The Effect of Postural Correction and Subsequent Balloon Inflation in Deformity Correction of Acute Osteoporotic Vertebral Fractures
Article information
Abstract
Objective
To determine deformity correction by postural correction and subsequent balloon inflation in acute vertebral compression fractures (OVCFs) and to examine the effect of bone mineral density on deformity correction.
Methods
A totol of 50 acute OVCFs received balloon kyphoplasty. Lateral radiographs were taken and analyzed at five different time points : 1) preoperative, 2) after placing the patient in prone hyperextended position, 3) after balloon inflation, 4) after deposition of the cement, and 5) postoperative. All fractures were analyzed for height restoration of anterior (Ha), middle (Hm) and posterior (Hp) vertebra as well as Cobb angle and Kyphotic angle. The bone mineral density (BMD) of lumbar spine was measured by dual-energy X-ray absorptiometry. According to the T-score, the patients were divided into two groups which were osteoporosis group and osteopenia group.
Results
Postoperative measurements of Ha, Hm and the Cobb angle demonstrated significant reduction of 4.62 mm, 3.66 mm and 5.34° compared with the preoperative measurements, respectively (each p<0.05). Postural correction significantly increased Ha by 5.51 mm, Hm by 4.35 mm and improved the Cobb angle by 8.32° (each p<0.05). Balloon inflation did not demonstrate a significant improvement of Ha, Hm or the Cobb angle compared with baseline prone hyperextended. Postural correction led to greater improvements of Ha, Hm and Cobb angle in osteoporosis group than osteopenia group (each p<0.05).
Conclusion
In acute OVCFs, the height restoration was mainly attributed to postural correction rather than deformity correction by balloon inflation. BMD affected deformity correction in the process of postural correction.
INTRODUCTION
Balloon kyphoplasty is a minimally invasive surgical treatment for osteoporotic vertebral compression fractures (OVCFs). Balloon inflation intends to restore vertebral height and correct kyphosis, creating a cavity into which the cement can be injected to stabilize the fracture and provide pain relief. Balloon kyphoplasty has shown good clinical outcomes as well as effective restoration of sagittal alignment15,18). There is a reduction of post-fracture kyphosis in up to 47% to 92% cases after kyphoplasty4,7,15,18). However, it has been demonstrated that many OVCFs are mobile and postural reduction can lead to clinically significant height restoration3,17). Therefore, the real efficacy of the kyphoplasty procedure can only be evaluated after the postural reduction in prone hyperextended position3,11,23).
Although balloon inflation provides a significant restoration of vertebral height postoperatively compared with preoperatively, whether it increases vertebral height after postural reduction remains controversial. Some studies11,19,23) claimed that the height restoration was attributed to dynamic fracture mobility as well as balloon inflation. While others argued that balloon inflation did not further increase vertebral height2), and even kyphoplasty achieved the same degree of height restoration and kyphosis reduction as vertebroplasty9). Moreover, balloon kyphoplasty was originally adapted for sub-acute or chronic OVCFs with delayed union or nonunion and now could also be adapted for acute OVCFs to improve function.
A previous study highlighted that significant factors affecting height restoration were the degree of the kyphotic deformity, the level, age of the fracture and the presence of an intravertebral vacuum cleft sign24). Most previous studies ignored the possible associations between deformity correction and bone mineral density (BMD).
The aim of the present study is to evaluate whether balloon inflation restores sagittal alignment after postural correction in acute OVCFs. This study also tests the hypothesis that the degree of deformity correction is related to BMD in the patients with OVCFs.
MATERIALS AND METHODS
Patients
This is a prospective radiology study of all consecutive balloon kyphoplasties performed in our unit over the previous year (February 2012 to February 2013). Fifty single-level OVCFs were treated by balloon kyphoplasty. Selection criteria for kyphoplasty were : 1) presence of OVCFs, 2) sufficient pain to impair activities of daily living, 3) absence of neurologic symptoms, 4) sufficient medical stability to tolerate general anesthesia, and 5) absence of contraindication. Patients were included only when their lumbar-spine BMD T-scores were lower than -1. Thirty-eight (77.8%) patients were women and twelve (22.2%) were men. Mean patient age was 71.6 years (range, 60-82 years). The fractures occurred between T10 and L3. These patients were operated within 4 weeks of sustaining the fractures. Fracture compression was severe in 6, moderate in 24, and mild in 20 OVCFs. Fracture severity was determined semiquantitatively according to Genant classification8), which was characterized as mild (20-25%), moderate (25-40%) or severe (>40%) vertebral compression fracture at any posterior, middle, or anterior point. The fracture was detected in preoperative standing anteroposterior and lateral radiographs. Further examinations were performed to provide an evidence of edema in the fractured vertebral body on T2-weighted images and to evaluate the phenomenon of intravertebral vacuum cleft by magnetic resonance imaging (MRI) scan in all patients.
