Brown-Séquard Syndrome Caused by a Cervical Synovial Cyst
Article information
Abstract
Synovial cysts are recognized as an uncommon cause of radicular and myelopathic symptoms. They are most frequently found in the lumbar region. The cervical spine or cervicothoracic junction is a rare location for a degenerative intraspinal synovial cyst as compared with the lumbar spine. At given cervical spinal levels, synovial cysts probably share clinical features with disc herniation and stenosis. However, the pathogenesis of synovial cysts remains still controversial. Here, we report a rare case of a synovial cyst in the lower cervical spine presented as Brown-Séquard syndrome and include a brief review of the literature. To the best of our knowledge, no previous report has been issued in the English literature on a synovial cyst presenting with Brown-Séquard syndrome. Neurologic function recovered completely after complete removal of the cyst and expansive laminoplasty.
INTRODUCTION
Synovial or ganglion cysts arising from the capsules of facet joints or from yellow ligament are uncommon disease entity3,4,10). These cysts are usually encountered in the lumbar spine, but can occur in the cervical or cervicothoracic spine5,8). Although rare, a synovial cyst or ganglion cyst can form in the cervical spinal canal, usually near an articular facet or in a yellow ligament. The majority of these cysts are asymptomatic, but occasionally, they can induce neurologic symptoms7). Moreover, Brown-Séquard syndrome caused by a synovial cyst is very rare and no previous report of a synovial cyst presenting with Brown-Séquard syndrome has been previously issued in the English literature. We experienced a rare case of Brown-Séquard syndrome caused by a cervical synovial cyst, and here, report this unique case with a review of the literature.
CASE REPORT
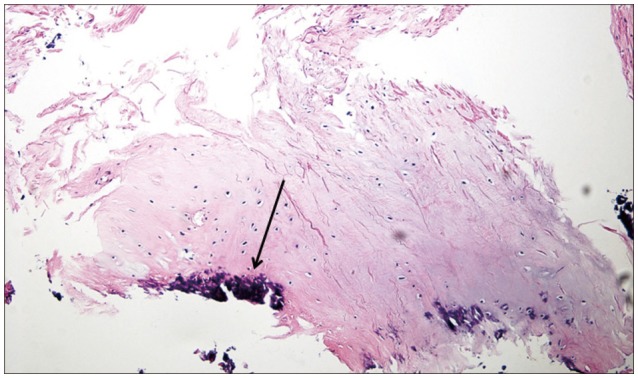
A 64-year-old man, who had experienced sudden weakness and numbness in the left lower extremity for 4 weeks, visited our emergency department for evaluation and treatment. Over several days, his gait disturbance gradually worsened and the numbness had extended to the left upper chest region. There was no evident traumatic episode before admission. A physical examination conducted at presentation revealed gait disturbance with spasticity. He was able to stand by himself, but needed a crutch for walking. A neurological examination showed motor weakness of left lower extremity (Grade IV). In addition, sensory disturbances of vibration and positional sensation were present on the left side below the T4 dermatome. Impaired perception of pain and temperature stimuli were also noted on the right side below the T4 dermatome. Brown-Séquard syndrome of the cervicothoracic or thoracic spine was then suspected. Plain radiographs of the cervical spine showed multiple degenerative changes. Accordingly, magnetic resonance imaging (MRI) of the whole spine was performed. Sagittal T2-weighted MR images revealed a left-sided cystic extradural lesion at the C7-T1 junction (Fig. 1A), and axial images showed that the extradural cystic lesion markedly compressed the spinal cord (Fig. 1B). The lesion appeared homogenously isointense on T1 weighted images and exhibited heterogeneous high signal intensity on T2 weighted images. Under a presumptive diagnosis of a cystic lesion in the lower cervical spine, emergent surgery was performed. Because there were additional osteophytes causing cord compression at C4-5 and C5-6, modified expansive laminoplasty of C5-6 and a laminectomy of C7 followed by complete removal of the extradural cyst were performed. The lesion was homogeneous, bright yellow in color, firm in consistency, and slightly adherent to dura mater, and contained a small amount of serous fluid. Pathological examination showed the cyst to be composed of fibrous connective tissue and to have a distinct synovial cell lining with focal calcification (Fig. 2). The diagnosis was confirmed as a synovial cyst. Immediately after surgery, motor power and impaired sensation were improved. At his 6-month follow-up, he was able to walk without any assistance and returned to work. At his 8-month follow-up, no recurrence of symptoms, except for mild numbness, was evident.
