Primary Eosinophilic Granuloma of Adult Cervical Spine Presenting as a Radiculomyelopathy
Article information
Abstract
We report a case of 29-year-old man diagnosed as a primary eosinophilic granuloma (EG) lesion of the seventh cervical vertebra. He had paresthesia on both arms, and grasping weakness for 10 days. Cervical magnetic resonance image (MRI) showed an enhancing mass with ventral epidural bulging and cord compression on the seventh cervical vertebra. Additionally, we performed spine series MRI, bone scan and positive emission tomography for confirmation of other bone lesions. These studies showed no other pathological lesions. He underwent anterior cervical corpectomy of the seventh cervical vertebra and plate fixation with iliac bone graft. After surgical management, neurological symptoms were much improved. Histopathologic evaluation confirmed the diagnosis of EG. There was no evidence of tumor recurrence at 12 months postoperative cervical MRI follow-up. We reported symptomatic primary EG of cervical spine successfully treated with surgical resection.
INTRODUCTION
Eosinophilic granuloma (EG) is one of Langerhans cell histiocytosis (LCH). LCH is a rare disease, with the incidence of 1 : 1500000 per year2,10). LCH was first named as histiocytosis X, and it includes three clinical entities, which are "Eosinophilic granuloma", a solitary osseous lesion; "Hand-Schuller-Christian disease", an eosinophilic granuloma with a triad of exophthalmos, lytic bone lesions (often in the skull), and diabetes insipidus (from pituitary stalk infiltration); and "Letter-Siwe disease," a malignant form of dissemination7,11,12). These three entities show very different presentations and outcomes, but have one thing in common, which is characterized by accumulation of the pathologic Langerhans cell10).
The most common site of EG is the skull, vertebra occupied only 7%15). In particular, the incidence of primary cervical spine is only 0.02%6). The most affected age of EG is younger than 15 years old2,10,16,18). Clinical feature of EG is mild, because EG is a self-limited disease2,3,5,7). Most cervical EG showed mild neck pain without neurological deficit2,10).
This case is primary EG of adult cervical spine with progressive neurological deficit. To the best our acknowledgement, it is the first primary reported EG presenting a radiculomyelopathy in Korea. We report a case of symptomatic primary of cervical spine excellently treated with surgical resection.
CASE REPORT
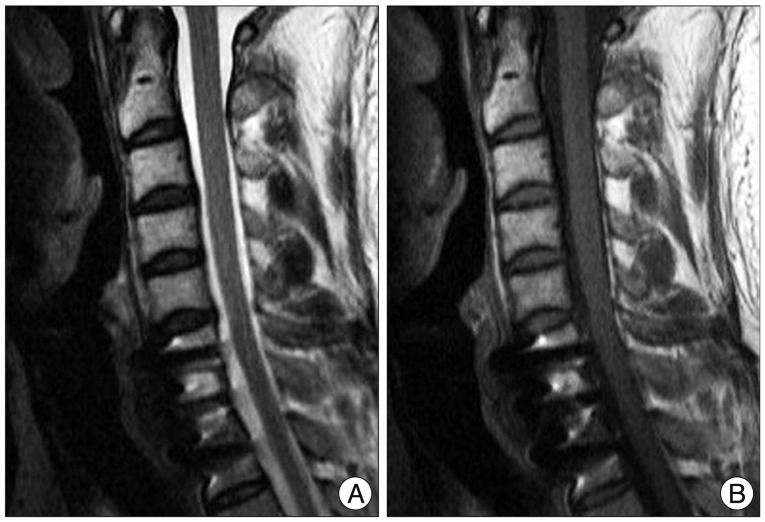
A 29-year-old man had paresthesia on both arms and grasping weakness for 10 days. His cervical MRI showed diffuse marrow infiltration with pathologic fracture producing symmetrical collapse of the C7 vertebral body. In addition, epidural extension produced ventral cord compression without cord signal change (Fig. 1). On physical examination, he had mild weakness of grasping and elbow extension power on both arms (Grade IV). Laboratory tests were all within normal limits. 3D cervical CT scan revealed symmetrical collapse of C7 vertebral body and no involvement of posterior column (Fig. 1). Our first impression was tuberculous (Tb) spondylitis; as such, we did anti-Tb medication and Tb-related laboratory tests. However, his grasping power of both hands was worsened (Grade IV→III). Therefore, we performed C7 corpectomy and anterior plate fixation C6-T1 and iliac bone graft (Fig. 2). In the operative field, disc spaces above and below the level of lesion were not involved. After surgical management, motor weakness was improved (Grade III→IV) and paresthesia on both arms also got better. Pathological evaluation confirmed the diagnosis of eosinophilic granuloma. He was immobilized after surgery in a rigid cervical brace for 3 months. In the following outpatient clinic, positron emission tomography CT was conducted additionally, but no other lesions were found. Twelve months follow-up cervical MRI showed no recurrence (Fig. 3) and his neurological deficits were fully recovered.

