Anatomic Feasibility of Posterior Cervical Pedicle Screw Placement in Children: Computerized Tomographic Analysis of Children Under 10 Years Old
Article information
Abstract
Objective
To evaluate the anatomical feasibility of 3.5 mm screw into the cervical spine in the pediatric population and to establish useful guidelines for their placement.
Methods
A total of 37 cervical spine computerized tomography scans (24 boys and 13 girls) were included in this study. All patients were younger than 10 years of age at the time of evaluation for the period of 2007-2011.
Results
For the C1 screw placement, entry point height (EPH) was the most restrictive factor (47.3% patients were larger than 3.5 mm). All C2 lamina had a height larger than 3.5 mm and 68.8% (51/74) of C2 lamina had a width thicker than 3.5 mm. For C2 pedicle width, 55.4% (41/74) of cases were larger than 3.5 mm, while 58.1% (43/74) of pedicle heights were larger than 3.5 mm. For pedicle width of subaxial spine, 75.7% (C3), 73% (C4), 82.4% (C5), 89.2% (C6), and 98.1% (C7, 1/54) were greater than 3.5 mm. Mean lamina width of subaxial cervical spine was 3.1 (C3), 2.7 (C4), 2.9 (C5), 3.8 (C6), and 4.0 mm (C7), respectively. Only 34.6% (127/370) of subaxial (C3-7) lamina thickness were greater than 3.5 mm. Mean length of lateral mass for the lateral mass screw placement was 9.28 (C3), 9.08 (C4), 8.81 (C5), 8.98 (C6), and 10.38 mm (C7).
Conclusion
C1 lateral mass fixation could be limited by the morphometrics of lateral mass height. C2 trans-lamina approach is preferable to C2 pedicle screw fixation. In subaxial spines, pedicle screw placement was preferable to trans-lamina screw placement, except at C7.
INTRODUCTION
Numerous posterior cervical fixation techniques have been developed to manage cervical spine instability and correct deformities. The introduction of segmental fixation using screw-rod system represents a significant advance in posterior cervical spine surgery. There have been lots of anatomical and biomechanical studies of cervical instrumentation in the adult population. In previous studies, the vast majority of adult cervical spine specimens were found to be suitable for lateral mass screw, pedicle screw and lamina screw especially in C2 and C7. However, these techniques have some limitations in pediatric patients due to their small and underdeveloped cervical spines. Because the screw fixation technique involves insertion of 3.5 mm diameter screws, there is concern about whether insertion of these screws is possible in children. If bony anatomy is not suitable for the screw placement, the surrounding critical neurovascular structures such as spinal cord, vertebral artery, venous plexus and cervical nerve root may be injured with errant screw placement. So far, only scarce data is available in the literature regarding posterior cervical fixation in the pediatric population.
This analysis of the morphometrics of the cervical spine was undertaken to assess the anatomical feasibility for the posterior cervical screw placement in the pediatric population and to establish useful guidelines for their placement.
MATERIALS AND METHODS
Retrospective data was evaluated from a total of 37 cervical spine computerized tomography (CT) scans (24 males and 13 females) included in this study. All patients were younger than 10 years of age at the time of admission (outpatient department or emergency care center) and the majority of patients suffered from minor cervical injuries or minor head injuries during a 5-years period (from February, 2007 to October, 2011). Patients with CT scan evidence of bony or ligament injury, deformity, intra-osseous pathology, or congenital anomalies were excluded. The average age of the whole patient sample was 57.1±35.9 months. To assess size and growth patterns of individual patients, the weight for age percentile growth chart for Korean pediatrics population was used. Pediatric patients were classified into a low-weight group, normal-weight group and over-weight group (cutoff value between three groups were 10 and 90 percentile). Not all patients had measured their body weight on the day of cervical CT evaluation, so only 27 cases were confirmed with an electrical medical chart review. Five patients were included in the low-weight group and 20 patients were included in the normal-weight group. Two patients were classified as over-weight group.