Technique of kyphoplasty
In the operating room, patients were placed in prone position with the spine extended by chest and pelvic bolsters and under general anesthesia condition. Kyphoplasty was performed through a transpedicular approach by using two 11-gauge bone biopsy needles. Inflatable Bone Tamps (Shangdong Guanlong Medical Utensils Co., Ltd, Shangdong, China) were placed bilaterally into the vertebral body through working cannulas and inflated in the center of the vertebral body. Inflation continued until the balloon reached 300 psi (1 psi=6895 Pa) or the maximal balloon volume was reached. After the balloons were withdrawn, polymethylmethacrylate cement (Tianjin Synthetic Materials Research Institute, Tianjin, China) was injected into the fractured vertebral body and its volume was recorded. The cement was allowed to cure for 5 minutes until it had a tooth paste viscosity to lower the risk of cement extravasation. Simultaneous c-arm fluoroscopy was used for guiding the needle insertion and balloon inflation.
Assessment of vertebral body height and kyphosis
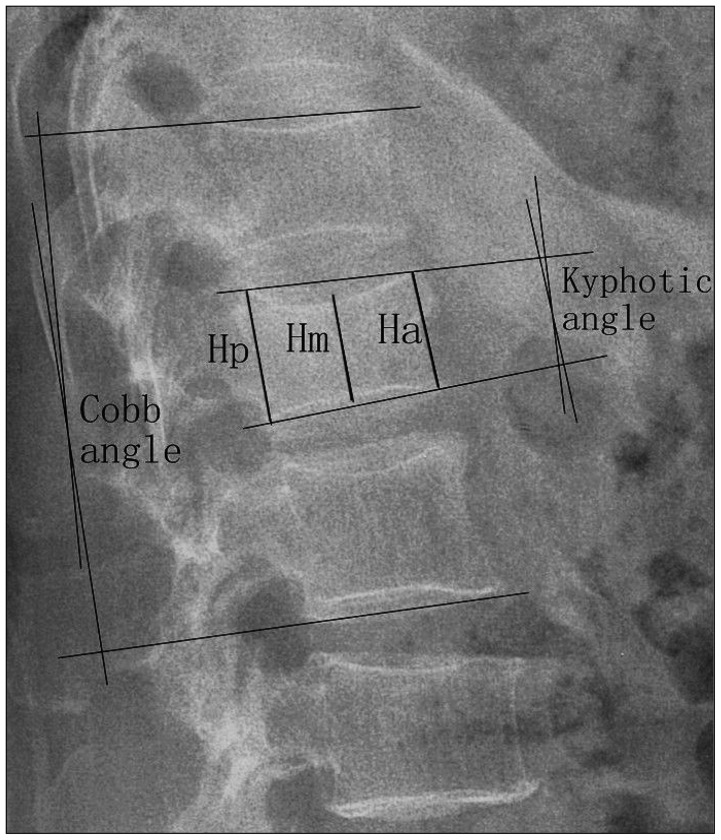
Lateral radiographs were taken and analyzed at five different time points : 1) preoperative (standing lateral X-ray), 2) after placing the patient in prone hyperextended position, 3) after bilateral balloon inflations, 4) after deposition of the cement, 5) postoperative (standing lateral X-ray). At each time point, we calculated vertebral height in the anterior (Ha), middle (Hm), and posterior (Hp) portions of the treated vertebra, Kyphotic angle and Cobb angle (Fig. 1). Ha was the distance between the most anterior-superior and anterior-inferior endplate margins. Hm was the distance between the midpoint of the two superior endplates and midpoint of the two inferior endplates in the middle part of vertebra. Hp was the distance between the most posterior-superior and posterior-inferior endplate margins. Kyphotic angle was the angle in degrees defined by the intersection of superior and inferior endplate of the fractured body. For determination of the Cobb angle, measurement was taken from the superior endplate of the vertebra one level above the treated vertebra to the inferior endplate of the vertebral body one level below the treated vertebra. Preoperative compression ratio was defined as the ratio of anterior height of fractured vertebra to average anterior height of the cranial and caudal vertebrae. Vertebral height and sagittal alignments were measured on Pictures Archiving and Communications System (INFINITT, Seoul, Korea). The blinded measurements were repeated 2 times at 2-week intervals. The precision error was calculated for each dimension Ha, Hm, Hp, Kyphotic angle, and Cobb angle, 15 randomly selected fractured and nonfractured osteoporotic vertebrae were measured. From these values, the standard deviation (SD) was obtained.
