Clinical Characteristics of Cerebral Venous Thrombosis in a Single Center in Korea
Article information
Abstract
Objective
The purpose of this study is to investigate the clinical characteristics of cerebral venous thrombosis (CVT) in a single center in Korea.
Methods
A total of 36 patients were diagnosed with CVT from August 2005 to May 2013. The patient data regarding age, sex, disease stage, pathogenesis, location, laboratory findings, radiological findings, and treatment modalities were retrospectively collected. The results were compared with those of previous studies in other countries.
Results
The patient group comprised 21 men and 15 women with a mean age of 46.9 years (ranging from three months to 77 years). The most common cause was a prothrombotic condition (8 patients, 22.2%). Within the patient group, 13 patients (36.1%) had a hemorrhagic infarction, whereas 23 (63.9%) had a venous infarction without hemorrhage. By location, the incidence of hemorrhagic infarction was the highest in the group with a transverse and/or sigmoid sinus thrombosis (n=9); however, the proportion of hemorrhagic infarction was higher in the cortical venous thrombosis group (75%) and the deep venous thrombosis group (100%). By pathogenesis, the incidence of hemorrhagic infarction was the highest in the prothrombotic group (n=6), which was statistically significant (p=0.016).
Conclusion
According to this study, CVT was more prevalent in men, and the peak age group comprised patients in the sixth decade. The most common cause was a prothrombotic condition. This finding was comparable with reports from Europe or America, in which CVT was more common in younger women. Hemorrhagic infarction was more common in the prothrombotic group (p=0.016) than in the non-prothrombotic group in this study.
INTRODUCTION
A cerebral venous thrombosis (CVT) is an uncommon type of stroke accounting for 0.5% of all strokes4). The pathogenesis is multifactorial, and the disease could occur at any age, including in neonates. However, a prothrombotic condition plays a key role in its occurrence. Because of the thrombogenic effect of estrogen, an increased incidence in women who take oral contraceptives as well as in pregnant women has been highlighted in previous reports, particularly in Europe and America where a high use of oral contraceptives has been reported3,18). This study was conducted on the premise that there have been no clinical reviews of CVT in Korea, and, thus the clinical characteristics of 36 CVT patients in a single center were reviewed and compared with those in previous studies.
MATERIALS AND METHODS
From August 2005 to May 2013, 40 patients diagnosed with CVT were treated in a single center. Three patients who were not evaluated for prothrombotic conditions because of personal reasons were excluded from the study group. One patient, who was transferred to another hospital with an incomplete work-up, was excluded, and 36 patients were included in the study. We retrospectively collected these patients' data regarding age, sex, the disease stage, pathogenesis, location, laboratory findings, radiological findings, and treatment modalities such as anticoagulant and/or antiplatelet therapy.
The patients were categorized by age and sex into groups, and the incidence in each group was evaluated. Thorough history taking, physical and neurological examinations, and evaluation of the laboratory and radiological findings were performed in an attempt to identify each patient's pathogenesis.
