIM) nucleus of the thalamus has been known to play an important role in the development of tremor, and various surgical modalities resulting in the destruction or modulation of the VIM nucleus have been used to control the symptoms. Radiofrequency thalamotomy (RFT) and deep brain stimulation (DBS) are representative of the surgical modalities which provide effective and sustained control of the tremor6,7).
However, in some patients surgical treatment may not be feasible because they have predisposing factors for high risk of procedure-related complications, although surgery is the best choice in terms of the therapeutic effect. Gamma Knife radiosurgery, the most commonly used method of stereotactic radiosurgery, has been used as an alternative to destructive surgery in patients who cannot undergo an invasive procedure. Prior reports have shown Gamma Knife thalamotomy (GKT) to be an effective treatment for tremor, with clinical improvement rates between 70% and 80%, comparable to those of stereotactic RFT4,10). The purpose of the present study was to investigate the clinical outcome of GKT in elderly patients with disabling tremor.
MATERIALS AND METHODS
We retrospectively reviewed the medical records of patients with tremor who were treated with GKT from June 2012 to August 2013. Seven patients underwent GKT (5 males and 2 females) and their mean age was 72.9 years (range, 70-75 years). Six patients were diagnosed with essential tremor, and one patient was diagnosed with Parkinson's disease in whom tremor was the predominant and disabling symptom. All of the patients had tremor duration of more than 5 years (range, 8-43 years) with tremors having a progressive or unresponsive clinical course despite sufficient medical treatment by the neurologists. GKT was considered in patients aged 70 years or older when RFT or DBS was not suitable due to medical comorbidities that prohibited invasive procedure (4 patients) or the patient refused to undergo traditional surgery (3 patients). Informed consent was obtained from all of the patients after explaining the procedure, benefits, risks, and alternatives (continued medical therapy, RFT, DBS, and no treatment) to radiosurgery. Although all of the patients had a bilateral tremor, they underwent left sided unilateral GKT.
Each patient underwent 1.5 tesla high-resolution MR imaging, with a stereotactic coordinate frame fixed to their head. MR imaging study included contrast-enhanced T1 images and T2 images taken at 2 mm intervals. MRI of the cranium including the thalamus and midbrain was performed to identify the anterior commissure (AC), the posterior commissure (PC), and the third ventricle. Stereotactic radiosurgical thalamotomy was performed using the Leksell Gamma Knife Perfexion model (Elekta instruments, Norcross, GA, USA). The intended target was the posterior and inferior part of the left VIM which was thought to be involved in the development of tremor. The target was set as follows to locate the isocenter of irradiation : 15-17 mm lateral to the AC-PC line; 7-8 mm anterior to the PC; and 3-4 mm superior to the AC-PC line. The laterality of the isocenter was carefully adjusted so as to keep it medial to the internal capsule. A maximum dose of 130 Gy was delivered with a single 4-mm isocenter and selective beam blocking was used to restrict the dose towards the internal capsule. The 20% isodose line of the 4-mm collimator was kept medial to the internal capsule and prescribed isodose volume was 94.7 mm3 in average (range, 93.1-96.2 mm3).
The modified Fahn-Tolosa-Marin tremor rating scale (TRS) scores3) were evaluated before and after GKT by neurologists who were not involved with the GKT procedure. Patient's handwriting, drinking from a glass of water, and tremors were evaluated separately (resting, postural, and action tremors). Writing short words such as the name and sentences like home address was evaluated, and drawing a straight line and a helical figure was also evaluated for both hands. Clinical follow-up with the modified TRS score was performed every 3 to 6 months. Follow-up brain MRI was performed at 3 to 8 months (median, 4 months) after GKT.
Preoperative and postoperative TRS scores were compared using the nonparametric Wilcoxon signed rank test (SPSS for Windows version 18.0 statistical software; SPSS Inc., Chicago, IL, USA).