BMD measurement
The bone mineral density for spine lumbar was measured by dual-energy X-ray absorptiometry (DEXA, Lunar Radiation, Madison, WI, USA) and the results were expressed as T-scores. Osteopenia is defined as a BMD that is between 1 and 2.5 SDs below the average for the reference population. Osteoporosis is defined as a BMD that is 2.5 SDs or more below the young adult mean20). According to the T-score for lumbar-spine BMD, the patients were divided into two groups, which were osteoporosis group (27 cases) and osteopenia group (23 cases).
Statistics
Statistical analysis was performed with SPSS 16 software (SPSS Inc., Chicago, IL, USA). For numeric data, mean±SD were calculated. To test for precision in measurements, we used the intra-class correlation. Comparisons between different time points were performed using a paired sample t-test. Comparisons between different groups were performed using the independent sample t-test or chi-square test. Differences were considered as statistically significant with a p value of less than 0.05.
RESULTS
Precision
Precision errors expressed as SD were 2.2 mm, 2.7 mm, 2.3 mm, 2.8°, and 4.2° for Ha, Hm, Hp, Kyphotic angle and Cobb angle, respectively. The intra-class correlations were 0.93, 0.90, 0.96, 0.88, and 0.86 for the Ha, Hm, Hp, Kyphotic angle and Cobb angle, respectively.
Overall height reduction and sagittal realignment
The overall height reduction and sagittal realignment postoperatively compared with preoperatively was showed in Fig. 2 and 3. Ha and Hm improved significantly from 20.84±5.06 mm (range, 9.42-33.08 mm) to 25.46±4.62 mm (range, 14.58-33.80 mm), and from 17.79±4.51 mm (range, 8.10-24.81 mm) to 21.45±4.18 mm (range, 9.49-27.6 mm), respectively. Hp improved from 27.36±4.82 mm (range, 19.82-37.46 mm) to 29.93±4.24 mm (range, 19.88-42.6 mm) without significance. The Kyphotic angle was reduced significantly from 10.27±4.31° (range, 2.5-18.74°) before surgery to 6.43±3.53° (range, 0.88-12.30°) after surgery. The Cobb angle was reduced significantly from 12.98±6.89° (range, -5.68-24.24°) before surgery to 7.64±5.91° (range, -6.35-22.03°) after surgery.
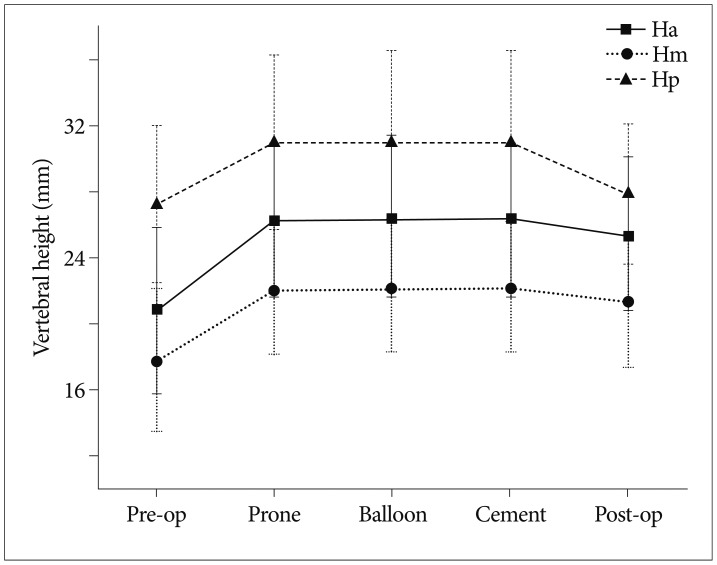
Vertebral height restoration during the kyphoplasty procedure. p<0.001 for prone vs. preoperative (Ha, Hm, Hp); postoperative vs. preoperative (Ha, Hm). p<0.01 for postoperative vs. cement (Ha, Hm, Hp). Ha : anterior vertebral height, Hm : middle vertebral height, Hp : posterior vertebral height.