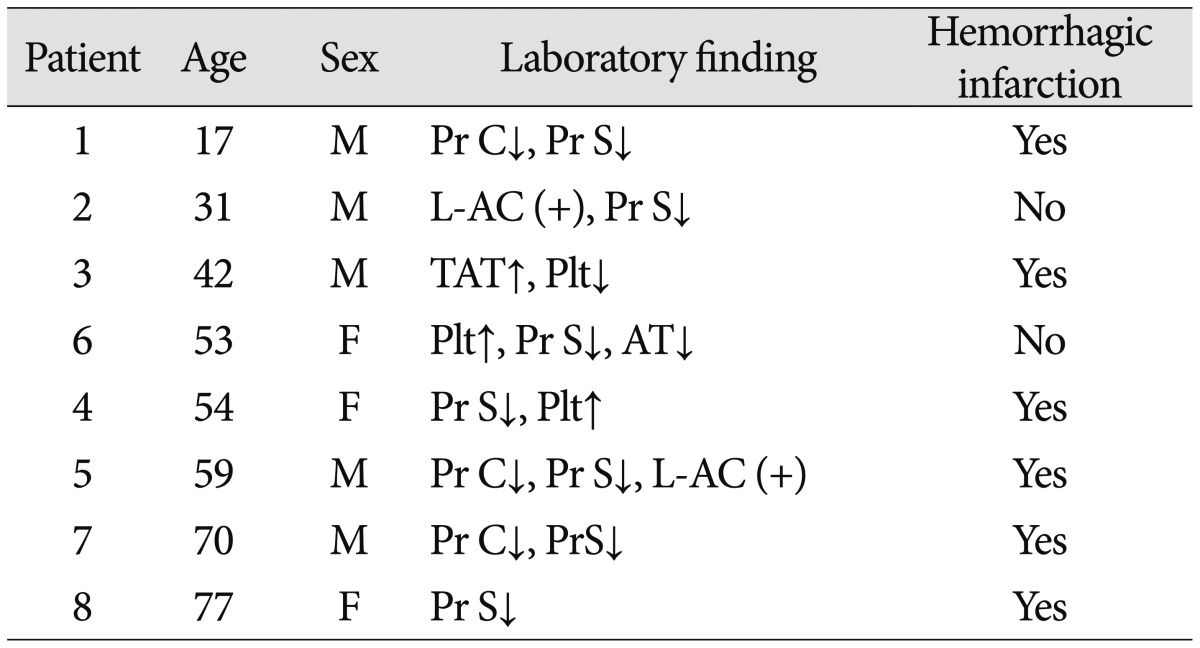
For the evaluation of prothrombotic conditions, blood samples were taken and checked for serum levels of anti-ds-DNA antibody, epithelial neutrophil-activating protein, anti-cardiolipin IgM & IgG, anti-phospholipid IgM & IgG, protein C antigen and activity, protein S antigen and activity, a lupus anticoagulant, thrombin-antithrombin complex, antithrombin III, and the platelet count. Patients with abnormal laboratory values were repeatedly tested after 1 to 2 weeks, and those with consistent abnormal values were regarded to have a prothrombotic condition.
Unless otherwise indicated, a prothrombotic condition was presumed to be the primary cause of CVT in these patients. Cancer, iron-deficiency anemia, and other systemic diseases were assumed to be causative factors in patients with normal laboratory values and without other causes of CVT. The group of patients with normal laboratory values and in whom all known possible causes of CVT were excluded was categorized as the "Idiopathic" group.
The patients who developed a CVT after intracranial surgery were included in the "Post-operative change" group. The diagnoses were incidentally confirmed by a routine post-operative CT or MRI. All the patients were asymptomatic except for a patient who experienced a partial seizure resulting from a left transverse sinus thrombosis after undergoing a suboccipital craniotomy for a left vestibular schwannoma. None of these patients had a procedure-related intracranial infection.
Infection was considered the causative factor for the patients who displayed a definite, localized infection with an adjacent venous sinus thrombosis.
The disease stages were grouped as "Acute", "Subacute", and "Chronic", depending on the time interval between the onset of the clinical symptoms and the time of diagnosis, as proposed by the International Study on Cerebral Venous and Dural Sinuses Thrombosis (ISCVT), which is the largest cohort study conducted on CVT. The period from the onset of symptoms until the time of diagnosis was investigated, and less than 48 hours was designated as "Acute", between 48 hours and 30 days as "Subacute" and more than 30 days as "Chronic"18).
The location of the disease, the presence of hemorrhagic infarctions, and the presence of dural arteriovenous fistulas (AVF) were determined by imaging studies including CT and MRI. The location was divided into the following five groups depending on the primary CVT site : the sigmoid and/or transverse sinus, superior sagittal sinus, cavernous sinus, cortical vein, and deep vein.
First, we attempted to verify the relationship between a hemorrhagic infarction and factors such as the location of the CVT and presence of a dural AVF. Then, we investigated the relationship between different pathogeneses and hemorrhagic infarctions.
Statistical analysis
Fisher's exact test was used to determine any significant relationship between a hemorrhagic infarction and each pathogenesis, the location of the CVT and the presence of a dural AVF. All the analyses were tested at the p<0.05 level of significance, and SAS, Version 9.4 (SAS Institute, Inc., NC, USA) was used for the association analyses.