All patients had undergone standardized bone-window CT scanning from C1 to C7 cervical vertebra in a supine neutral position. Linear (in millimeters) and angular measurements were bilaterally made using m-view 5.4 software (Marosis Technologies, Inc., Seoul, Korea). Consequently, the dimensions and angulations of 518 cervical segments were obtained. All CT scans were performed on a 64-slice CT scanner with 2-mm axial image thickness (Siemens Medical Solutions, Erlangen, Germany). Sagittal and coronal reconstructions were obtained using 1.25-mm thickness slices. CT films were scanned at a resolution of 512×512 pixels. The thickness or length of the structure was measured with the inter-outer cortical space. Separate sections of axial or parasagittal images were used to determine the most reliable parameters in the whole cervical spine segments.
C1 (atlas) morphometric analysis
The method recommended by Chamoun et al.4) was used to measure the C1 structure.Fig. 1 shows representative dimensions in detail.

Axial (A and C) and sagittal (B and D) computed tomographic images show the morphometric anatomy for measuring C1 cervical spine. a : medio-lateral angle, b : lateral mass width, c : lateral mass height (anterior), d : lateral mass height (posterior), e : entry point height, f : supero-inferior angle, g : maximal screw length, h : C1 posterior arch height.
1) Entry point height (EPH) : between the lower margin of the C1 posterior arch and the lower margin of the posterior C1 lateral mass in the sagittal plane
2) Lateral mass width (LMW) : between the medial margin of the transverse foramen and the lateral margin of the cervical cord space in the axial plane
3) Maximal screw length (MSL) : maximal length for assuring bicortical purchase from the presumed entry point to the anterior margin of the C1 anterior arch in the axial plane
4) Lateral mass height-anterior (LMH-a) : anterior height of the lateral mass in the sagittal plane
5) Lateral mass height-posterior (LMH-p) : posterior height of the lateral mass in the sagittal plane
6) Medio-lateral angle (MLA) : maximal angular degrees to avoid the transverse foramen and lateral margin of the cervical cord space from the presumed staring point in the axial plane
7) Supero-inferior angle (SIA) : maximal angular degrees to avoid the occiput-C1 facet joint and C1-2 facet joint from the presumed starting point in the sagittal plane
All C1 dimensions measurements were conducted as the following regular patterns. The midpoint of the lateral mass was selected with parasagittal images using the multiple scout image viewer skill (simultaneously shows corresponding axial, sagittal and coronal images). The LMH-a, LMH-p, SIA, and EPH values were measured.
Second, previous images were used as scout images to determine the entry point in axial sections. The LMW, MLA, and MSL were then measured.
C2 (axis) morphometric analysis
Fig. 2 shows representative dimensions in detail.
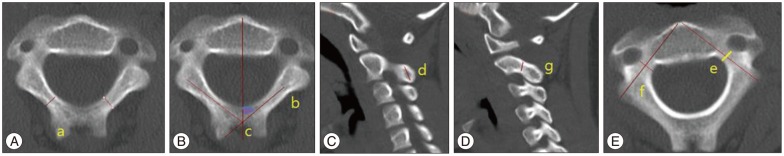
Axial (A, B, and E) and sagittal (C and D) computed tomographic images show the morphometric anatomy for measuring C2 cervical spine. a : lamina width, b : lamina length, c : spino-lamina angle, d : lamina height, e : pedicle width, f : pedicle length, g : pedicle height.
1) C2 lamina width (C2-LW) : transverse diameter of the lamina obtained at its narrowest part
2) C2 lamina height (C2-LH) : longest diameter in the sagittal plane
3) C2 lamina length (C2-LL) : distance from the contra-lateral spino-lamina junction to the lamina-lateral mass junction.
4) C2 pedicle width (C2-PW) : transverse diameter of the pedicle obtained at its narrowest point through the middle of the pedicle
5) C2 pedicle height (C2-PH) : between the upper and lower endplates in a para-sagittal reformatted image through the middle of the cervical pedicle
6) C2 pedicle axial length (C2-PAL) : from the anterior border of the vertebral body along the middle of the pedicle along its long axis to the posterior border of the lateral mass.
