Endovascular Treatment of Symptomatic High-Flow Vertebral Arteriovenous Fistula as a Complication after C1 Screw Insertion
Article information
Abstract
High-flow vertebral arteriovenous fistulas (VAVF) are rare complications of cervical spine surgery and characterized by iatrogenic direct-communication of the extracranial vertebral artery (VA) to the surrounding venous plexuses. The authors describe two patients with VAVF presenting with ischemic presentation after C1 pedicle screw insertion for a treatment of C2 fracture and nontraumatic atlatoaxial subluxation. The first patient presented with drowsy consciousness with blurred vision. The diffusion MRI showed an acute infarction on bilateral cerebellum and occipital lobes. The second patient presented with pulsatile tinnitus, dysarthria and a subjective weakness and numbness of extremities. In both cases, digital subtraction angiography demonstrated high-flow direct VAVFs adjacent to C1 screws. The VAVF of the second case occurred near the left posterior inferior cerebellar artery originated from the persistent first intersegmental artery of the left VA. Both cases were successfully treated by complete occlusion of the fistulous portion and the involved segment of the left VA using endovascular coil embolization. The authors reviewed the VAVFs after the upper-cervical spine surgery including C1 screw insertion and the feasibility with the attention notes of its endovascular treatment.
INTRODUCTION
High-flow vertebral arteriovenous fistula (VAVF) can rarely occur by an unintended vertebral artery injury caused by penetrating accidents, injuries of the cervical spine or medical procedures5,6,12). Owing to the course of the vertebral artery (VA) and the complexity of the anatomy of the posterior skull base and C1-2 areas, the posterior C1 or C2 screw insertion has a potential risk of vertebral artery injury. Those lesions are associated with serious neurologic complications such as cerebral ischemia caused by arterial steal or thromboembolic events, neck mass, delayed hemorrhage by arterial dissection, pseudoaneurysm or heart failure especially in infants13,21,22). The endovascular treatment (EVT) has been firstly selected for VAVFs. Considering the complexity of VAVFs, it is important to understand anatomical factors influencing EVT such as normal or related abnormal vascular structures on the craniovertebral junction (CVJ)6,13,21). Herein, we report our experiences with two cases successfully treated by endovascular coil embolization of high-flow VAVF caused by C1 screw insertion.
CASE REPORT
Case 1
A 57-year-old woman presented with severe neck pain after a pedestrian traffic accident. The initial neurologic examination showed symmetrical motor power without any sensory changes in the extremities. Plane films and computed tomography of her cervical spine demonstrated a C2 fracture involving the bilateral (mainly left) C2 pedicle and a lateral mass extending into the base of the odontoid process. The preoperative magnetic resonance imaging (MRI) did not demonstrate any abnormal course and relationship of the VA and adjacent structures.
The patient underwent a bilateral pedicle screw fixation between C1, C2, and C3. The operative procedures through posterior approach were uneventfully completed. Six days after operation, she complained of an abrupt and severe nuchal pain and blurred vision. She deteriorated the symptoms and showed dysarthria, right facial palsy and drowsy consciousness. The diffusion MRI of the brain showed a multifocal acute infarction in the bilateral cerebellar hemisphere and the bilateral occipital lobes. The digital subtraction angiography (DSA) demonstrated high-flow VAVF between the V3 segment of the left VA above the pedicle screw located left C1 and the paravertebral venous plexus (Fig. 1A). The VAVF was also fed by a backward flow from the right VA. The blood supplies from the right VA to posterior circulation were sufficiently accounted. Therefore, a complete occlusion of the left VA involving the VAVF using EVT was decided to prevent an aggravating ischemic symptom due to arterial steal and thromboembolism caused by VAVF.

Case 1. The pretreatment angiography (A) demonstrates high-flow arteriovenous fistula at the V3 segment of the left vertebral artery above the screw inserted left C1 pedicle. The left V3 segment including the fistulous segment was complete occluded by endovascular coil embolization (B). The posttreatment angiography (C) demonstrates a complete obliteration of the fistula and occlusion of the V3 segment.