RESULTS
Patient data
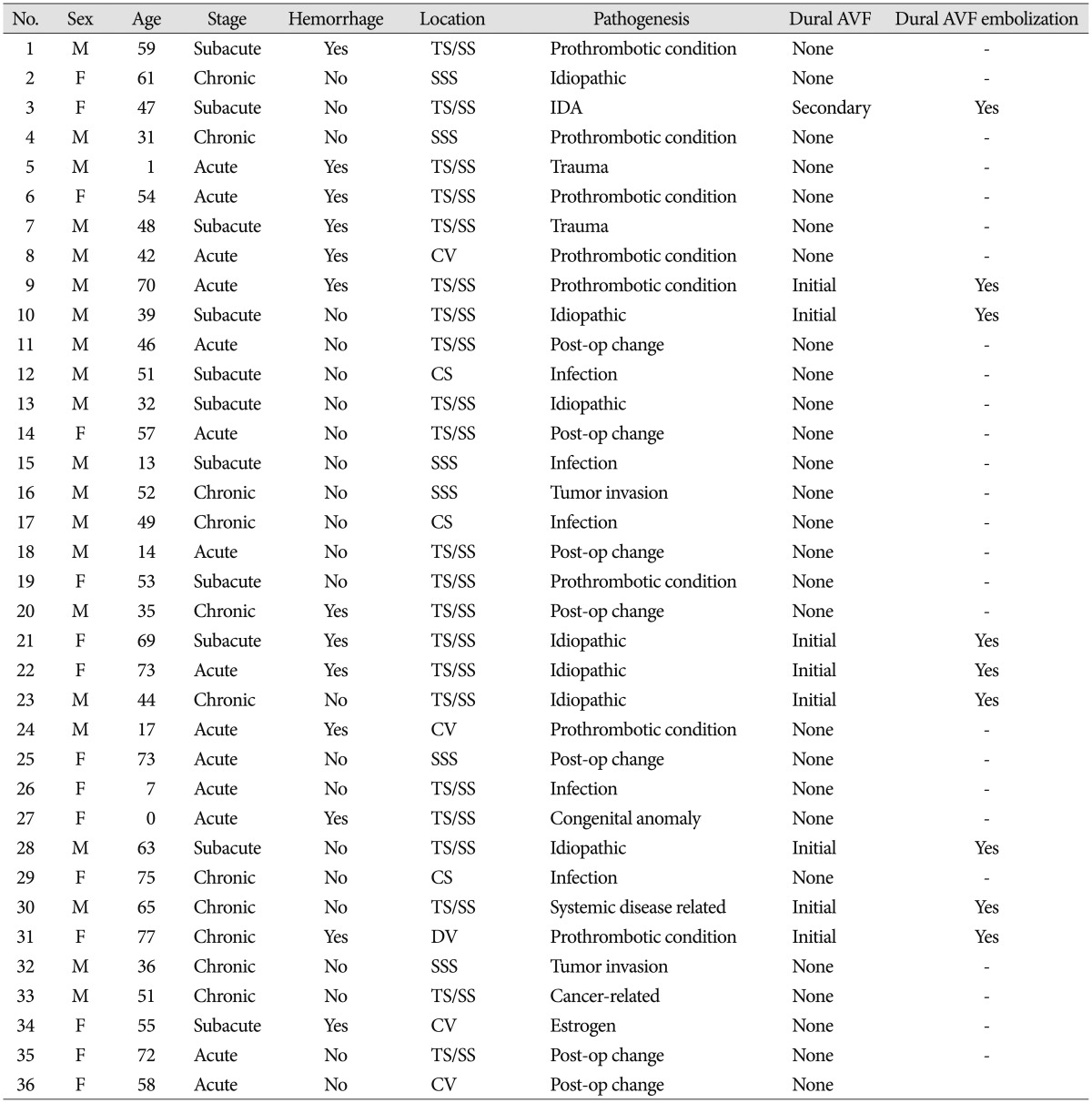
The patient group included 21 men and 15 women with a mean age of 46.9 years at diagnosis (ranging from 3 months to 77 years). In the age groups by decades, the highest prevalence was seen in the sixth decade (n=9).
Within the patient group, 14 (38.9%) patients were in the acute stage at the time of diagnosis, 11 (30.1%) were in the sub-acute stage, and 11 (30.1%) were in the chronic stage.