RESULTS
The median follow-up period after GKT was 7.3 months (range, 3.3-12.1 months). All of the reported patients underwent pre- and post-operative testing. Baseline modified TRS score and follow-up TRS scores are shown in Table 1. Median baseline TRS score checked before GKT was 64 (range, 53-80), initial writing score for the right hand was 4 (range, 2-4), drinking score was 3 (range, 3-4), and tremor score for the right upper extremity was separately evaluated for resting, postural, and action tremors. The median resting, postural, and action tremor scores were 0, 2, and 3, respectively. The follow-up TRS score at less than 4 months after GKT was available in 6 patients. The median follow-up TRS score was 58 (range, 29-78), writing score was 3.5 (range, 1-4), drinking score was 3 (range, 1-4), and the median resting, postural, and action tremor scores in the right upper extremity were 0, 1.5, and 2.5, respectively. Until 4 months, 3 among these 6 patients showed improvement in the TRS score. On comparing between the pre-operative and post-operative TRS scores, there was no statistically significant difference in all of the values; total TRS score (p=0.674), writing score (p=0.317), tremor score (p=1.000), and drinking score (p=0.414).
Follow-up TRS score at 4 months and above after GKT was measured in five patients. The median TRS score was 53 (range, 23-78). The writing score was 3 (range, 2-4), drinking score was 3 (range, 0-4) and the median resting, postural, and action tremor scores in the right upper extremity were 0, 1, and 2, respectively. All five patients showed improvements in the TRS score, and of the remaining 2 patients who were not followed up after 4 months, one patient had already showed marked improvement within 4 months. Finally, 6 of the 7 patients showed objective improvement in the TRS score. There was 18.8% improvement in the follow-up TRS score in these 7 patients, and after excluding one patient who demonstrated progressive tremor and increase in the TRS score, there was 28.9% improvement in TRS scores in these 6 patients. Five patients agreed that there was improvement in subjective symptoms at the same time. Meanwhile, one patient reported no improvement in subjective symptoms despite objective improvement in the TRS score. Another patient did not show any objective and subjective improvement in the TRS score and symptoms, respectively after GKT until 4 months. Contrary to the TRS scores measured within 4 months after GKT, the follow-up TRS scores measured after 4 months of GKT showed statistically significant improvements. Improvement in the total TRS score (p=0.043) and tremor score (p=0.041) was found to be significant. But, the writing and drinking scores did not reach statistical significance (p=0.059, 0.189, respectively). The changes in TRS scores between before and after GKT measured within and after 4 months of GKT are shown in Table 1 and 2. There was no neurological deficit related to the treatment or other procedure-related complications.
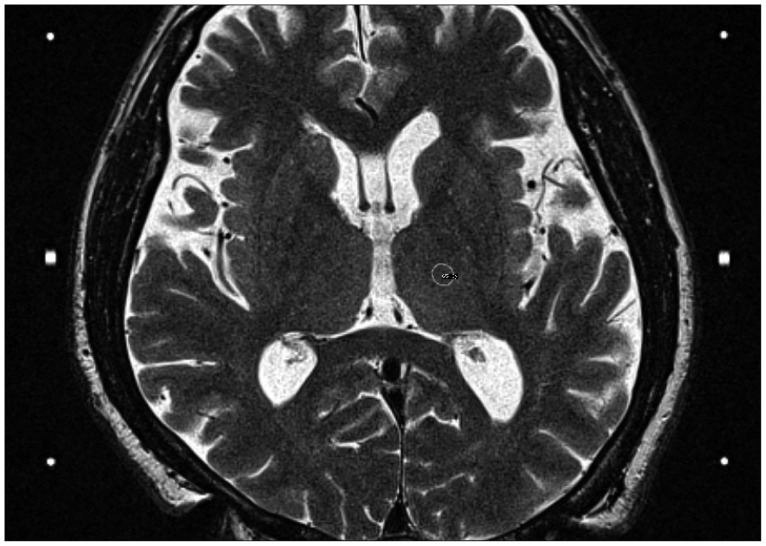
All of the patients underwent follow-up MRI after 3 to 8 months (median, 4 months) of GKT. Radiosurgical changes at the intended target site after GKT were seen in 5 patients. A well-circumscribed lesion with peripheral contrast enhancement around a low-signal region was detected. Mean diameter of the enhancing lesion was 4.77 mm (range, 3.8 to 5.63 mm). Four among these five patients showed symptom improvement at the time of MRI and the remaining one patient underwent MRI at 1 month after treatment and did not show any radiosurgical changes at that time and improvement in the symptoms. But, this patient showed delayed improvement at 8 months after GKT and follow-up MRI showed that the maximum diameter of the enhancing lesion was 5.63 mm. Therefore, MRI changes post-GKT were accompanied by symptom improvement in all five patients.
