The Surgical Treatment of Three Young Chronic Subdural Hematoma Patients with Different Causes
Article information
Abstract
Chronic subdural hematoma (CSDH), which rarely happens in the young, is thought to be a disease of the elderly. Whereas unspecific symptoms and insidious onset in juveniles and young adults, as a result of its relative low morbidity, CSDH is usually neglected even undertreated in the young. Through the three cases and review of the current literature on this subject, we tried to illustrate the clinical and etiopathological characteristics of this entity and find out the most appropriate treatment strategy. We report three young CSDH patients with different but similar symptoms. The present histories, tests and examinations revealed different predisposing factors accounting for the genesis of CSDH. Their preoperative symptoms were all resolved with burr hole and drainage operation. Juveniles and young adults suffering from CSDH differ from that of their elderly counterparts in their clinical and etiopathological characteristics. Although trauma is the most important risk factor in young and old CSDH patients, some other predisposing factors may exist. Burr hole and drainage surgery could resolve the problem most of the time. But further tests and examinations even specific management should be made in some cases.
INTRODUCTION
Chronic subdural hematoma (CSDH) is broadly thought to be a disease of the elderly and is well recognized and managed in the aged population. Whereas unspecific symptoms and insidious onset in juveniles and young adults, as a result of its relative low morbidity, CSDH is usually neglected even undertreated in that population group. Although trauma is the commonest risk factor in young and old CSDH patients, some other predisposing factors may exist1,2,3,15,18,22,26). A comprehensive understanding of the similarities and differences between the two groups in their clinical and etiopathological characteristics would undoubtedly be in favor of the diagnosis and management of this disease.
CASE REPORT
Case 1
A 17-year-old boy was admitted to our hospital with a global headache and dizziness accompanied by mild fever for 5 days. The neurological examination did not show any positive signs except for mild somnolence. CT-scan showed an isodense subdural hematoma in the left frontal and parietal region with an obvious compression of the left lateral ventricle and evident midline shift to the right (Fig. 1A). He preferred playing basketball in his spare time but denied recent head trauma. The blood count and coagulation panel revealed nothing remarkable. A burr hole and irrigation surgery was performed under local anaesthesia.
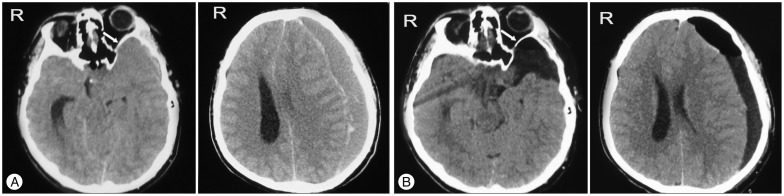
A : Preoperative CT shows an isodense subdural hematoma in the left frontal and parietal region with an obvious compression of the left lateral ventricle and evident midline shift to the right. B : Preoperative CT reveals an arachnoid cyst on the right sylvian region. Arrow shows the bony indentation and thinning of the peak of the left middle fossa.
CT images one day after operation showed a complete evacuation of the subdural hematoma and slight shift of the midline structures with the residual hematoma space occupied by low density fluid and air (Fig. 1B). However, the interesting finding in the postoperative CT was that an arachnoid cyst was located in the tip of the middle fossa. A retrospective analysis of the preoperative CT images displayed the bony indentation and thinning of the peak of the left middle fossa, which implied a pre-existed arachnoid cyst. Postoperative cerebral angiography did not reveal ateriovenous malformation or other vascular abnormalities. The previous symptoms were completely resolved after surgery and the patient was immediately engaged in daily life after discharge despite the remaining slight midline shift. Follow-up CT imaging taken 3 months after surgery showed no change of the volume of the arachnoid cyst and no new formation of CSDH.
Case 2
A 27-year-old male complained of intermittent distending headache for one month without head injury history. The headache was not deteriorated progressively, but with no evident remission. He then went to the local hospital 2 days before admission. The MRI (Fig. 2A) revealed a half-mooned high intensity effusion on T1 and T2 weighted imaging in the right hemisphere with compressed ipsilateral ventricle and midline shift, which implied a CSDH. Physical examination the day on admission was unremarkable. Coagulation panel and blood count of the patient showed no abnormal findings.