Concerning the pathogenesis, 8 (22.2%) cases resulted from a prothrombotic condition, 7 (19.4%) were because of a post-operative change, 5 (13.9%) were from an infection, 2 (5.6%) followed a trauma, 2 (5.6%) resulted from local invasion of a preexisting brain tumor, 1 (2.8%) was cancer-related, 1 (2.8%) was related to systemic diseases (chronic renal disease and gout), 1 (2.8%) occurred after hormonal replacement (estradiol hemihydrate) therapy, 1 (2.8%) resulted from a congenital anomaly, and 1 (2.8%) was caused by iron-deficiency anemia. No definitive cause was found in 7 patients (19.4%).
The specific laboratory findings of the 8 patients with a prothrombotic condition are presented in Table 1.
Among the 7 patients in the post-operative change group, 2 patients had undergone a craniotomy for a parasagittal meningioma, 1 for a right occipital skull plasmacytoma, 1 for a left vestibular schwannoma, 1 for a right vagus schwannoma, 1 for a right cerebellar hematoma following an arteriovenous malformation rupture, and 1 for a left cerebellopontine angle meningioma.
In the infection group, the patients had infections in the following locations : a right superior ophthalmic vein thrombophlebitis, a right periorbital abscess and diffuse pachymeningitis, central nervous system aspergillosis, a right otomastoiditis, and a fungal sinusitis with brain abscess.
The radiological findings showed that 13 patients (36.1%) had a hemorrhagic infarction at diagnosis, whereas 23 (63.9%) were without a hemorrhage. None of the hematomas resulted in a severe mass effect that warranted emergency surgical decompression.
A dural AVF was initially present in 8 patients (22.2%) and was newly diagnosed during the follow-up in 1 patient (2.8%). All the patients underwent endovascular dural AVF embolization.
By location, 22 patients had a thrombosis predominantly in the transverse and/or sigmoid sinus, 6 patients mainly in the superior sagittal sinus, 3 patients in the cavernous sinus, 4 patients within the cortical vein, and 1 patient in the deep venous system.
A brief summary of the clinical characteristics of the patients is provided in Table 2.
Relationship with hemorrhagic infarction
Each pathogenesis group was analyzed for an association with hemorrhagic infarction.
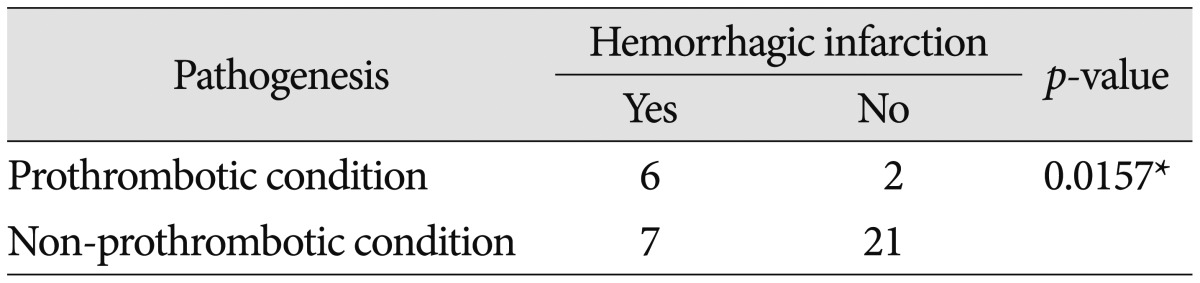
Of the 8 patients in the prothrombotic group, 6 had a hemorrhagic infarction, and 2 had a venous infarction without a hemorrhage. Of the 28 patients in the non-prothrombotic group, 7 patients had a hemorrhagic infarction, whereas 21 had a venous infarction without a hemorrhage. The prothrombotic group had more frequent hemorrhagic infarctions, whereas the non-prothrombotic group had more venous infarctions, which was statistically significant (p=0.016) (Table 3).
The identical analysis was conducted for each pathogenesis entity; the remaining differences were insignificant.
Four of the 9 patients (44.4%) with a dural AVF and 9 of the 27 patients (33.3%) without a dural AVF had a hemorrhagic infarction. The presence of a dural AVF did not have a significant relationship with hemorrhagic infarction (p=0.4097).
