Acute Spontaneous Spinal Subdural Hematoma with Vague Symptoms
Article information
Abstract
Spinal subdural hematoma is a rarely reported disease and spontaneous spinal subdural hematomas (SSDH) without underlying pathological changes are even rarer. The patients usually show typical symtoms such as back pain, quadriplegia, paraplegia or sensory change. But rarely, patients may show atypical symptoms such as hemiparesis and misdiagnosed to cerebrovascular accident. We recently experienced a case of SSDH, where the patient initially showed vague symptoms, such as the sudden onset of headache which we initially misdiagnosed as subarachnoid hemorrhage. In this case, the headache of patient improved but the neck pain persisted until hospital day 5. Therefre, we conducted the MRI of cervical spine and finally confirmed SSDH. The patient was managed conservatively and improved without recurrence. In this case report, we discuss the clinical features of SSDH with emphasis on the importance of an early diagnosis.
INTRODUCTION
Acute spontaneous spinal subdural hematoma (SSDH) is a rarely reported disease. The cause of SSDH may be spontaneous or iatrogenic. And many of patients are associated with underlying coagulopathy or receiving anticoagulant and antiplatelet agent11). Typical symptoms related with SDH are neck pain, radicular pain and myelopathy such as quadriplegia or quadriparesis3,4,7,9,11,12,13,14,15). These symptoms occur due to the cord compression by hematoma. It is known to be a neurosurgical emergency but some cases with spontaneous remission have also been reported4,11,14,15). And, SSDH may initially lead to misdiagnosis if the patient shows unusual manifestations11).
Here in, we report a case of SSDH with sudden onset headache with no other neurologic symptoms. The patient was initially misdiagnosed as non-aneurysmal subarachnoid hemorrhage.
CASE REPORT
A 66-year-old woman visited the emergency department with a sudden onset of severe headache. She had no underlying disease, no history of anticoagulant therapy, no hematological coagulopathy and no history of trauma. She only underwent a mastoidotomy due to chronic otitis media at our institute one week before admission. She was alert but had a severe, worsening headache of sudden onset and neck stiffness. No neurologic abnormalities were found in the cranial nerves and cerebellar system. According to her medical history and neurologic examination, we conducted a brain computed tomography (CT) under the impression of acute subarachnoid hemorrhage, but it was unremarkable. Next, we conducted spinal tapping and she showed positive on 3 tube test. We then performed an angiography CT and 4 vessel angiography. But, no definite intracranial aneurysms could be found. The tentative diagnosis of non-aneurysmal subarachnoid hemorrhage was made initially. We hospitalized the patient, continued the supportive care and conservative management. Until hospital day 5, the headache was improved but posterior neck pain and neck stiffness persisted. We performed a cervical spine magnetic resonance imaging (MRI) and found a large amount of subacute subdural hematoma on C7 to T4 level (Fig. 1). We continued the supportive care as the patient had no neurologic deficit but only pain and the symptoms were gradually improved. She was discharged on hospital day 15. A follow up MRI was performed after 4 months. The hematoma was nearly disappeared and the patient presented no residual symptoms (Fig. 2).
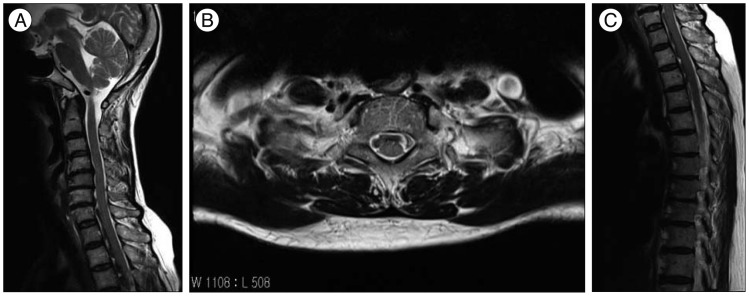
A and B : Sagittal and axial T2-weighted magnetic resonance image of the cervical spine demonstrating subdural hematoma on ventral side of the cord. C : Sagittal T2-weighted magnetic resonance image of the thoracic spine.
DISCUSSION
SSDH is an uncommon cause of spinal cord compression. And it is usually related with following trauma, lumbar puncture, anticoagulant therapy, underlying neoplasm, arteriovenous malformation or rarely, with acupuncture4,7,9,11,12). Spontaneous SSDH is a rarer entity, but the etiology remains still unclear4). In the spinal subdural space there are no major vessels and no bridging veins. One theory is that the hemorrhage originates within the more vascular subarachnoid space, possibly after sudden raised intra-abdominal or intra-thoracic pressure3). And others suggest that the subdural hematoma arises from ruptured small vessels on the inner surface of the dura10).
There has been some case reports and review of literatures dealing with diagnosis and treatment of the disease. The most common site of SSDH is in the thoracolumbar or lumbar segment11). Most of patients present with pain, quadriplegia, paraplegia, sensory change or cauda equina syndrome3,4,5,7,9,11,12,13,14,15). And, sometimes patients show unusual manifestations such as pure hemiparesis11). It is thus difficult to make the correct diagnosis at the very beginning if the patient has no history of trauma, related disease or treatment and do not show typical symptoms. It is often misdiagnosed as cerebrovascular accidents if the patient shows an unilateral involvement of motor or sensory disturbance11). There are reports that showed successful treatment of SSDH with conservative management4,5,7,8,9,11,13,14,15). However, in some cases, SSDH may need surgical treatment and besides, in some cases, neurologic deficit can persist3,4,6,7,10,12,15). Therefore, it is important that clinicians make an impression for the the disease and an early diagnosis is essential for preventing irreversible paralysis or other neurologic deficits5). But, like in this case, patients may show atypical symptoms and may be initially misdiagnosed. If the initial diagnostic work ups are unremarkable, clinicians should consider SSDH even when patients do not show typical symptoms corresponding to SSDH. Once the clinician suspect the diagnosis of SSDH, MRI is the preferred diagnostic method and SSDH appears as a space-occupying lesion, usually ventral, contained within the dura mater1,2).
CONCLUSION
In general, SSDH is a rare disease and known to be related to trauma. It is frequently associated with underlying coagulopathy in most patients or with those patients receiving anticoagulant or antiplatelet agent. Usual symptoms are neck pain, radicular pain and myelopathy. But, SSDH can cause various symptoms and the patient may have no related disease or previous trauma history like in our case. Moreover, delay of treatment due to misdiagnosis can lead the patient to have irreversible neurologic deficit. It is therefore very important for the clinicians to suspect the possibility of spontaneous SSDH even the patients do not have related disease or typical symptoms.