Dynamic fracture mobility
Placement of patients in prone hyperextended position led to a significant restoration of vertebral height and segmental kyphosis (Fig. 2, 3). After placing the patient in prone hyperextended position, Ha improved by 5.51±2.64 mm, Hm by 4.35±2.73 mm, Hp by 3.79±3.22 mm, Kyphotic angle by 5.01±2.74°, and Cobb angle by 8.32±3.69° (each p<0.001).
Effect of kyphoplasty
The average balloon inflation pressure was 180 psi (range, 120-300 psi). The average volume of cement applied to the vertebra was 4.6 mL (range, 3-6 mL). Balloon inflation did not contribute to a significant vertebral height increase in anterior, middle or posterior portion after postural reduction (each p>0.05) (Fig. 2). In addition, no significant improvement was detected in Kyphotic angle or Cobb angle (each p>0.05) (Fig. 3). Subsequent placement of cement in the vertebra did not alter the degree of reduction by means of Ha, Hm, Hp, Kyphotic angle and Cobb angle (each p>0.05) (Fig. 2, 3). Moreover, patients lost reduction after cementing to post-operative films, with Ha losing 0.97±0.33 mm, Hm by 0.86±0.31 mm, Hp by 1.43±0.52 mm, Kyphotic angle by 1.51±0.44° and Cobb angle by 3.51±1.02° (each p<0.05).
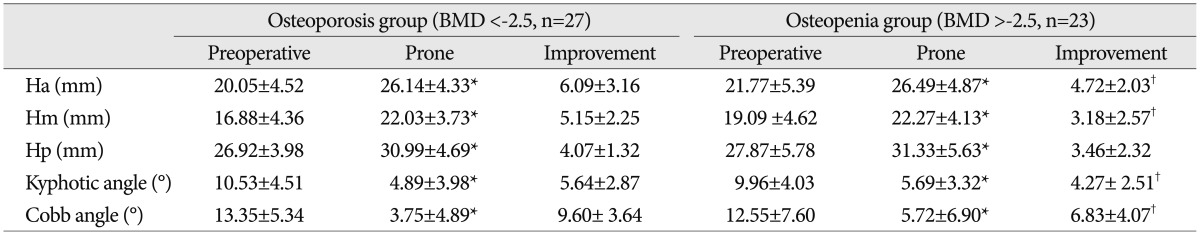
Effect of BMD
We evaluated the effect of postural correction on height restoration and sagittal realignment in the osteopenia and osteoporosis groups, respectively (Table 1). In both groups, postural correction improved Ha, Hm, Hp, Kyphotic angle and Cobb angle significantly (each p<0.05). Moreover, postural correction led to greater improvements of Ha, Hm, Kyphotic angle and Cobb angle in osteoporosis group compared with osteopenia group (each p<0.05). In contrast, balloon expansion did not significantly improve vertebral height and sagittal alignment in either group and no significant difference of improvement was noticed between the two groups. Preoperative compression ratio was 62±23% in osteoporosis group, which was more severe than 79±9% in osteopenia group (p<0.01). Intravertebral vacuum clefts occurred in 11 of 27 vertebrae in osteoporosis group and 8 of 23 vertebrae in osteopenia group (p>0.05).
DISCUSSION
Dynamic fracture mobility raises concern in OVCFs as it implies complete corticocancellous disruption and permits the vertebral height restoration after postural reduction3,17). As the injury of OVCFs produced is an anterior wedge fracture, postural reduction in prone hyperextended position can re-expand the compressed anterior column11). Intra-operative positioning with bolsters under the upper chest and the iliac crests could lead to clinically significant height restoration5,16,17,21). Voggenreiter23) reported that placement of the patient in this way produced a significant reduction of Cobb angle by 6.4°, Kyphotic angle by 3.7°, Ha by 19%, Hm by 16% and Hp by 16%. Cawley et al.2) put forward a technique which maintained the leverage created by pelvic extension as well as bolstering the chest and pelvis. Analysis of their data revealed an 8.3% increase in anterior vertebral height and a 4.9° reduction in Cobb angle. By using four small bolsters, we demonstrated improvements of 8.3° in Cobb angle, 5.0° in Kyphotic angle, 26.4% in Ha, 24.5% in Hm and 13.9% in Hp in our intra-operative postural correction. We suggested that placements of bolsters under the chest and pelvis provided a satisfactory spine extension and contributed to a significant deformity reduction.