Nine of the 22 patients (40.9%) with mainly transverse and/or sigmoid sinus involvement, none of the 6 patients (0%) with mainly superior sagittal sinus involvement, none of the 3 patients (0%) with a cavernous sinus thrombosis, 3 of the 4 patients (75%) with a cortical vein thrombosis and 1 of the 1 patient (100%) with a deep vein thrombosis had a hemorrhagic infarction; however, the relationship between the location and hemorrhagic infarction was not significant (p=0.501, 0.068, 0.288, 0.124, 0.361, respectively). The incidence of hemorrhagic infarction was higher in the group with a transverse and/or sigmoid sinus thrombosis, and the proportion of hemorrhagic infarction was higher in the cortical venous thrombosis and the deep venous thrombosis groups; no noteworthy relationship was observed.
Treatment
Anticoagulants and/or antiplatelets were prescribed for all the possible candidates, regardless of their disease stage. Their therapeutic plans were individualized based on the difference in their presentation, general condition, and accompanying risk of bleeding. Thirteen patients (36.1%) were administered anticoagulant therapy with or without antiplatelets, and 3 patients (8.3%) received antiplatelet therapy only. Twenty patients (55.6%) were not prescribed anticoagulants or antiplatelets; 9 patients had recently undergone a craniotomy, 2 initially had a trauma-related hemorrhagic lesion, 2 had a sizable hemorrhagic infarction at diagnosis, and all these factors added to an increased risk of intracranial hemorrhage. Four patients with a dural AVF without notable intraparenchymal lesions had undergone endovascular sinus occlusion with dural arteriovenous fistula embolization and were not administered additional anticoagulants. Two patients were in a terminal condition and were observed without medication. A 3-month-old patient was not prescribed anticoagulants for safety reasons.
DISCUSSION
The clinical characteristics of 36 Korean patients diagnosed with CVT in a single center were reviewed in this study, which focused on the relationship of hemorrhagic infarction, disease stage, location of CVT, and pathogenesis. The differences with previous reports from other countries have been emphasized.
Pathogenesis
Pregnancy, puerperium and oral contraceptives
Pregnancy and the puerperium are common causes of transient prothrombotic states because pregnancy induces several prothrombotic changes in coagulation. Hypercoagulability is hypothesized to be aggravated after delivery as a result of volume depletion and trauma15). A CVT associated with pregnancy and puerperium accounts for 21% of all the causes of CVT, according to the ISCVT8). Approximately 2% of pregnancy-associated strokes are attributable to CVT10,11). The frequency of puerperium CVT is reported to be approximately 12 cases per 10000 deliveries16). Estrogen-containing oral contraceptives play an important role in the pathogenesis of CVT in young women2,6,14). In most CVT studies, the use of oral contraceptives is the most frequent risk factor in women; the rate of usage was 47% in the ISCVT and as high as 96% in an Italian study3).
In our study group, 1 CVT event was related to estrogen use; none were related to pregnancy. A potential explanation for this finding is that Korea has considerably low crude birth and fertility rates as well as a markedly low usage of oral contraceptives by Korean women compared to that in the United States and many European countries. The crude birth rate (9.6 births per 1000 population) and fertility rate (1.3 births per woman) in Korea are among the lowest in the world22,23). The use of oral pills as a means of contraception in Korea is as low as 2.0%, whereas that rate is tenfold higher in the United States and up to twentyfold higher in many European countries21).
Post-operative change
Iatrogenic injury to the venous sinus during and after surgery near the sinuses might induce CVT, as observed in 7 of our patients. No study has investigated the incidence of iatrogenic CVT following surgery. There have been case reports of CVT after applying topical hemostatic matrix and cauterization at the nearby sinus, as well as studies on the incidence at the remote site after lumbar CSF drainage13,19). In our study group, all of the seven cases displayed localized CVT near the surgical lesion, which implies iatrogenic injury to these sinuses. The assumed causative factors are mannitol and CSF drainage during a craniotomy, which induces hyper-osmolality that aggravates CVT. Overexposure of the sinus leads to desiccation of the dura surrounding the sinus, leading to shrinkage and thrombosis. Retraction against the venous structures might limit blood flow and subsequent stasis and thrombosis. Maintaining adequate hydration and minimizing sinus exposure and retraction against venous structures is necessary during surgery near the sinuses. Dominant sinuses should never be sacrificed, and careful decision-making is required when occluding non-dominant sinuses11). Because iatrogenic CVT might be asymptomatic or present with a headache, which is a non-specific symptom after craniotomy, complete pre-operative and post-operative imaging studies including angiography or venography are essential for the diagnosis of iatrogenic CVT.
