Cerebral Toxoplasmosis Combined with Disseminated Tuberculosis
Article information
Abstract
A 24-year-old man presented with mental change, fever, abdominal pain, tenderness and palpable mass on the lower abdomen. He was a non-Korean engineer and did not accompany a legal guardian, so medical history taking was difficult due to his mental status. Brain magnetic resonance imaging showed multiple rim-enhanced lesions of the brain, and abdominal computed tomography showed huge paraspinal abscess. Chest X-ray and computed tomography showed poorly defined nodular opacities. We initially thought that this patient was infected with toxoplasmosis with typical cerebral image finding and immunoglobulin laboratory finding of cerebrospinal fluid and serum study. The abdominal abscess was confirmed as tuberculosis through the pathologic finding of caseous necrosis. We used anti-tuberculosis medication and anti-toxoplasmosis medication for almost 4 months, and then his clinical state and radiological findings were considerably improved.
INTRODUCTION
Recently, the number of immigrant workers increased in the Republic of Korea. The majority of these people are from different environments such as tropical climate. They may have carried various infectious diseases, which are not indigenous to Korea. One example is toxoplasmosis, an intracellular protozoan parasite infection which is usually found in patients with acquired immune deficiency syndrome3). The disease may be associated with various clinical outcomes5). This paper reports a cerebral toxoplasmosis case with disseminated tuberculosis in an immunocompetent patient.
CASE REPORT
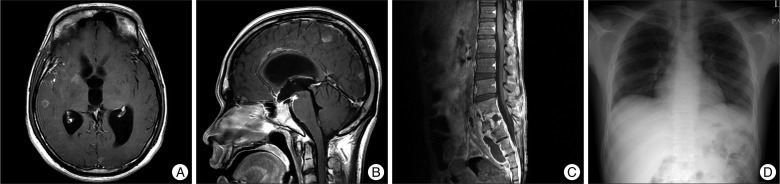
A 24-year-old man was hospitalized because of abdominal pain, vomiting, fever of 38℃ and headache which began 3 days ago. He was an Indonesian engineer who came to Korea for work 6 months ago. He was drowsy and was not accompanied with a legal guardian, so history taking could not be properly performed. A longitudinal 7 cm-sized surgical scar was noticed above the umbilicus on the abdominal midline, and pliable cystic mass was palpable below the left inguinal area. Multiple enlarged anterior neck lymph nodes were palpable with severe tenderness. On neurological examination, he was drowsy and ptosis of the right eye was noticed (Fig. 1). However, his retina study was normal. Non-enhanced brain CT taken on admission showed multiple nodules of subtle high densities and in various sizes, in both cerebral hemispheres and cerebellum with minimal perilesional edema. On brain MRI, there were about 20 rim-enhanced scattered nodules in the whole brain combined with leptomeningeal seeding (Fig. 2). Chest X-ray and CT scan showed diffuse scattering haziness like as miliary pulmonary tuberculosis with right paratracheal lymphadenopathy (Fig. 3). On abdominal CT scan, huge rim-enhancing fluid collection was found in the paraspinal area around the lower lumbar spine, presacral and both iliopsoas muscles. This fluid cyst was herniated to the left inguinal and anterior thigh muscles. Osteolytic lesions and perithecal sac abscess were noticed at L3, L4, L5 and upper sacrum (Fig. 4), but neurological deficit of lower extremities was unclear. At admission, his WBC count was 6250/µL, neutrophil differential count 83%, and HIV antigen negative.
Magnetic resonance imaging at admission shows a multiple rim-enhanced lesion around the whole brain and leptomeningeal seeding.