Case illustration
A 71-year-old man with a tremor in both hands visited our clinic. His hands had started shaking since 1990 and the action tremor was worse than the postural or resting tremor. The tremor aggravated gradually, and recently his voice too had started trembling especially when he was nervous. He received numerous medications at other hospitals, but the tremor could not be controlled effectively. His initial TRS score checked before GKT was 80. He refused to undergo invasive surgical treatment and preferred GKT. A maximal dose of 130 Gy was applied to the left VIM nucleus (Fig. 1). The drawing of a helical figure and the address written by the patient before GKT are shown in Fig. 2.
Radiosurgical target was calculated with Surgiplan (Elekta AB, Stockholm, Sweden). Maximal dose of 130 Gy was applied to 93.6 mm2 area by using a single 4-mm collimator.
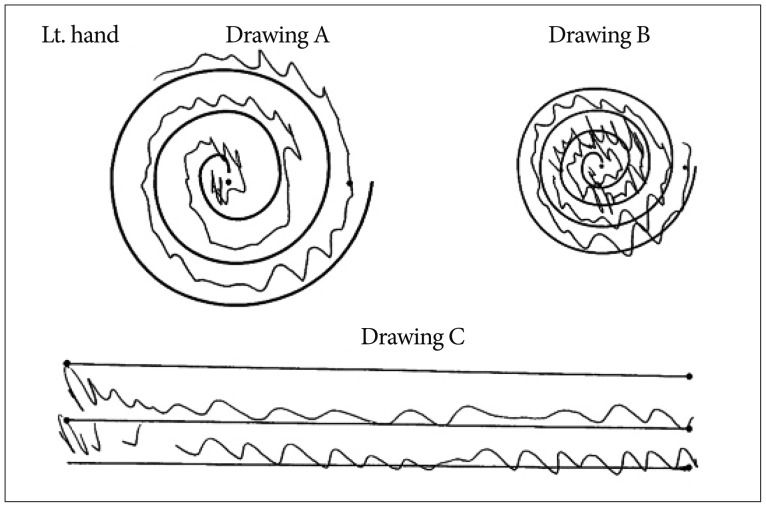
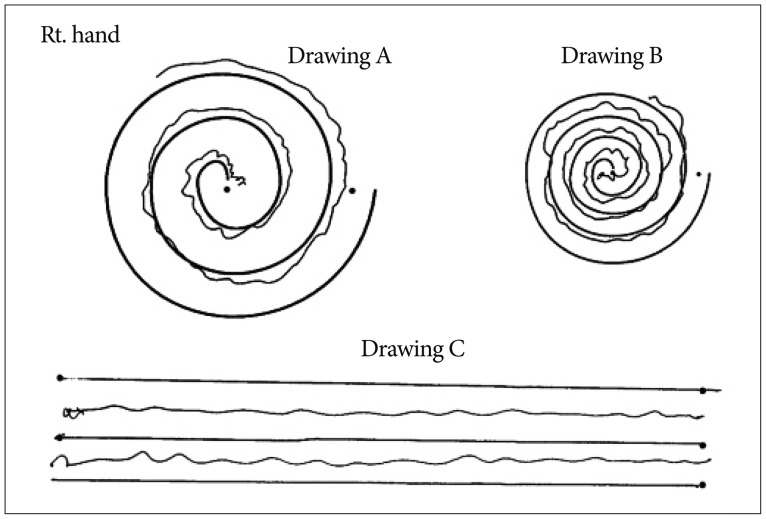
Drawing a helical figure using both hands and writing a short sentence with the right hand was done prior to the procedure.
At two months after GKT, the follow-up TRS score was 65 (81% of that at baseline). At 10 months after GKT, the TRS score was improved to 23 (29% of that at baseline). MRI scan with contrast enhancement was performed after 4 months of GKT. A peripheral enhancing rim-like lesion at the intended target site was noted on MRI (Fig. 3). His right hand tremor was nearly arrested and voice tremor was also reduced. The drawing of a helical figure and the address written by the patient at the last follow-up visit are shown in Fig. 4.