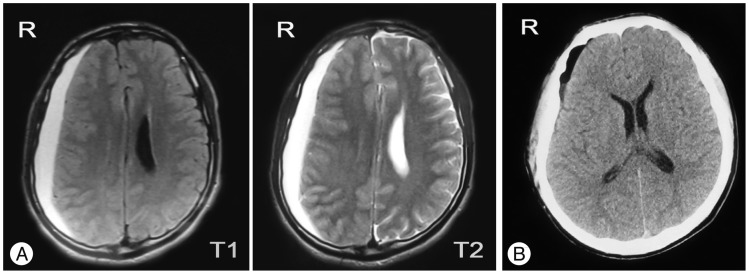
A : MRI shows a half-mooned high intensity effusion on T1 and T2 weighted imaging in the right hemisphere with compressed ipsilateral ventricle and midline shift. B : Postoperative CT illustrates a complete evacuation of the hematoma and restoration of the compressed brain tissue.
A burr hole and irrigation operation was conducted one day after admission. Postoperative CT one day after surgery showed complete evacuation of the hematoma and restoration of the compressed brain tissue (Fig. 2B). Considering complete resolution of the preoperative symptoms, the subdural catheter was withdrawn subsequently. A computed tomography angiography, which revealed nothing remarkable, was conducted to rule out any vascular anomaly of the brain and dura. Follow-up CT imaging taken 3 months after surgery showed no novel collection of CSDH.
Case 3
A 31-year-old female complained of a frontal and parietal hea-dache for 10 days with aggravation for 2 days following a mild head trauma one month previously. The headache was slightly aggravated with orthostatic position. The day before admission she vomited once and suffered right hemiparesis. CT showed an isodense subdural hematoma in the left frontal and parietal region, with compressed ipsilateral ventricle and midline shift (Fig. 3A).
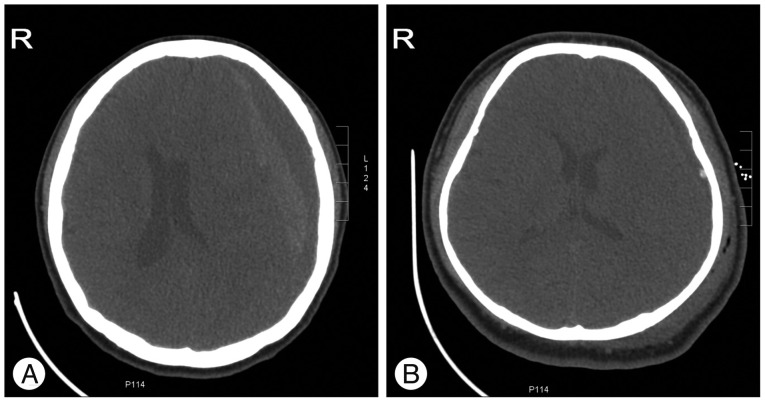
A : CT shows an isodense subdural hematoma in the left frontal and parietal region with compressed ipsilateral ventricle and midline shift. B : Postoperative CT illustrates a subtotal evacuation of the subdural hematoma and restoration of the midline structures with the residual hematoma cavity replaced by low density fluid and air.
Without any hemostatic disorder and surgery contraindication, the patient underwent a burr hole and irrigation operation. Her intracranial pressure was not so high as was seen in the patients alike. Postoperative CT (Fig. 3B) one day after operation showed a subtotal evacuation of the subdural hematoma and restoration of the midline structures with the residual hematoma cavity replaced by low density fluid and air. With an apparent relief of her preoperative symptoms she was discharged 8 days after admission. She was readmitted 15 days later, complaining of severe headache. Her headache was slightly aggravated with orthostatic position. CT images the day on admission showed a small amount of subdural hematoma in the left frontal region without compression of the ventricles or shift of the midline structures. Headache derived from intracranial hypotension was suspected.
She underwent a lumbar puncture with the opening pressure below 50 mmH2O in the lateral decubitus position. A jugular venous compression maneuver was used to rule out the possibility of obstruction in cerebral spinal fluid (CSF) circulation. Biochemical examination and microorganism culture of her CSF were unremarkable. With no operation indication, she received intravenous saline hydration, bed rest and oral analgesics. As her headache resolved gradually, she refused to undergo MRI or cisternography. She was discharged with a slight intermittent headache. Outpatient follow-up revealed complete resolution of her headache. She reengaged in daily work and study.