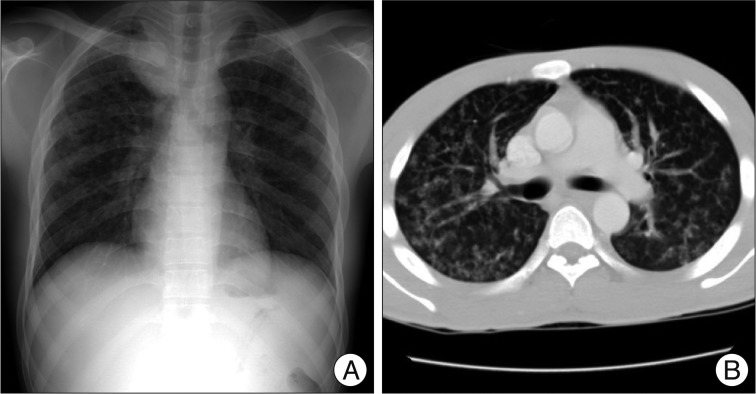
Initial chest X-ray (A) and chest computed tomography (B) show bilateral and poorly defined nodular opacities. This finding suggests pulmonary tuberculosis or toxoplasmosis.
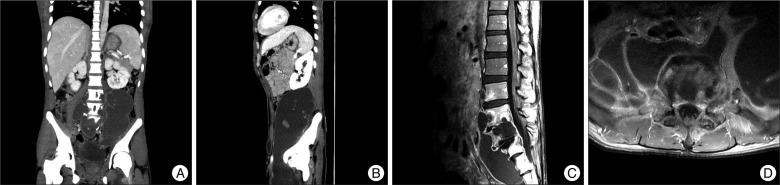
Huge paraspinal abscess are shown on computed tomography (A and B) and magnetic resonance images (C and D). The abscess caused bony erosion and extended into the epidural space.
On hospital day 3, he fell into a deep stupor. On follow up brain CT, cerebral edema was aggravated, and newly developed infectious hydrocephalus was observed. Emergent external ventricular drainage (EVD) was done and left for 2 weeks, and the patient regained his consciousness. On hospital day 30, hydrocephalus recurred, and EVD was performed again. Hydrocephalus did not recur afterwards. Initially, third generation cephalosporin (Ceftriaxone) was administered to the patient. However, fever was persistent, and his general condition was deteriorated. Therefore, laboratory study was performed to find another infectious origin such as tuberculosis, fungus or several parasites with consideration of the patient's epidemiology. As a result, we found positive toxoplasma IgG in serum and CSF, but another culture and immune study results were negative. We started medical therapy for toxoplasmosis, namely Sulfadiazine and Pyrimethamine, for 16 weeks according to the recommendation of the Korea Orphan Drug Center.
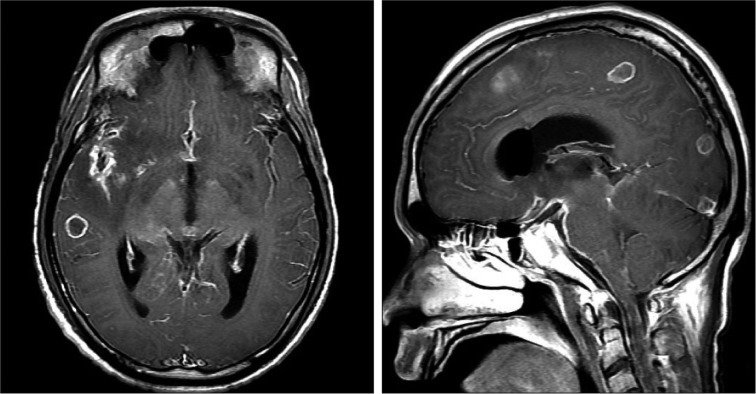
We performed percutaneous drainage of the abdominal cyst. On past history taking, the surgical scar was assumed to have been made when removing an abscess 2 years ago. Initially, we used pigtail catheter to drain the abdominal abscess. The abscess was white and yellowish in color and very thick and sticky, so it was not drained. So, we made another large incision and performed drainage again. Then, subtotal abdominal abscess was removed in hospital day 45. On culture study, there was no microorganism, and acid-fast bacilli were not detected by Ziehl-Neelsen stain. However, typical caseous necrosis was noticed without positive results of sputum culture and polymerase chain reaction for acid-fast bacilli. Clinical and radiological evidence also suggested the possibility of tuberculosis. Thus, we administered medication for anti-tuberculosis and toxoplasmosis for nearly 4 months. As a result, the patient's clinical and radiological outcomes were improved. Three months later, the size and number of enhanced nodules were decreased on brain MRI. Chest X-ray showed improvement of diffuse haziness and the abdominal abscess considerably decreased in size (Fig. 5). He gained his consciousness with minimal cognitive impairment and could walk by himself.