7) C2 spino-lamina angle (C2-SLA) : angle between the C2 spine process and a line parallel to the longitudinal axis of the lamina
Subaxial morphometric analysis
Fig. 3 shows representative dimensions in detail.
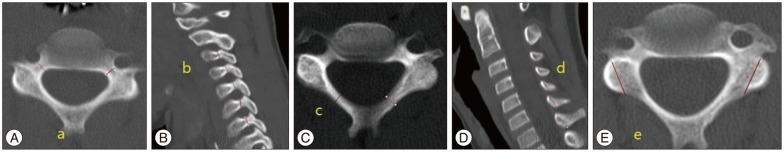
Axial (A, C, and E) and sagittal (B and D) computed tomographic images show the morphometric anatomy for measuring the subaxial spine. a : pedicle width, b : pedicle height, c : lamina width, d : lamina height, e : leteral mass length.
C3 : Third cervical vertebra, C4 : Fourth cervical vertebra, C5 : Fifth cervical vertebra, C6 : Sixth cervical vertebra, C7 : Seventh cervical vertebra
1) Pedicle width (C3-7 PW) : transverse diameter of the pedicle obtained at its narrowest point through the middle
2) Pedicle height (C3-7 PH) : between the upper and lower endplates in a para-sagittal reformatted image through the middle of the cervical pedicle.
3) Lamina width (C3-7 LW) : transverse diameter of the lamina obtained at its narrowest point
4) Lamina height (C3-7 LH) : LH was measured in the parasagittal plane
5) Lateral mass length (C3-7 LML) : from the midpoint of the lateral mass to the posterior lip of the foramen transversarium with 30° in lateral direction of the axial plane
Statistical analysis
Statistical analysis was performed using the SAS (Version 9.2) software program. Unpaired Student's t-test and paired t-test were used to analyze sex, laterality (left or right) and weight-related differences among specimens. A Pearson's correlation coefficient test was used to investigate the relationship between morphometric measurements of whole cervical spine and age. Statistical significance was set at p<0.05.
RESULTS
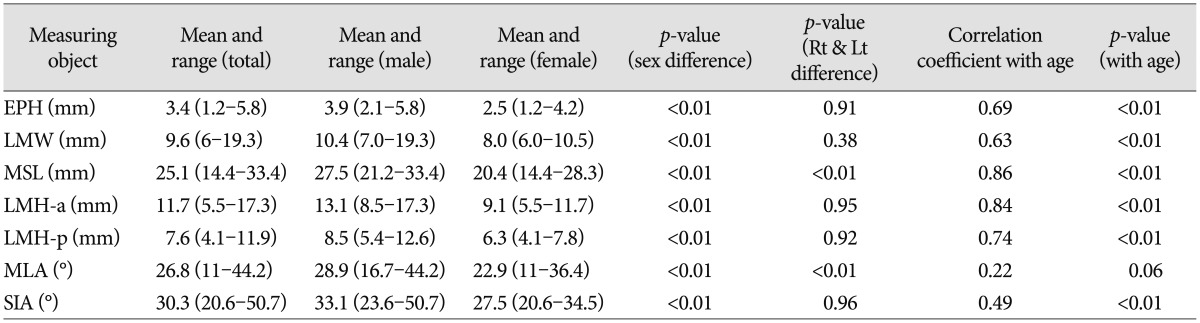
There were no statistically significant differences between low-weight and normal to over-weight group in any measured C1 dimensions (p=0.30-0.93).Table 1 shows the mean value and other values for C1 anatomic measurements. Patients older than 20-months had values more than 3.5 mm greater than younger patients with significant difference in EPH (p<0.02). For C1 EPH, 47.3% (35/74, range, 1.2-5.8 mm) were larger than 3.5 mm and all dimensions were larger than 3.5 mm in the LMH (range, 6-19.3 mm). The mean value of C1 posterior arch height was 3.57 mm (right : 3.59, left : 3.55). Statistically significant differences between right and left dimensions were only found for MSL (p<0.01) and MLA (p<0.02). All measured C1 dimensions showed statistically significant differences between males and females (p<0.01). All measured C1 dimensions showed strong or moderately positive Pearson's correlation coefficient values with older age, but MLA showed weakly positive values with no statistical significance (p=0.06). MSL and LMH-a dimensions had the strongest correlation values (0.86, 0.84, respectively).