Under local anesthesia, a single microcatheter approached via 5 Fr guiding catheter located the left VA was easily passed from the proximal part of the fistula to the distal V3. The V3 segment of the left VA was complete occluded by four detachable coils and ten pushable coils (Fig. 1B). The angiography revealed a complete obliteration of the fistula and occlusion of the V3 segment of the left VA (Fig. 1C). The patient had an unremarkable post-procedural course without further aggravation of the symptoms relating to a cerebral ischemia or VAVF. She was gradually improv-ed and was discharged two weeks after the procedure. Two months after the embolization, the follow-up angiography showed stable occlusion of the VAVF. During 32 months follow-up, there were no new symptoms and lesions at the imaging studies.
Case 2
A 45-year-old woman presented with numbness and recurrently transient weakness of her left extremities. The brain MRI showed no ischemic lesions on brain. However, the MRI of the cervical spine revealed an increasing atlanto-dental interval (ADI) with compromising the central canal at the C1 level. A CT angiography (CTA) of the cervical spine revealed an unusual course of the bilateral V3, a so-called persistent first intersegmental artery (PFIA). The horizontal part of the bilateral V3 begun from not C1 vertebral foramen but C2 vertebral foramen and was placed between the C1 and C2 posterior arches. For the stabilization of the atlanto-axial subluxation, the patient underwent a bilateral screw fixation between C1 and C2 using pedicle the screw insertion technique. During the careful dissection of the left C1 lateral mass, a relatively large volume of arterial bleeding was encountered, which was immediately controlled by compression using gelform and bone wax. The remaining surgical procedures were uneventfully finished.
Immediately after the recovery from anesthesia, the patient complained of pulsatile tinnitus on the left ear. Four days later, she additionally presented with vertigo, nausea, dysarthria and subjective weakness and numbness of extremities. The DSA demonstrated a high-flow VAVF between the V3 segment of the left VA and the paravertebral venous plexus (Fig. 2A). The venous regurgitations from the fistula were extended into the left sigmoid and inferior petrosal sinus. The posterior circulations including the left PICA were only supplied by the right VA due to transection and arterial stealing at the fistula. The VAVF was also fed by a backward flow from the right VA. The angiography also confirmed two anomalies of the bilateral VA: 1) the bilateral PICA originating from VA between C1-2; 2) the bilateral PFIA. A complete occlusion from the distal to proximal segment of VA involving fistulas was decided to improve her symptoms due to vertebrobasilar insufficiency and venous hypertension caused by high-flow VAVF.
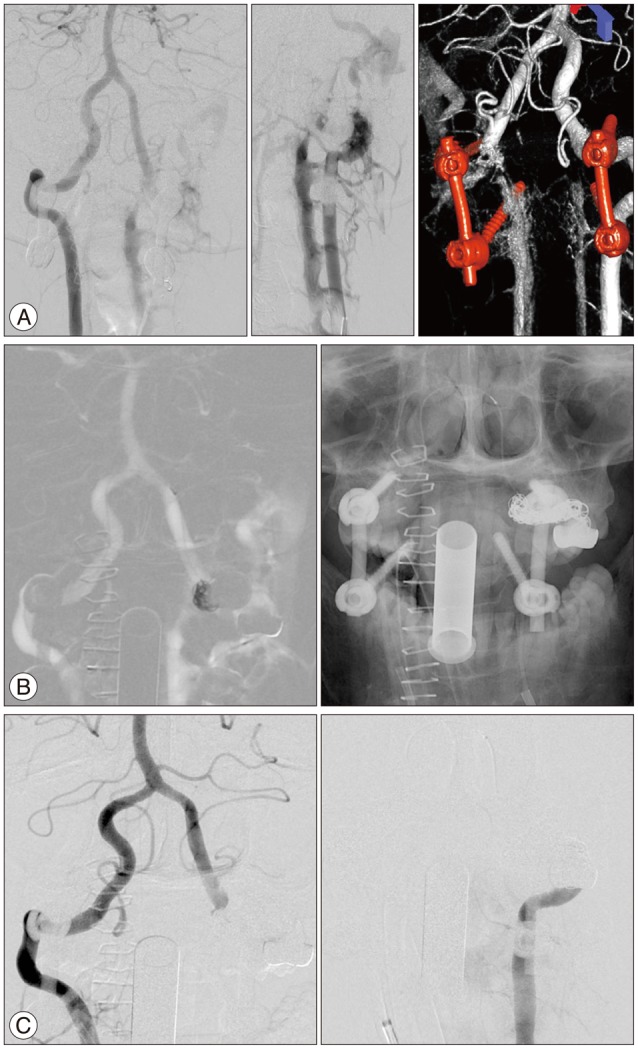
Case 2. The pretreatment angiography (A) demonstrates a high-flow arteriovenous fistula with transection between the V3 segment of the left vertebral artery and the paravertebral venous plexus with the venous regurgitations extending into the left sigmoid and inferior petrosal sinus. The 3D image (A, right) reveals the left posterior inferior cerebellar artery (PICA) originating from extradural segment near the fistula. The two microcatheters were navigated to the distal and proximal protion of the fistula for saving the left PICA and supporting coil-frames (B). The posttreatment angiography (C) demonstrates a complete obliteration of the fistula with saving the left PICA.