DISCUSSION
Toxoplasma gondii is an intracellular protozoan parasite1). Humans become infected with this parasite through 3 ways : by ingesting bradyzoites in undercooked meat of infected food animals; by ingesting sporozoites in water which has been contaminated by garden soil containing infected cat feces; or congenital transplacental transmission3). The infection causes various clinical outcomes. Since the immune system of healthy people can effectively fight this infection, a small number of people present with toxoplasmosis. Most symptoms of toxoplasmosis are mild such as flu-like symptoms, lymphadenopathy and myalgia1). However, in rare cases, mainly in immunocompromised patient such as those with acquired immune deficiency syndrome4), severe neurological or ophthalmological complications are presented3,9). Since our patient was immunocompetent (negative for HIV antigen), it may be that toxoplasma which had been dormant in the past was manifested with severe symptoms once the patient's general condition deteriorated. In the laboratory results of serum, toxoplasma IgG was positive, but IgM was negative. This suggests that our patient was not in an acute stage of the first time infection but had been infected a long time ago.
Cerebral toxoplasmosis may be fatal. Most typical manifestations of fatal neurological toxoplasmosis are intracranial calcifications and choroidoretinitis7). Although these complications were weakly presented in our patient, it can affect intellectual function. In some regions, up to 9% of cases of mental retardation are associated with toxoplasmosis2). We did not examine the patient's intellectual function because he was drowsy when he first presented, hindering communication with the patient. It was challenging to diagnose cerebral toxoplasmosis based on MRI findings, because, on cranial imaging, it is very similar to central nervous system (CNS) lymphoma, primary and metastatic CNS tumors, or other intracranial infections like tuberculoma or abscesses8). On brain-MRI, our patient presented an eccentric target sign which is typically noticed in tuberculosis and toxoplasmosis. For the differential diagnosis, we performed additional study and consulted with the Korea Centers for Disease Control and Prevention. As a result, we decided that this case was cerebral toxoplasmosis with combined with paraspinal tuberculosis. There were three pieces of evidence of cerebral toxoplasmosis : 1) IgG antibody to toxoplasmosis was positive in serum and CSF; 2) IgG avidity test was highly positive in serum and CSF, indicating that the patient was exposed to Toxoplasma gondii within at least 5 months; 3) toxoplasmosis polymerase chain reaction was positive. In addition, in our case, we detected caseous necrosis from the pathologic study of abdominal abscess. There was a surgical scar on the abdomen. Since the patient's condition did not allow communication, it was difficult to check his surgical history about the wound. The only piece of information the patient provided us about the scar was that it was due to surgery for "any inflammation" which was performed several years ago. Therefore, we assumed that the abscess of tuberculosis recurred this time. The assumption also provided a possible explanation that the patient's immune system might have been impaired because of tuberculosis10), which in turn triggered latent toxoplasmosis to be manifested3).
Toxoplasmosis usually affects the lungs in immunosuppressed patients6,11), and such lung involvement can be confused with pulmonary tuberculosis. It was confusing with our patient too as his abdominal abscess revealed caseous necrosis in pathologic finding and his chest imaging showed typical signs for disseminated pulmonary tuberculosis such as bilateral, symmetric, coarse and poorly defined nodular opacities. However, there were no laboratory results to support the diagnosis of pulmonary tuberculosis. Based on our impression that the patient had either pulmonary toxoplasmosis or tuberculosis, we administered both anti-toxoplamosis and anti-tuberculosis medications, and the finding of pulmonary images study was improved. The abdominal abscess also decreased after continuous drainage and medication therapy.
CONCLUSION
We report a very rare case of cerebral toxoplasmosis in Korea. As the country is increasingly becoming multicultural, various new parasitic infections should be investigated whenever suspected. Particularly, people should be aware of the fact that toxoplasmosis can occur in immunocompetent patients and coincide with any other infection such as tuberculosis.