Symptomatic Epidural Pneumorrhachis : A Rare Entity
Article information
Abstract
Pneumorrhachis, which involves the entrapment of air or gas within the spinal canal, is a rare clinical entity, and the pathogenesis and etiologies of this uncommon entity are various and can present a diagnostic challenge. Usually, pneumorrhachis represents an asymptomatic epiphenomenon but it can produce symptoms associated with its underlying pathology. Here, we report a rare case of symptomatic epidural pneumorrhachis accompanying pneumothorax. Possible pathogenic mechanisms are discussed and a review of the literature is included.
INTRODUCTION
Pneumorrhachis is defined as the presence of air within the intradural or extradural compartments of the spinal canal4,5). Air within the epidural space is also referred to as epidural emphysema or epidural pneumorrhachis, and has been described in association with spontaneous pneumomediastinum or pneumothorax, degenerative disc disease, epidural abscess, synovial cysts, or after epidural analgesia. On the other hand, symptomatic epidural pneumorrhachis is an extremely rare manifestation after severe trauma3,6,9,10). Pneumorrhachisis usually asymptomatic, does not tend to migrate, and is reabsorbed spontaneously5). However, rarely, it is symptomatic and associated with discomfort and pain or even neurological deficits8,12). Here, we report a rare case of symptomatic, extensive traumatic epidural pneumorrhachis accompanying pneumothorax and include a review of the literature.
CASE REPORT
A 50-year-old man was admitted to our emergency department with blunt neck and thoracic trauma caused by a falling tree. On arrival, he was alert and his Glasgow Coma Scale point was 15. His vital signs were stable and electrocardiography, blood cell count, and serum biochemistry were unremarkable. He had full strength in his bilateral upper and lower extremities and he was able to move without limitation. However, he complained of intolerable, diffuse pain in his neck and back with reduced sensation to light touch in all extremities. There was decreased temperature and pinprick in his upper and lower extrimities bilaterally, below the C5 level. Brain computed tomography (CT) revealed no evidence of any abnormality. However, thoracic CT revealed a basal lung contusion and left pneumothorax with multiple fractures of third, fourth, fifth, and sixth ribs, and cervicothoracic spine CT showed extensive pneumorrhachis extending from C4 to T8 and compressing the spinal cord excessively (Fig. 1). Nonetheless, there was no evidence of fracture or subluxation within the spine. A thoracostomy tube was promptly inserted and he was transferred to our intensive care unit for close observation. Conservative treatment including bed rest, O2 inhalation, and medication for pain relief was administered for 7 days, when he was stable and able to tolerate an oral diet. On the 14th day after admission, CT of the cervicothoracic spine was normal and demonstrated complete resolution of the air within the spinal canal with no further complication (Fig. 2). The patient was discharged of 18 days after admission. At the time of discharge, his neurologic examination was unremarkable, and he had full strength in all extremities and an intact sensation to light touch without pain.
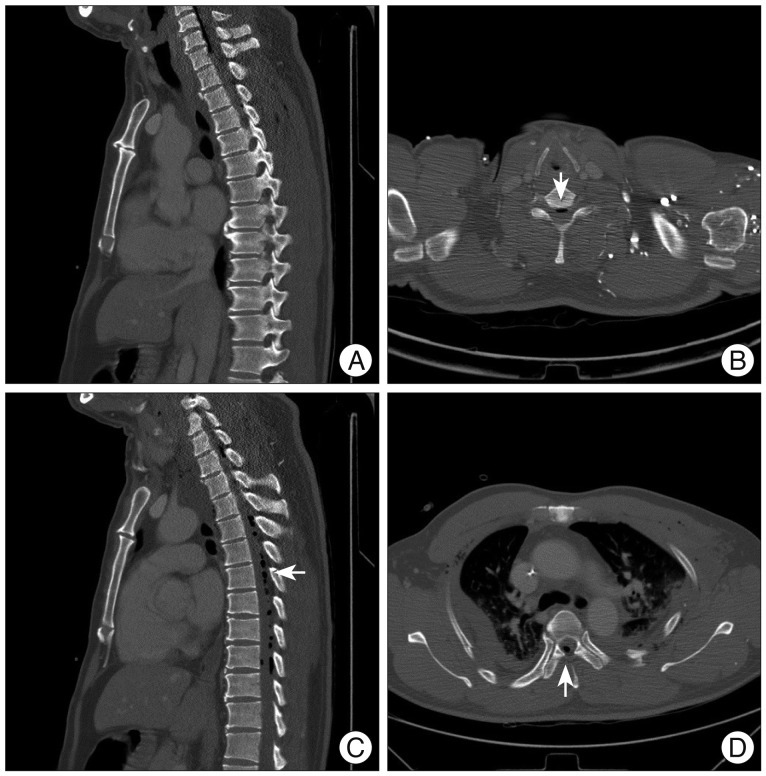
Computed tomography (CT) scans of the patient. A and B : Sagittal and axial cervicothoracic CT images show air (arrows) within the anterior cervical epidural space. C and D : Sagittal and axial cervicothoracic CT images show air (arrows) within the posterior thoracic epidural space.
DISCUSSION
Pneumorrhachisis is defined as the presence of air within the epidural or subarachnoid space. The condition is rare, and thus, few reports are available1). Although difficult, even by CT, the epidural and subarachnoid types of pneumorrhachis should be differentiated, because the clinical consequences of traumatic epidural pneumorrhachis and traumatic subarachnoid pneumorrhachis differ. According to a previous report, the former is usually innocuous and self-limited, whereas the latter may be complicated by tension pneumocephalus and meningitis7). The causes of epidural pneumorrhachis have been broadly classified as iatrogenic, spontaneous, or traumatic. Iatrogenic causes are the most common, usually after epidural injection or epidural analgesia. Non-traumatic causes have been described following spontaneous or non-trauma related pneumomediastinum or pneumothorax3,10). In a review of the English literature, Goh and Yeo7) analyzed 13 cases of traumatic epidural pneumorrhachis, seven of which were secondary to traumatic pneumothorax or pneumomediastinum, as in our case. The pathway through which air spreads from the posterior mediastinum space into the epidural space is uncertain. One possible mechanism for pneumorrhachis is that air present in the posterior mediastinum and pressurized by pneumothorax or pneumomediastinum, dissects along fascial planes from the posterior mediastinum, through the neural foramina, into the epidural space2). Traumatic epidural pneumorrhachis is usually benign and resolves spontaneously when the underlying cause is treated. Hence, the management of traumatic epidural emphysema is based on targeting the underlying etiology. In patients with epidural pneumorrhachis secondary to traumatic pneumothorax showing persistent air leak, treatment of the pneumothorax by tube thoracostomy or occasionally surgery will result in resolution of the epidural air11). However, patients with epidural air secondary to more sinister underlying causes, such as, a dural-enteric fistula, require urgent intervention to prevent significant morbidity or even mortality8). The present report concerns a patient with traumatic epidural pneumorrhachis secondary to pneumothorax in the absence of pneumomediastinum, who was treated conservatively, and achieved a complete, uneventful recovery. Although traumatic pneumorrhachis is usually asymptomatic and does not require special treatment because the driving force of pneumothorax or pneumomediastinum can only push small volumes of air into the epidural space, its presence itself indicates severe trauma that requires careful monitoring.
CONCLUSION
We describe a unique case of symptomatic epidural pneumorrhachis secondary to traumatic pneumothorax. Although rare and usually innocuous, treating neurosurgeons should always be wary of the more sinister and potentially life-threatening causes of traumatic epidural pneumorrhachis.