DISCUSSION
CSDH is generally thought to be a disease of the elderly as it is well recognized and managed in the aged population. There are many hypotheses pertaining to the genesis of CSDH. Bridging vein tearing after a minor head injury and hemostatic disorder caused by blood effusion in the subdural cavity is widely accepted as the pathogenetic mechanism in the formation of CSDH in aged people. However, it could not explain all the cases, especially those young patients without traumatic history and cerebral atrophy.
Coagulopathy, arteriovenous malformation and anuerysm have previously been reported to predispose to CSDH1,15,16). Besides, arachnoid cyst, especially located at the middle fossa11,23), has long been regarded as a promotive factor2,3,18,22,26). The speculated mechanism may be that tearing of the outer wall of an arachnoid cyst causes subdural and/or intracystic hemorrhage by breaking the bridging veins, unsupported blood vessels around the cyst wall and leptomeningeal vessels in the base of the cyst3,18). As was illustrated by case 1, preferring playing basketball, though without definite head injury history, might have led to tearing of the wall of the arachnoid cyst and its ambient blood vessels. Then, a certain amount of cerebral spinal fluid (CSF) and/or blood leaking into the subdural space induced the formation of the outer membrane under the dura mater. The fenestrated neovessels in the subdural outer membrane and the osmotic and hemostatic alterations induced by the subdural degradation products give rise to the gradual collection of subdural hematoma.
Intracranial hypotension (IH) has also been reported to be associated with CSDH14,19,20,28,30). IH is characterized as orthostatic headache, low CSF opening pressure at lumbar puncture, subdural collection, diffuse meningeal enhancement with gadolinium and caudal displacement of the brain on MRI imaging5,10,13,17). CSF leakage caused by trauma, invasive craniocerebral and lumbar procedures or some inherited diseases as Marfan's syndrome, Enlers-Danlos syndrome, etc. is the commonest pathological basis of IH7,21,24,27). As was illustrated by case 3, head injury might have led to the intracranial hypotension and they collectively or respectively caused the CSDH. Also, there are reports of CSDH derived from IH with no evident reason9,29).
Besides all reasons above, there are also some reports of CSDH in the young with no traced origin4,6). Just as case 2 illustrated, no traumatic history and predisposing factor could be sought out. Anyway, early realization of the common symptoms and timely diagnosis and management would undoubtedly benefit the CSDH patients.
With different etiopathological mechanisms, the treatment strategies of CSDH differ greatly between the juvenile and young adult group and the elderly. As some of the young CSDH patients may predispose with one or more risk factors, e.g. arachnoid cyst, arterioveneous malformation, coagulopathy, aneurysm or intracranial hypotension, the preferable choices would be taking account of CSDH and the promotive factors at the same time. In consideration of arachnoid cyst as a relatively convinced risk factor in the genesis of CSDH, we should inform patients with arachnoid cyst and their families of the possibility of complication with CSDH and advise care to avoid head injury in daily life18). That does not mean that we should recommend surgical treatment for arachnoid cysts to patients without clinical manifestation to prevent CSDH. Surgery aiming at arachnoid cyst may also lead to CSDH formation12,18). In fact, as was illustrated by case 1 and other cases18), pure burr hole evacuation and drainage could yield satisfactory result most of the time.
While, the treatment of intracranial hypotension related CSDH consists of burr hole evacuation of the hematoma, sufficient bed rest, intravenous hydration, analgesics or epidural blood patch if CSF leakage is identified8,19,25,28). Spontaneous IH usually resolves spontaneously in a certain period of time with conservative treatment including bed rest and intravenous hydration. So, the complicating CSDH may be treated with only burr hole and drainage surgery as case 3 showed. If remission could not be achieved with conservative management, radioisotope cisternography or CT myelography is recommended. Epidural blood patch is implemented when CSF leakage is located19,28,30).
CONCLUSION
Juveniles and young adults suffering from CSDH differ from that of their elderly counterparts in their clinical and pathological characteristics. Although trauma is the most common risk factor in young and old CSDH patients, some other predisposing factors may exist. Burr hole and drainage surgery can resolve the problem most of the time. But further tests and examinations even specific management should be made in some cases.