Prothrombotic condition
The prothrombotic condition is the most widely studied risk factor for CVT. The incidence of the prothrombotic condition in CVT was reported to be 34.1% in the 624 cases in the ISCVT8,20) and 21% in the 182 cases in a recent multicenter study by de Freitas et al.5). A prothrombotic condition is associated with numerous factors. The roles of antiphospholipid antibodies, anticardiolipin antibodies, natural anticoagulant protein (antithrombin III, proteins C and S) deficiencies, and factor V Leiden gene mutation have been described in past studies1,18). In our patient group, the incidence of a prothrombotic condition was 22%, which is similar to or slightly lesser than in previous studies.
Dural AVF
The relationship between dural AVF incidence and CVT is complex and not completely understood. Thrombosis of the cerebral venous sinus could later induce a dural AVF, as seen in one of our patients, and a pre-existing fistula could be the underlying cause of CVT18). A dural AVF could spontaneously close after the sinus recanalizes. In cases in which a dural AVF is found with the initial diagnosis of CVT, the order of the timing of the two disease entities could not be clearly decided. To clarify the actual incidence of dural AVF and CVT and the relationship between them, larger cohort studies with long-term angiographic evaluation are required.
Infection
Infection is hypothesized to cause CVT by altering the coagulation cascade and inducing a hypercoagulable state in patients with an active infection12). Infection accounted for 8.2% of all the cases in the ISCVT series4). Cavernous and transverse sinus thrombosis cases are most frequently associated with infections such as sinusitis, otitis, and mastoiditis, with Staphylococcus aureus as the most frequently reported pathogen14). In our study, the incidence of infection was 13.9%, and in the 3 patients with a cavernous sinus thrombosis, infection was the cause.
Prothrombotic condition and hemorrhagic infarction
The probability of a hemorrhage might increase with coagulopathy, and patients with hypercoagulability are less likely to experience a bleeding diathesis7). In this study, the incidence of a hemorrhagic infarction was significantly higher in the patients with a prothrombotic condition. In arterial infarctions, a large-volume infarction, a delayed time of reperfusion and collateral flow failure are the factors associated with hemorrhagic transformation4,9). Similarly, the authors hypothesize that hypercoagulability leads to a more rapid thrombosis formation and venous sinus occlusion, which results in a more abrupt venous stasis and increased intracranial pressure, resulting in an increased probability of hemorrhagic transformation.
This issue has not been investigated previously, and this study has certain limitations. First, the specificity and sensitivity of the hypercoagulability laboratory values might be altered because confounding factors were neglected. Defining 1 or 2 positive findings of numerous hypercoagulability laboratory tests as a prothrombotic condition might be controversial. In addition, the sample size is limited, with 8 of the 36 patients having a prothrombotic condition. More tests and larger randomized trials are needed to sufficiently verify this hypothesis. Finally, this study was conducted retrospectively; the patient data extracted from the medical charts were initially recorded for clinical use rather than for research purposes. In spite of these limitations, however, our study contains unique information on the characteristics of CVT patients in a Korean sample and on the significance of the relationship between hemorrhagic infarction and prothrombotic condition.
CONCLUSION
In this study, CVT was more prevalent in men, and the peak age at diagnosis was in the sixth decade of life. The most common cause was a prothrombotic condition, followed by infection and post-operative change. This finding was comparable with reports from Europe or America, in which CVT was more common in younger women18). The low proportion of Korean women on oral contraceptives and the low birth rate in Korea might have influenced those results. A hemorrhagic infarction was more common in the prothrombotic group than in the non-prothrombotic group (p=0.016). Further studies with larger cohorts are required to evaluate the clinical characteristics of CVT patients in Korea and to establish appropriate therapeutic strategies.