Preoperative radiographic images show tumorous condition. MRI showed collapse of C7 vertebral body and extension to paravertebral soft tissue and epidural space without invasion to adjacent disc spaces. In addition, epidural extension produced cord compression without definite cord signal change. Computed tomography scan and simple radiograph revealed severe bony destruction and sparing of the posterior column. A : T1 weighted sagittal MRI scan. B : T2 weighted sagittal MRI scan. C : T1-weighted gadolinium-enhanced axial MRI scan. D : Simple lateral radiographs at presentation. E : Coronal CT scan. F : Axial CT scan.

POD 1 radiographic images show C7 corpectomy state. A : Simple lateral radiograph. B : Cervical sagittal CT scan. C : Cervical coronal CT scan.
DISCUSSION
EG is the most common form (79% of all LCH bone lesions) among the three entities of LCH12). In the skeletal involvement of EG, skull is the most frequently involved site, followed by the pelvis, spine, mandible and ribs5). In the spinal involvement, thoracic vertebrae are the most often involved spine (54%); then, followed by the lumbar (35%), and cervical vertebrae (11%)2,4,17). Islinger et al.8) reported that in the retrospective review of 541 patients with LCH, spinal EG percentage was 3% in the adult group and was predominantly thoracic lesion. Howarth et al.6) also reported that the involvement of the cervical spine was present in only 0.02% of the 342 bone lesions. The frequent involving site of the vertebra is vertebral body, and posterior column is sparing commonly15).
The gender distribution (male to female) is 2-5 : 11,2,7). EG can present at any age but mostly occur in children or young adolescents. Most affected age of cervical EG is younger than 15 years old2,10,16,18).
Most common presenting symptom is neck pain and restricted range of motion or torticollis because the growth of EG is slow2,10). If the symptoms are relatively light, as many authors stated, close observation with frequent neurological examination can be chosen as the first proper treatment after histopathological diagnosis, confirmed by open biopsy or needle biopsy2,3,10,23). Jiang et al.10) strongly recommended using CT guided-needle biopsy for the confirmative diagnostic method. For patients with mild neurological symptoms, most of the authors stated that cervical immobilization is sufficient2,7,10,22,23).
In our case, primary EG located in cervical spine, and it showed progressive neurological deficits. This phenomenon is very rare in EG and it needs surgical management. Surgery should be performed for neurological deficits or severe mechanical pain2,9,15,20,21). As stated above, most of the reported cases underwent non-surgical treatment (close observation, immobilization) also have good results. There are several authors that stated that solitary osseous EG is a self-limiting disorder2,3,5,7). However, our patient showed progressive weakness in both arms, and therefore, we performed decompressive corpectomy and fusion surgery with iliac bone graft. Aggressive pattern of EG as our case is a rare phenomenon2,7,10). At 1 year follow-up, he has been in good condition with no evidence of recurrence.
Radiation therapy can be one of the treatment methods. In the study by Jiang et al.10), the local radiotherapy could obtain remarkable bony reconstruction and spine realignment. Richter and D'Angio14) also suggested low dose local radiotherapy for widespread involvement or incurable spinal LCH and several other researchers have also approved its effect, and its side effects appear to be small. However, Bertram et al.2) commented that radiotherapy should not be used as a first-choice treatment, especially in children. To the concerns regarding the destruction of the growth potential of the endochondral plates and secondary malignancy or radiation injury to the spinal cord, they recommend that the child cases should avoid radiotherapy if possible2).
Chemotherapy to treat LCH can help for multiple bone lesions or multi-system disease (Hand-Schuller-Christian disease or Letterer-Siwe disease)7). Some studies demonstrated the safety and effectiveness of chemotherapy13,19). However, in solitary cases as our patient, many authors do not recommend chemotherapy for initial management2,7,10).
CONCLUSION
We report a case of adult EG on C7 vertebral body that was successfully treated with surgical procedure. There are many diseases that showed vertebral destructive mass, but EG also should be considered as a potential disease. Although cervical EG showed somewhat a self-limiting process, there were several reported cases that showed neurological defects, as our case. In such cases, surgical intervention can make a successful result.
Acknowledgements
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A1014361).