Disseminated Tuberculosis of Central Nervous System : Spinal Intramedullary and Intracranial Tuberculomas
Article information
Abstract
As a cause of spinal cord compression, intramedullary spinal tuberculoma with central nervous system (CNS) involvement is rare. Aurthors report a 66-year-old female presented with multiple CNS tuberculomas including spinal intramedullary tuberculoma manifesting paraparesis and urinary dysfunction. We review the clinical menifestation and experiences of previous reported literature.
INTRODUCTION
There are many causes of spinal cord compression such as hematoma, infections. However, case of intramedullary tuberculoma, compressing the spinal cord, with disseminated intracranial lesion is very rare3). Although tuberculosis remains a major health problem in developing countries, tuberculoma involving the central nervous system (CNS) is still uncommon compared with the involvement of other systems3,4). It has been estimated that approximately 10% of all patients with tuberculosis have CNS involvement1). Intramedullary tuberculomas are rare and constitute only 0.2 to 0.5% of all CNS tuberculomas3). Most cases of intramedullary tuberculomas are subacute with progressive spinal cord compression symptoms1-5). Given the rarity of spinal intramedullary tuberculoma, there is no standardized treatment protocol for this condition6,9). We report a rare case that the patient had previously received therapy for pulmonary tuberculosis and subsequently developed intramedullary spinal tuberculoma concurrently with asymptomatic multiple intracranial tuberculomas.
CASE REPORT
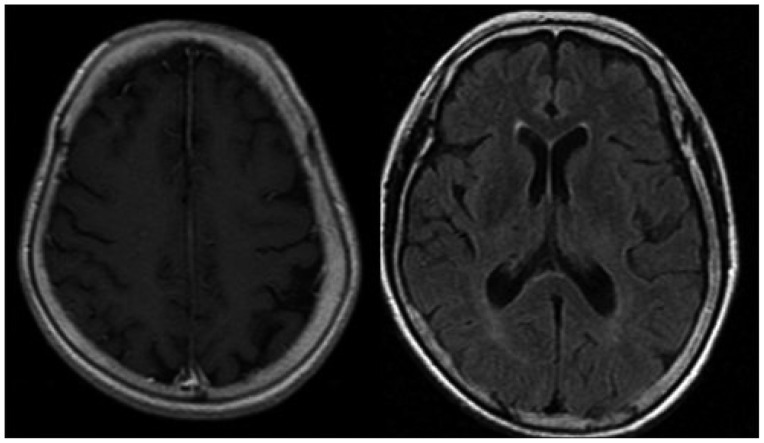
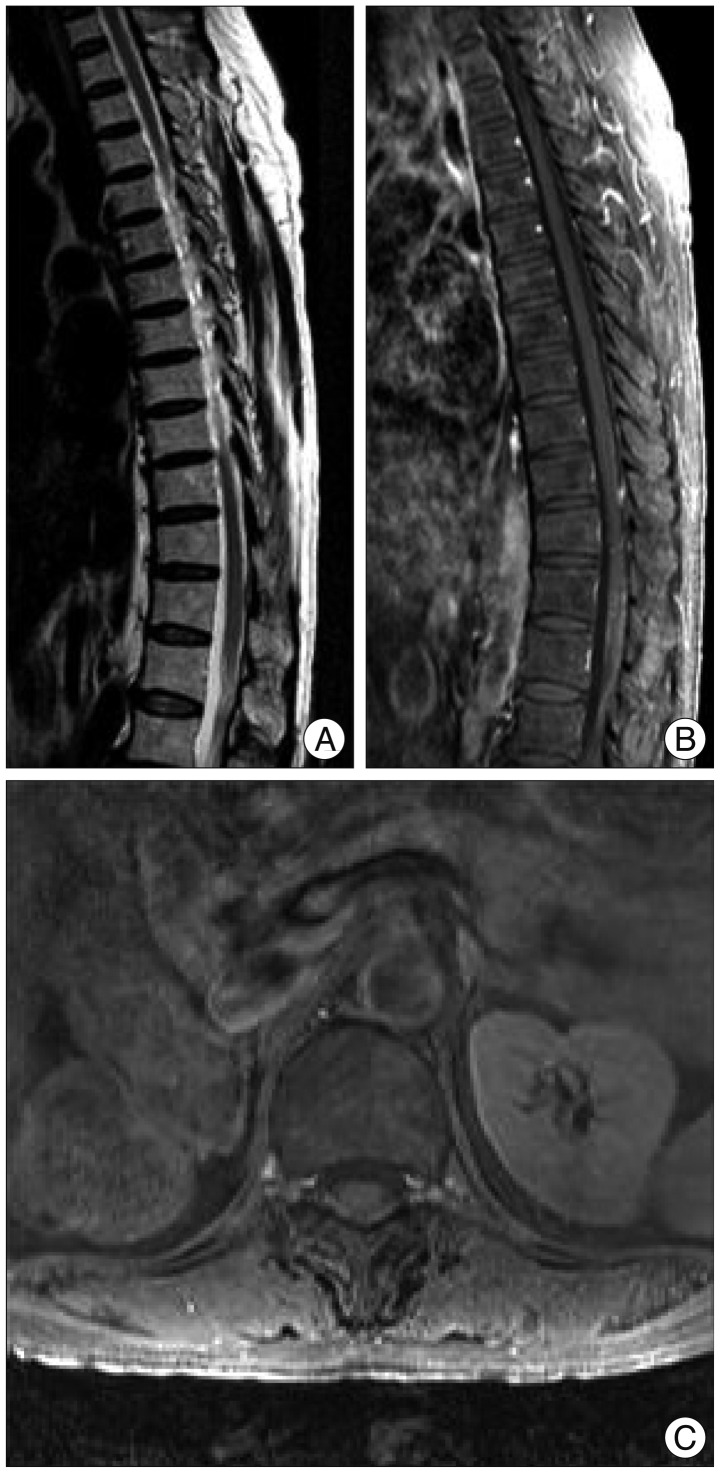
A 66-year-old woman was admitted with bilateral lower extremity weakness and voiding difficulty for 2 weeks. Paraparesis with muscle power of the right lower extremity was grade 2/5 and the left lower extremity was grade 1/5, impaired sensations below the L1 level and decreased strength in the anal sphincter tone. Lower extremity reflexes including knee jerk and ankle jerk were absent. No evident upper extremity motor or sensory deficit was seen. Magnetic resonance imaging (MRI) of the thoracolumbar showed about 1.2×1×4 cm sized intramedullary enhancing lesion with central necrosis on conus medullaris at T12-L1 levels. The lesions were isointense on T1-weighted images and hyperintense on T2-weighted images, which were associated with diffuse edema of spinal cord on T7-T11 level. We presumed that this abscess might be closely related with tuberculous abscess. However, in laboratory, sputum, Cerebrospinal fluid (CSF) cultures and Acid-Fast bacilli stains were negative. A cerebrospinal fluid study showed glucose levels 55 mg/dL, protein 100 mg/dL, and 50 lymphocytes/mm3. Initial C-reactive protein (CRP) was 24. On review of her previous medical history, she was