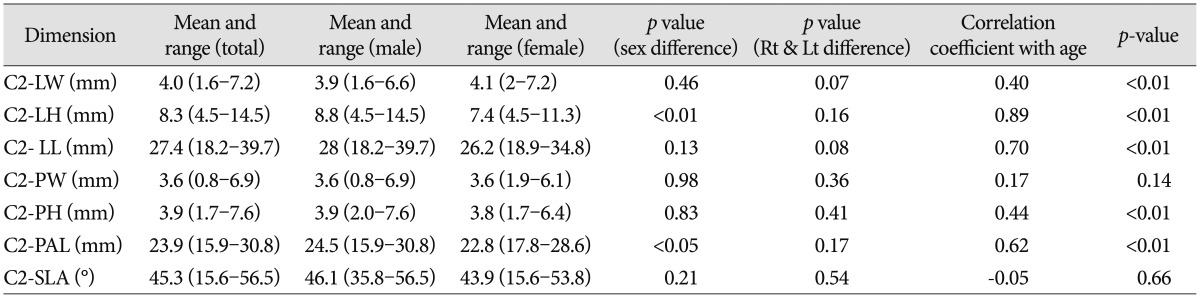
C2 anatomic measurements are described in Table 2. There were no statistically significant differences between low-weight and normal-weight groups in any measured C2 dimension, except the C2-SLA dimension (p<0.01). Mean SLA was 45.3° (range, 15.6-56.5). Patients older than 30-months had values that were greater than 3.5 mm values than those of younger patients, with significance at C2-LW and C2-PW (p<0.01). For C2-LW, 68.8% (51/74) were thicker than 3.5 mm, and all lamina height were larger than 3.5 mm (range, 4.5-14.5). The shortest lamina screw purchase length was measured as 18.2 mm. For pedicle width, 55.4% (41/74) of cases were larger than 3.5 mm, while 58.1% (43/74) of pedicle heights were larger than 3.5 mm. However, only 31 (41.8%) cases met the criteria for 3.5 mm screw application when both pedicle width and height were considered. No patients had lamina or pedicle length less than 14 mm.
No measured C2 dimensions had statistically significant differences between right and left dimensions (p=0.07-0.54). Statistically significant differences were only found between male and female dimensions for C2-LH (p<0.01) and C2-PAL (p<0.05). All measured C2 dimensions showed strong or moderately positive Pearson's correlation coefficient values with older age, except the C2-PW and C2-SLA dimensions. C2-LH, C2-LL, and C2-PAL dimensions had strong correlation with age, while C2-LW and C2-PH had moderate correlation with age.
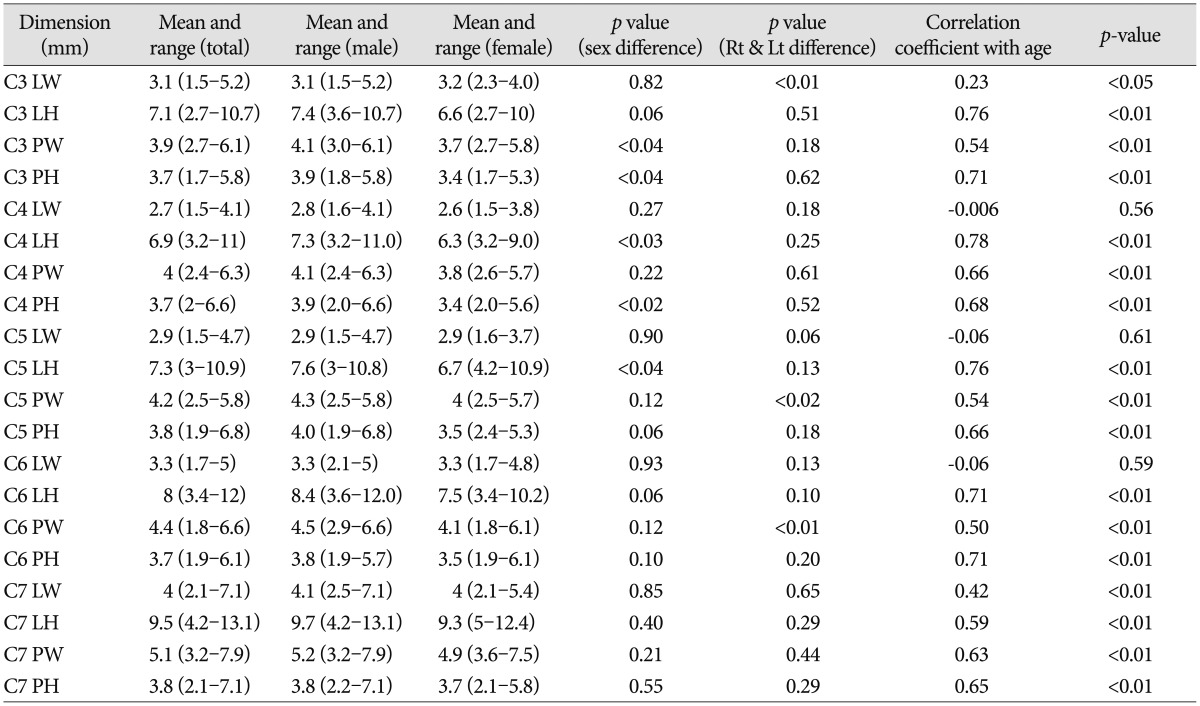
Subaxial cervical vertebrae measurements are described in Table 3. There were no statistically significant differences between low-weight and normal-weight groups in any subaxial cervical vertebrae. Mean pedicle width was 3.9 mm (C3), 4.0 mm (C4), 4.2 mm (C5), 4.4 mm (C6), 5.1 mm (C7). Mean pedicle height