Under general anesthesia, bilateral femoral arteries were punctured. For using the double-microcatheter technique to approach the distal part of the fistula from right VA and proximal part of the fistula from left VA, two 5 Fr guiding catheter were placed into the proximal segment of the right and left vertebral arteries. The first microcatheter was navigated to the distal portion of the fistula via vertebrobasilar junction from the right VA. Subsequently, the second microcatheter was placed on the proximal portion of the fistula via the left VA. An initial coil-frame was made from one detachable coil inserted through the first microcatheter. The first frame was placed between just the distal segment of the fistula and the left PICA (Fig. 2B). Two detachable coils and four pushable coils were inserted through the second microcatheter. For saving the left PICA and supporting other coil-frames, the initial coil-frame had not been detached until the proximal segment of the fistula was occluded. Although the fistula from the left VA was completely occluded, the right VA angiography showed a remaining of the fistula through the distal portion of the VAVF. After detaching the initial frame, another detachable coil was inserted via the first microcatheter. The bilateral VA angiography showed a complete obliteration of the orifice of VAVF and venous refluxes (Fig. 2C). Immediately after the recovery from general anesthesia, her tinnitus was completely disappeared. The patient was discharged to home at the fifth post-procedural day without neurological changes. The three months later, the CTA of the cervical spine revealed a stable occlusion of the VAVF. During a follow up period of six months, the patient had no further neurologic signs or symptoms.
DISCUSSION
VAVFs are rare lesions caused by traumatic or spontaneous origin. Penetrating neck injuries are frequently associated with the lesions; however, a dislocation or fracture of the cervical spine and iatrogenic causes such as central line insertion or cervical spine surgery are also associated 3,4,6,7,8,12,18). In the literature, the rates of VA injuries during spine surgeries were accounted for approximately 2-8%. The risk of neurological deficits from those injuries was presented as 0.2% per patient, and the mortality was presented as 0.1%11,12,19). Although an uncommon occasion, a VAVF during a cervical spine surgery is a very serious complication causing neurologic deficits due to cerebral ischemia or vertebrobasilar insufficiency and other presentations such as cervical myelopathy, tinnitus, neck mass and even death3,12,13,21,22). In our first case, although the direct injury by C1 screw was not observed during operation, we supposed that the VAVF were developed by the injury on the basis of the angiographic findings. The cause of delayed neurologic presentation of the first patient could have resulted from the widening of the channel and the aggravation of the steal phenomenon after the initial small fistula formation.