Follow-up MRI at 4 months after Gamma Knife thalamotomy. Peripheral enhancing rim-like lesion was seen at the intended target site.
DISCUSSION
Various surgical techniques were introduced over decades for a medically refractory, disabling tremor. DBS has been commonly used for the treatment of tremor since its introduction in 1980s due to advantages over other surgical treatments such as reversibility, individual modifiability, and non-destructive nature in terms of neuromodulation. However, in certain patients (including the elderly, those taking anticoagulants or with coagulopathy, those with medical comorbidities, and who refuse to undergo invasive surgical treatment), invasive procedures such as RFT and DBS are not a feasible option.
In this study, GKT proved to be effective in improving medically refractory tremor in patients and very safe in predominantly elderly patients. In our case series, the TRS score improved in 6 out of the 7 patients. Young et al.17), reported long-term results of GKT for the treatment of essential tremor. At 1 year post GKT, results in 51 patients were evaluated, and in this series 78% of patients were tremor free, 18% of patients were nearly tremor free, and in 8% of patients, the tremor had not improved. At 4 years post GKT, 71% of patients were tremor free, 18% of patients were nearly tremor free, and treatment had failed in 6% of patients.
Many centers attempted to use various doses for GKT. A rather high dose up to 180 Gy was used in earlier cases12). The use of a higher dose seemed to be associated with a relatively early clinical efficacy but treatment-related complications such as hemiparesis or dysarthria were frequently noted with the use of a high radiation dosage, especially when the dose was more than 150 Gy, and after considering the efficacy and the complications, the optimal dose for GKT has recently been reported as 130 Gy11). Although the size of the cohort was small and the follow-up period was short, the finding that there were no procedure-related complications in our study confirms the safety of the radiation dose of 130 Gy to the VIM.
In our study, the number of cases included was small (n=7) and the follow-up period (median, 7.3 months) was also short in order to evaluate the long-term outcome and the occurrence of complete arrest of the tremor. This must be the limitation of this study. But on com-paring between the follow-up TRS scores before and after 4 months of GKT, we observed that the TRS score was improved during the follow-up period after GKT. Also, the follow-up TRS score at more than 4 months after GKT reach-ed statistical significance, while the follow-up TRS score within 4 months of GKT failed to reach statistical significance. The follow-up TRS scores within 4 months and at more than 4 months of GKT were compared, and the results are shown in Table 2. Although we performed a rather short-term follow-up and included a small cohort, we could achieve an improvement in the tremor in 85.7% of the patients without any significant complications. Unlike the immediate outcome that can be observed after DBS or RFT, the minimal interval from GKT to achieving an effective outcome seems to be more than 4 months.
GKT for suppression of the action tremor has not been directly compared with DBS. Benabid et al.2), implanted thalamic DBS units in 20 patients with a tremor, and at the 3-month follow-up they found that complete or near complete relief of tremor had been achieved in 75% of patients, and this outcome was apparently better than that of GKT including that in the present study. Other groups have documented improved outcomes with DBS for essential tremor by performing an at least 2-year follow-up5,9,16). Complications after the DBS procedure include lead breakage, wound infection, electrode migration, and intracranial hemorrhage1,18). The complication rate after the DBS procedure reached almost 23.5% in some series18). Furthermore, side effects of stimulation include dysarthria, paresthesia, dystonia, balance disturbance, ataxia, and limb weakness8,13). Finally, the overall complication rate was more than 30%. Stereotactic RFT for essential tremor has a reported success rate of 73-93%, which again is comparable to that of GKT4,6,15). Compared with DBS, however, open thalamotomy may be associated with a poorer functional outcome and more adverse effects14). Meanwhile, no procedure-related complications and no neurological deficit occurred after GKT in the present study. The most critical factor related to complications after GKT is the prescribed dose, and a report of complications in a previous literature demonstrates a dose-dependent risk of GKT. Therefore, it can be suggested that GKT with prescribed maximal dose of 130 Gy is safer than the other surgical procedures although its therapeutic efficacy may not be similar to that of RFT or DBS.
CONCLUSION
GKT with maximal dose of 130 Gy to the target site of VIM is a very safe procedure for patients who cannot tolerate invasive surgical procedures. Although the short-term outcome of GKT may not be similar to that of DBS or RFT, GKT can be considered to be a superior modality in terms of safety.