was 3.7 mm (C3), 3.7 mm (C4), 3.8 mm (C5), 3.7 mm (C6), 3.8 mm (C7). For pedicle width, 75.7% (C3), 73% (C4), 82.4% (C5), 89.2% (C6), and 98.1% (C7, 1/54) were greater than 3.5 mm. For pedicle height, 62.2% (C3), 58.1% (C4), 63.5% (C5), 64.9% (C6), and 67.6% (C7) were greater than 3.5 mm. Mean lamina width was 3.1 mm (C3), 2.7 mm (C4), 2.9 mm (C5), 3.8 mm (C6), and 4.0 mm (C7), respectively. Only 34.6% (127/370) of subaxial (C3-7) lamina thickness were greater than 3.5 mm. Mean lamina height was 7.0 mm (C3), 6.9 mm (C4), 7.3 mm (C5), 8.0 mm (C6), and 9.5 mm (C7). Mean lateral mass length for ideal screw placement was 9.28 mm (C3), 9.08 mm (C4), 8.81 mm (C5), 8.98 mm (C6), and 10.38 mm (C7).
Only C3 LW (p<0.008), C5 PW (p<0.019) and C6 PW (p<0.01) had statistically significant differences between the right and left dimensions. Statistically significant differences between male and female dimensions were found for C3-PW (p<0.05), C3-PH (p<0.05), C4-LH (p<0.05), C4-PH (p<0.05), and C5-LH (p<0.05). For LML, 41.9% (31/74, C3), 44.6% (33/74, C4), 55.4% (41/74, C5), and 33.8% (25/74, C6) were larger than 9 mm. All measured subaxial dimensions showed strong or moderately positive Pearson's correlation coefficient values with older age, except C4 LW, C5 LW, and C6 LW dimensions.
DISCUSSION
In recent years, many techniques for screw fixation of the cervical spine have become available for the adult population. Traditional wiring techniques are biomechanically inferior to screw-based techniques, and immobilization after surgery may be more difficult for pediatric patients8,12,19,21) Therefore, the anatomical dimensions of the whole cervical spine must be investigated to study the safety of screw fixation. The suggested minimum thickness needed to allow safe placement of a screw varies in the literature4,5,18,23).