The V3 segment is anatomically complicated and is also associated with several congenital or acquired vascular-anomalies such as PFIA, fenestration of VA, PICA from C1-2 and high-riding VA, etc. Some reports suggest that congenital or acquired disorders such as Down or Klippel-Feil syndrome, neurofibromatosis, fibromuscular dysplasia, atlantoaxial dislocation, or rheumatoid arthritis are predominant risk factors for the presence of such vascular anomalies5,16,17). These variations also have been reported in 1-5% of the normal population 15,17,20). Therefore, preoperative angiographic studies such as CTA or DSA with 3-dimensional bony reconstruction for acknowledging the vessel-bone relationships are mandatory to predict the surgical risk. In our second case, we predicted such risk from the preoperative CTA; however, a VA injury occurred during the dissection. A thorough understanding of the surgical anatomy, a gentle dissection avoiding a vessel injury and helpful modalities such as a navigation system or a intraoperative CTA could be reducing the risk during surgery in the CVJ.
Owing to the advantages compared with the surgical repair such as shorter procedure and recovery time, smaller risk of bleeding and infection and immediately obtaining angiographic results after the procedure, EVT have been accepted the first option for VAVFs. From the literature and our cases, EVT provided good clinical and angiographic results without significant morbidity4,7,8,9,14,18). Immediate or delayed occlusion rates were reported for approximately 90% of lesions6). Detachable or non-detachable coils, detachable balloons, covered stent, vascular plugs, glue or Onyx were used for the obliteration of VAVFs. The use of detachable coils has been considered as a safe and effective method by its retrievability, trackability and diversity of sizes2,10,18). However, misplacement or migration of embolic materials, fistula recurrence and cerebral ischemia or infarction caused by thromboembolism or vertebrobasilar insufficiency remain as the concerns and require a long-term follow-up.
There are some considerations of EVT for VAVFs. First, the best goal of treatment is to completely occlude the fistula channels and preserve the patency of the VA. However, if the high-flow VAVFs demonstrated a transection of the VA, an extensive damage of the vessel wall or multiple influx channels, preserving the parent artery may be impossible and a vascular sacrifice may be necessary. In the presented two cases, we have chosed trapping the influenced VA for the complete occlusion of the influx channels of VAVFs. In case of a patent contralateral VA or sufficient collateral supplies via posterior communicating artery, an influencing VA can be completely occluded to prevent further complications1,13). If tolerable for the patients, a balloon test occlusion of the influencing VA could provide the clinical tolerability and vascular susceptibility of inflow via contralateral VA or other collateral supplies1,8). And second, technical aspects to save critical branches near the VAVFs with complete obliteration are still of concern. A double microcatheter technique via bilateral VA approach is useful in some cases presenting with difficult geometry. The use of a single microcatheter might be difficult to navigate the whole influencing segment for high-flow VAVFs with transection or multiple channels. The second microcatheter can be used for the selection of the distal segment of fistula channels and as a physical barrier. In our second case, we firstly kept a distally-located 'undetaching' detachable coil-frame via contralateral VA. It could prevent both supporting of packing coils and avoiding the inadvertent occlusion of branching vessels by herniation or migration of coils. This method may be a safe and effective technique for saving the critical branches such as extradural PICA, anterior spinal artery, or prominent perforating arteries supplying the brain stem. In previous reports, some additional techniques were introduced. The covered stent has been selected for preserving the blood supply of influenced segment of the VA. If any critical artery were not branched from the injured V3 segment, the covered stent could be applied; however, stiffness, poor trackability, unconformity of vessel-caliber and a disruption by neck movement remain as issues of this technique 9). Because of the possibility of an unintended occlusion of arterial branches in applying the covered stent, if the PICA or the anterior spinal artery is originated adjacent the fistula as in our second case, this technique might be reluctantly selected for VAVFs of V3 and V4 segments of a VA. For similar reasons, detachable balloons and vascular plugs for parent VA occlusion were restrictively used for V1 and V2 segments4). In selective cases presenting single or small feeding channels, the transarterial coil embolization with-or-without gluing materials such as Onyx archived good results with preserving the VA2,8,14).
CONCLUSION
The EVT of VAVF is safe and effective in the treatment of the high-flow, complex VAVFs. The detachable coil has its advantages of retrievability, trackability and diversity of its size. Preoperative angiographic studies such as CTA or DSA are essential for understanding the vessel-bone relationships to avoid the risk of VA injury. Furthermore, long-term angiographic follow-ups after the EVT are important for determining the thromboembolic complications and recurrence of fistulas.