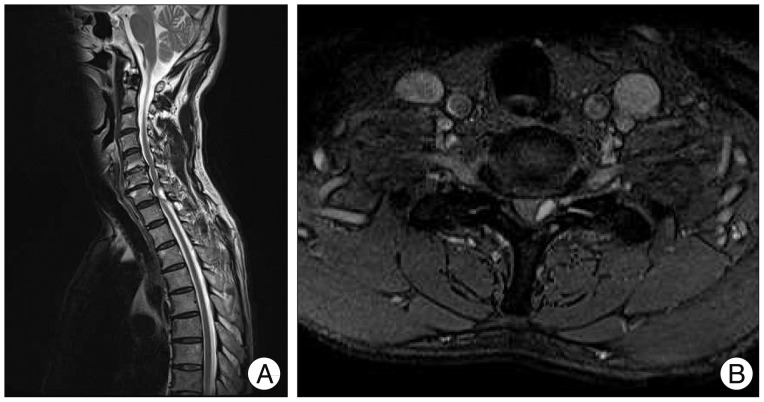
T2-weighted sagittal (A) and axial magnetic resonance (B) images show an intraspinal cystic mass lesion compressing the spinal cord at the C7-T1 level.
DISCUSSION
Extradural juxtafacet cysts are uncommon intraspinal pathologies. These cysts are often located at lumbar facet joints, and less frequently, at cervical facet joints1,12). These "juxtafacet cysts" encompass synovial and ganglion cysts. Synovial cysts and ganglion cysts have similar clinical and radiological features but are histopathologically differentiable. Although several hypotheses have been proposed to explain the development of epidural juxtafacet cysts, their pathogenesis remains unclear. Synovial cysts are believed to develop from degenerative diseases of joints and to represent herniations of joint synovium, but no joint communication may be evident by imaging. On the other hand, ganglion cysts are believed to originate from mucinous degeneration within periarticular dense fibrous connective tissue2,7). Generally, synovial cysts contain clear, serous fluid, whereas ganglion cysts contain gelatinous, viscous fluid. However, this distinction is not clear, and their differential diagnosis based on contents is difficult. Furthermore, distinguishing between these two entities does not appear to be meaningful from clinical perspective because the treatments afforded are identical. For this reason, Kao et al.9) grouped synovial and ganglion cysts together and proposed the term "juxtafacet cyst". Other pathologies that should be included in the differential diagnosis include all types of space-occupying lesions that may occur in the spinal canal.
Both MRI and CT are useful for the diagnosis of degenerative intraspinal cysts. MRI is most helpful at demonstrating free fluid in a cyst, whereas CT can reveal gas contents in a cyst, the presence of which strongly suggests that the cyst communicates with a facet joint or a degenerated disc space. The clinical progression of patients with a degenerative juxtafacet cyst is variable. Synovial cysts of the spine are usually asymptomatic unless acute hemorrhage occurs after trauma or a significant increase in size causes nerve root or cord compression. In cases without neurological deterioration, close observation could be recommended because spontaneous reduction or resolution of a cyst have been reported during conservative treatment6,11). In addition, a less invasive treatment, that is, intra-articular local anesthetic and steroid injection, has been proposed when pain is the exclusive symptom. However, this management is accompanied by risks of neurologic complications in the cervical region. Accordingly, the foundational treatment for degenerative intraspinal cyst is surgical excision. Most authors have performed laminectomy and cyst excision in the cervical spine. Our patient also had associated Brown-Séquard syndrome and combined spondylotic spinal stenosis, and thus, spinal cord decompression by open door laminoplasty was indicated in addition to complete cyst removal.
CONCLUSION
Although rare, a synovial cyst in the lower cervical spine should be taken into consideration as a possible cause of Brown-Séquard syndrome in patients with a degenerated cervical spine.