Balloon kyphoplasty has the potential to relieve the fracture related pain and correct the segmental deformity. A few studies showed that balloon kyphoplasty was effective in deformity correction of OVCFs and attributed the height restoration to the balloon inflation12,15,22). Voggenreiter23) found that balloon inflation achieved a deformity correction with the Cobb angle reducing by 3.5° compared with baseline prone hyperextended, Ha improving by 19% and Hm by 18%, respectively. In his series, a majority of OVCFs (61.5%) were severe compression fractures. Kim et al.11) attempted to determine the efficacy of kyphoplasty after postural reduction in severe OVCFs and observed significant improvements of Ha by 13 mm and Hm by 9 mm, respectively. Thus, kyphoplasty could further achieve significant height restoration after the process of postural reduction in severe OVCFs.
The degree of the kyphotic deformity seems to be the most significant factor affecting height restoration12). Table 2 summarises the corrections achieved by postural correction and balloon inflation in various studies. Cawley et al.2) suggested that postural correction rather than balloon inflation led to a significant restoration of vertebral height which was in conflict with several other studies. In his study, the mild and moderate OVCFs were in the majority with preoperative compression ratio of 72%. We also found that the treated vertebra reached maximal restoration after intra-operative postural reduction and little height restoration was observed by subsequently using balloon kyphoplasty in mild or moderate OVCFs. In the current study, eighty-eight percent of these OVCFs were mild and moderate in fracture severity with preoperative compression ratio of 70%.
Fracture chronicity is a variable affecting postural versus balloon assisted reduction. The adaptation of balloon kyphoplasty is originally for patients who have the delayed union or nonunion vertebral fractures in sub-acute or chronic phases (more than 6-8 weeks after injury). As kyphoplasty rapidly reduces pain and improves function, disability, and quality of life, it is now in common used for the treatment of acute vertebral compression fractures1,6). Feltes et al.6) found that kyphoplasty failed to restore vertebral height in acute osteoporotic vertebral fractures. Our study also showed that dynamic fracture mobility rather than balloon inflation attributed to height restoration in acute OVCFs.
In the current study, we noticed that patients lost reduction after cementing to post-operative films. This phenomenon can be explained by two reasons : firstly, the soft bone of osteoporosis allows subsidence to occur once the up-right posture is resumed. Secondly, incomplete PMMA leads to the limited dynamic correction of the segmental deformity14). Thus, postural correction contributes to height restoration and sagittal realignment and cement augmentation contributes to height maintenance.
BMD correlated with the prevalence of vertebral fracture. In patients with normal BMD, a vertebral fracture was found in 14% and the percentage rose to 21% in patients with osteopenia and to 33% in patients with osteoporosis10). There were few studies of the relationship between BMD and restoration of the vertebral height, as well as segmental kyphosis. One study found out that BMD did not correlated with height restoration14). However, in our study, postural correction led to a greater improvement of vertebral height (Ha and Hm) and segmental kyphosis in vertebrae with lower BMD. A possible explanation was warranted : preoperative compression ratio affected the height restoration and kyphotic angle reduction14). As dynamic fracture mobility permitted compressed vertebra to restore vertebral height, anterior vertebral compression was greater in osteoporotic fractures and hence greater height restoration was permitted.
The current study has some limitations. First, the number of patients and the number of compression fractures are limited. Second, we did not evaluate the long-term maintenance of height loss as follow-up was not the primary intention of this study. It has been previously demonstrated that vertebral height remained stable for at least 2 years following treatment13).
CONCLUSION
In acute osteoporotic vertebral compression fractures, the height restoration was mainly attributed to postural correction rather than deformity correction by balloon inflation. The degree of the kyphotic deformity seemed to be an important factor affecting height restoration. BMD affected deformity correction in the process of postural correction.