treated for pulmonary tuberculosis, diagnosed six months earlier. And 1 month ago, pus was found in the right kidney due to her flank pain, which was proved to be tuberculosis after drainage. She was also treated by rifampin, ethambutol, pyrazinamide at other hospital. Chest simple X-ray showed that features of bilateral pulmonary tuberculosis with multiple patchy consolidations. We took brain MRI in order to differentiate the brain lesion. MRI findings of brain showed multiple abscesses at the cerebrum and cerebellum. Results of a Tb INF-r were positive. Initially, we planed surgical treatment, however, we postponed the surgery due to her poor general condition and refusal of her family. Under the diagnosis of multiple CNS tuberculomas on spinal cord and brain, the anti-tuberculous drugs were started with rifampicin 600 mg, isoniazid 300 mg, pyrizinamide 1000 mg, ethambutol 800 mg. At 2 month later after medication, the muscle power in the both lower limbs had improved to grade 4/5, and voiding was also recovered. After 3 months of medical treatment, she could walk by herself. Follow up lab of CRP was reduced from 24 to 0.9 at 2 month later. Normalization of CRP was seen at 3 months of medication for tberculosis. After 6 months, the MRI of spine showed the markedly decreased size of intramedullary nodule at T12-L1 levels, which meaned improvement of tuberculous abscess, though perilesional edema of conus medullaris still remain. And MRI of brain showed that marked improvement of multiple nodular enhancing lesions at both frontoparietal lobe, right thalamus and both cerebellar hemisphere. Finally, we concluded these lesions were due to tuberculosis though we did not have the pathologic confirmation.
DISCUSSION
Tuberculosis is a chronic bacterial infection of mycobacterium tuberculosis, and characterized by the formation of granuloma in infected tissues and cell-mediated hypersensitivity1,4).
Spinal intramedullary tuberculomas are extremely rare, seen in only 2 of 100000 cases of tuberculosis and 2 of 1000 cases of tuberculous CNS disease1). Intramedullary tuberculomas tend to occur predominantly in young people of developing countries1,5). According to Jena et al.2), tuberculomas of the spinal cord are seen in childhood or early adolescence rather than in later life. Intraspinal tuberculoma is almost always secondary to tuberculous involvement elsewhere in the body, most commonly pulmonary tuberculosis, as our patient7,8). The review of MacDonnell et al.3) reported the most common location of intramedullary tuberculoma is thoracic spinal cord, 72% of all case, which is similar to current case. The higher incidence involving the dorsolumbar area is explained on the basis of the regional blood flow to the spinal cord, the thoracic cord receiving about 45% of the entire supply to the cord as against 34% for the cervical cord9,10).