Applicability of a C1 lateral mass screw fixation technique to the pediatric population is essential to avoid unnecessary fusions to the occiput and to limit caudal subaxial extension for occipitocervical fusion cases. Recently, the clinical use of C1 lateral mass screws was published2,14). If LMH-a is considered an upper edge and LMH-p a bottom edge, the C1 lateral mass is trapezoid faced with a medial trajectory. The C1 lateral mass also faced to more superior direction. Therefore, maximal screw fixation purchase can be obtained with a supero-medial trajectory. Fixation with an least 14.4 mm screw length was possible in this study. There were no restrictions to 3.5 mm screw fixation purchase in the LMW aspect. Chamoun et al.4) reported that only 1 of 152 cases had LMW less than 4 mm in 152 studies. The only anatomical restrictive factor for C1 lateral mass screw fixation in our study was EPH. Only 47.3% of patients had sufficient space for 3.5 mm screw fixation in situ. However this limitation can be overcome by using an inferior C1 arch notching technique. Practically all patients showed sufficient space for 3.5 mm screw fixation, when we measuring C1 posterior arch height (mean value of EPH add C1 posterior arch right : 6.9, left : 6.9, range : 3.9-11.1 mm). Therefore, pe-diatric patients may have more anatomical space to purchase C1 screw fixation, when considering C1 arch as a additional space.
Generally, the left and right lateral mass had symmetrical morphological features regarding whole measured dimensions, excluding the MSL and MLA dimensions. Variability in C1 transverse foramen size and position may play a key role in limiting the lateral margin for measuring MLA and MSL. All C1 morphologic dimensions for boys were larger than for girl's in our study, indicating that particular cautions should be used when deciding on surgical plans in girls. We infer that C1 lateral mass dimensions changes with age, excluding MLA dimensions. As mentioned before, variability in the C1 transverse foramen may induce these results.
The most representative techniques for C2 vertebrae are pedicle screw fixation and trans-lamina screw fixation. Pedicle screw fixation techniques are more widely used in the adult population, but the clinical applicability of trans-lamina screw fixation also has also been announced in recent years3,5). Leonard and Wright17) first introduced trans-lamina screws for C2 in adults and pediatric patients (1 patient less than 10 years old). This technique has been extended to the entire subaxial cervical spine in the general adult population10,11). Chamoun et al.3) reported the successful use of C2 and subaxial trans-lamima screw fixation in 6 pediatric patients younger than 10 years old.
Trans-lamina screw fixation was preferable to pedicle screw fixation in our study and many previous reports showed similar results6,7,20). There was no restriction in 3.5 mm screw fixation regarding the C2-LH aspect in our study. C2-LW plays a key role in permitting 3.5 mm screw fixation in our study (68.8% possible). However, both pedicle width and height were restrictive factors in pedicle screw fixation (55.4% and 58.1%, respectively). The possibility of pedicle screw fixation decreased to 41.8%, when both pedicle height and width were considered. C2 pedicle screw fixation involve more risk of injury to the vertebral artery and can be more technically challenging than C2 trans-lamina screw fixation.
All measured C2 dimensions in our study showed symmetrical morphology. Only C2-LH (p<0.01) and C2-PAL (p<0.05) dimensions were statistically related to sex. In clinical practice, C2-LH and C2-PAL have sufficient length for screw fixation. Therefore, surgical plans did not change based on sex. We infer that all C2 dimensions changes with age, except C2-PW and C2-SLA. Pedicle width is the most problematic anatomic structure in older patients.
After Abumi et al.1) first reported the clinical results of pedicle screw fixation for the subaxial cervical spine, many clinical applications have been executed in adult patients. Recently, Rajasekaran et al.23) reported that safe insertion of pedicle screw is possible in pediatric patients. Vara and Thompson25) performed a cadaveric study of pediatric cervical pedicle width [mean value : 3.63 mm (C3), 3.73 mm (C4), 4.10 mm (C5), 4.58 mm (C6), 5.15 mm (C7)] with results similar ours.
Some studies showed that PH is larger than PW in the adult population, however our results were contrary15,16,22). PW was lowest at the C3 level and slightly increased with the decreasing level of subaxial cervical vertebrae. PH are nearly similar each other. Generally, PH was the main restrictive factor to purchase screw insertion in our results (Fig. 4C). Only 33 (44.6%, C3), 35 (47.3%, C4), 30 (40.5%, C5), 26 (35.1%, C6), and 25 (33.8%, C7) cases met the criteria for 3.5 mm screw application when both pedicle width and height were considered. PW and PH statistically increased with age at all levels (p<0.01).

Graph demonstrating the mean value of pedicle and lamina dimensions in subaxial spine. PW : pedicle width, PH : pedicle height, LW : lamina width, LH : lamina height.
As with C2 results, LW was the predominant restrictive factor for subaxial trans-lamina screw insertion in our results. The LH aspect of the whole subaxial cervical vertebrae was less than 3.5 mm long in only 6 cases (1.6%, 6/370). In terms of clinical feasibility, 34.6% (128/370) of individual cervical LW were at least 3.5 mm in the present study. Notably, the maximal rate of acceptance occurred at C7 and the minimum was at C4. When both lamina and height were considered, 23 (31.1%, C3), 11 (14.9%, C4), 15 (20.3%, C5), 26 (35.1%, C6), and 53 (71.6%, C7) cases of trans-lamina screw fixation were possible. Only LW did not increase with age at C4, C5, and C6 levels.
Our results indicate that pedicle screw fixation is generally preferable in the subaxial cervical spine, except at the C7 vertebra. Clinically, trans-lamina screw fixation is rarer than pedicle screw fixation in pediatric subaxial spines1,13,23).
Although many previous reports have suggested that lateral mass screw fixation results in excellent stability and lower complication rates, only a few reports have been published regarding the use of subaxial lateral mass screws in pediatrics24). Sekhon24) suggested that a minimun subaxial lateral mass screw length of 14 mm is needed to confer any substantial degree of biomechanical stability in adults. However, Hedequist et al.9) reported high fusion rate and low complication rate for lateral mass screw fixation using minimum 10 mm screws in children. Subaxial LML is the most difficult measurement target, because many lateral mass screw fixation technique are the bidirectional (laterally and cephalad). Solitary axial or sagittal images cannot satisfactorily represent three-dimensional images. The usual posterior surface of the C7 lateral mass is small and uneven, so an imaginary line of lateral mass screw fixation has lateral direction violations. An axial image was used to measure LML, so the actual length may be greater than the measured length. If C7 measurements are excluded, 43.9% (130/296, from C3 to C6) of LML showed were greater than 9 mm. Left and right subaxial cervical spine generally had symmetrical morphological features, except C3-LW, C5-PW, and C6-PW.
Limitation and interpretation
Pediatric spine has some unique features when comparing with adult spine : 1) soft bone quality, 2) cancellous bone is less developed. And, we consider the potential problem derived from the metal implant (toxicity) to the pediatric people. Therefore, it will be not so easy to apply present data to the clinical field directly.
Our sample size was relatively small, and may have been insufficient to represent the general pediatric population. Although we tried to overcome two-dimensional representation with scout image view skill, CT-based studies have limitations in translating three-dimensional cervical spine morphology. All measured data would be more reliable with intra and inter-observer variability tests.
CONCLUSION
C1 lateral mass fixation could be limited by the morphometrics of lateral mass entry point height. However, notching technique of C1 arch can make C1 lateral mass screw possible in all pediatric population. C2 trans-lamina approach is preferable to C2 pedicle screw fixation, because all C2-LH dimensions exceeded 3.5 mm. Patients older than 30 months may have sufficient bony space for C1 lateral mass, C2 pedicle screw, and C2 trans-laminar screw placement. Pedicle height values are not significantly different from each level, but pedicle width value tended to increase from C3 to C7 in the subaxial cervical spine. In subaxial spines, pedicle screw placement was preferable to trans-lamina screw placement, except at C7. The possibility of subaxial lateral mass screw fixation must be investigated with more tailored method.