The clinical presentation of intramedullary tuberculomas is similar with clinical feature of subacute spinal cord compression, such as appropriate motor and sensory findings depending on the level of the lesion3,9,10). MacDonnell et al.3) also reported lower extremity weakness, back pain, bowel or bladder dysfunction, paresthesia as a clinical presentation, which is similar with our case.
Tuberculomas of the spinal medulla should be considered in the differential diagnosis of subacute spinal cord compression, particularly in patients with evidence of extraneural tuberculosis disease4,9,10). Intramedullary tuberculoma may be difficult to differentiate from space-occupying lesions such as primary and metastatic spinal tumors and other chronic granulomatous disease such as sarcoidosis, brucellosis, histiocytosis5).
The MRI used to be the diagnostic tool of choice in the evaluation of intramedullary tuberculosis1,5,6,8). The MRI characteristics of intramedullary tuberculomas have been described by Jena et al.2). The tuberculous lesion appears isointense on T1-weighted MRI images (T1WI) with slight or no expansion of the cord. On T2-weighted MRl images (T2WI) it appears isointense to hyperintense, sometimes with central high signals1,2,4). The MRI picture varies with the stage of the tuberculoma formation2,8). In the early phase, there is great inflammatory reaction with an abundance of the giant cells and a poor collagenous capsule with variable surrounding edema. At this stage the tuberculomas seem to be isointense on both T1WI and T2WI and enhancing homogeneously on contrast. Later, the tuberculoma capsule becomes richer in collagen and the surrounding inflammatory reaction may decrease or disappear, resulting in an isointense lesion on T1WI and isointense to hyperintense on T2WI, and ring enhancement with hypointense center on Gd-DTPA MR scan1,2,6,8,10). With the development of caseation, the center becomes bright and gives an appearance of "target sign"7,10). In current case, MRI finding was similar with literature, the lesions were isointense on T1-weighted images and hyperintense on T2-weighted images and enhancing lesion with central necrosis5,6).
Additionally helpful but nondiagnostic laboratory values include an elevated leukocyte count, an elevated sedimentation rate, and an elevated CSF protein with a predominance of mononuclear cells8). In current case, CSF analysis showed non-specific finding, which might be related with previous anti-tuberculosis medication. But CRP was dramatically reduced after medication.
Simultaneous occurrence of intracranial and intramedullary tuberculomas is rare8-10). Our patient had also simultaneous occurrence of intracranial and intramedullary tuberculoma. Muthukumar et al.6) reported a 14-year-old girl who presented with progressive paraparesis in whom imaging revealed intramedullary tuberculoma with multiple intracranial tuberculomas. In this case, the intracranial lesions were incidentally discovered as our case. However, Yen et al.10), the patients were symptomatic for both intracranial and intramedullary lesions.
The choice of treatment modality and regimen is an important consideration5,8,9). Antituberculous agents are widely used and important in the treatment of intramedullary tuberculoma5,7,8,10). The response to antituberculous therapy clearly suggested tuberculous as a etiology7,8). As general principle in the treatment of CNS tuberculosis, drugs that penetrate the CNS such as particularly isoniazid, rifampin, ethambutol and pyrazinamide should be used8). There are no controlled studies detailing the specific combination and duration of antituberculous chemothrapy for intramedullary spinal tuberculomas3,6). The ideal treatment of intramedullary tuberculoma remains controversial7,8). Both surgical and medical treatments may show good results in different series7). Many authors have recommended medical treatment of intramedullary tuberculomas with good results rather than surgical treatment2,10). Surgery is generally indicated when 1) there is no response to chemotherapy, 2) the diagnosis is in doubt, and 3) there are large lesions with rapid deterioration in neurological function6,9). In our case, patients presented with paraplegia with classical imaging features of intramedullary tuberculoma with pulmonary and extrapulmonary tuberculosis, which were improved with chemotherapy. We tried to obtain the tissue, however, we could not perform the biopsy or culture from the brain and spinal cord lesion. Because patient and her family refused the procedure. This may be the shortage of our case. Rao8) and Jena et al.2) reported 6 patients with presumed radiological diagnosis of intramedullary tuberculoma who responded well to chemotherapy. This report may support treatment modality procedure which we choose in current case. Additionally, if there is any space occupying lesion on spinal cord, we should consider the possibility of tuberculomas, expecially in case of extraneural tuberculosis.
The intramedullary tuberculoma, although a rare entity, must be considered in the differential diagnosis of spinal cord compression in patients with a history of tuberculosis, a recent exposure to tuberculosis, a positive Mantoux test, an immunocompromised state, immigration from a developing country, or the pyrexial onset of symptoms1,4-6).
CONCLUSION
We reported the rare case of disseminated intramedullary and intracranial tuberculoma, which was treated successfully with medical treatment and review the previous literature.
It is important that we must consider the tuberculosis as a one of the spinal cord compressing etiology especially in case of extra neural tuberculosis.
As our patients, antituberculous therapy is successful and remains the mainstay of treatment, however when faced with a progressing neurological deficit, the neurosurgeon may need to consider surgical treatment.