Hyperperfusion Syndrome after Carotid Stent-Supported Angioplasty in Patients with Autonomic Dysfunction
Article information
Abstract
Cerebral hyperperfusion syndrome (CHS) is a rare, serious complication of carotid revascularization either after carotid endarterectomy or carotid stent placement. Although extensive effort has been devoted to reducing the incidence of CHS, little is known about the prevention. Postprocedural hypertension is very rare due to autoregulation of carotid baroreceptors but may occur if presented with autonomic dysfunction. We present two cases of CHS after cerebral revascularization that presented autonomic dysfunction.
INTRODUCTION
Cerebral hyperperfusion syndrome (CHS) typically occurs after carotid endarterectomy or carotid stent-supported angioplasty (CSA). The clinical features are characterized by ipsilateral headaches, vomiting, seizures, confusion, focal neurological deficits, parenchymal hemorrhage, and subarachnoid hemorrhage3,12). Risk factors for CHS associated with post-revascularization are severe ipsilateral stenosis, old age, severe contralateral disease, poor collateral flow, and hypertension, which have also been confirmed in patients with post-CSA1,6). Post-interventional hypotension is more likely to occur rather than hypertension due to parasympathetic hyperactivity by the baroreceptor reflex2). However, such as in patients with autonomic dysfunction, parasympathetic hyperactivity by the baroreceptor reflex is lower than normal. Therefore, it can lead to increased cerebral blood flow, which may be influential in causing CHS. Recently, noninvasive, well-validated clinical tests of autonomic function are available and are in relatively wide use. These comprise an evaluation of sudomotor, cardiovagal, and adrenergic functions.
As of now, there is yet to be a recommended test for assessing autonomic function before CSA. After the experience of two cases with CHS that presented autonomic dysfunction and post-procedural hypertension, we review the literature and report our cases.
CASE REPORT
Case 1
A 78-year-old male patient visited our hospital due to transient dysarthria and left-sided weakness which persisted for 5 years. He also had hypertension and diabetes mellitus. On arrival at the hospital, his National Institutes of Health Stroke Scale score was 2 with dysarthria and left-sided weakness (MRC grade IV). Brain magnetic resonance (MR) images showed no signs of acute cerebral infarction but brain MR angiography showed high grade stenosis of the proximal right internal carotid artery (ICA). Cerebral angiography performed one month later showed 80% stenosis of the symptomatic right ICA origin (Fig. 1A) and 55% stenosis of the left ICA origin. CSA was performed on the right side. An intravenous bolus of 5000 IU of heparin was administered. An anticholinergic drug (atropine) was administered before CSA to prevent hyper-parasympathetic function by the baroreceptor-reflex. The CSA procedure was performed in a standard protocol, including the following steps : placement of a 7.2 mm Emboshield NAV6 protection device (Abbott Vascular, Santa Clara, CA, USA), present angioplasty by 7×40 mm Sterling Monorail angioplasty balloon (Boston Scientific Corporation, Maple Grove, MN, USA), and 7-10 mm×40 mm RX Acculink® stent placement (Abbott Vascular, Santa Clara, CA, USA). Blood pressure was monitored and controlled pre- and post-procedurally. The morphological result improved with mild residual stenosis after dilation (Fig. 1B). Approximately 10 minutes after the intervention, the patient suddenly showed anosognosia and tried to sit up, developed left-sided weakness (MRC grade III/III), deviation of eye ball position to the right side, and became irritable. The patient had to be restrained because of constant movement, causing his blood pressure to rise up to 197/115 mm Hg. Despite using antihypertensive agents, his blood pressure did not fall below 150/100 mm Hg. In the intensive care unit, calcium channel block was maintained and blood pressure remained stable at 110/75 mm Hg.
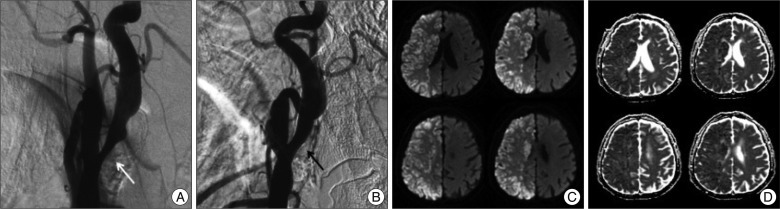
A 78-year-old male patient's cerebral angiography and brain MRI. Conventional angiography before carotid artery stenting reveals severe stenosis of the right internal carotid artery (white arrow) (A). Successful angioplasty with stenting was done in the right internal carotid artery (black arrow) (B). On a 24-hour follow-up diffusion weighted MRI (C), newly developed restricted diffusion lesions in the right middle cerebral artery and anterior cerebral artery territory. The apparent diffusion coefficient in the lesions amounts to a much higher value than that of normal parenchymal tissue, suggesting vasogenic edema (D).
On a 24-hour follow-up MRI, newly developed restricted diffusion lesions were found in the right ICA (middle and anterior cerebral arteries) territory. The apparent diffusion coefficient in the lesions amounted to a much higher value than that of normal parenchymal tissue, suggesting vasogenic edema (Fig. 1C, D).
Assessment of the autonomic function test was performed because the patient had a history of diabetes mellitus. In cold pressor test, blood pressure increased by systolic 31 mm Hg and diastolic 22 mm Hg, showing a normal reaction4). During the deep-breathing test, the difference between the maximal and minimal heart rate during six successive breaths was less than 10 beats/min indicated abnormal function5). The 30/15 ratio was calculated as the ratio of the R-R interval at beat 30 after standing to that at beat 15 (ratio=1.02 as a borderline response). During Valsalva-maneuver testing, the Valsalva ratio for this patient was 1.10 and defined as an abnormal autonomic response (Table 1)11).
Case 2
A 75-year-old male patient had presented with dysarthria and left-side weakness, which resolved within 24 h. He had a history of hypertension, diabetes mellitus. The MRI of the brain showed a few tiny foci of infarcts in the left subcortical watershed distribution (Fig. 2A). The MRA showed a high-grade stenosis of the proximal left ICA with no stenosis of the right ICA. A carotid stenting procedure was carried out 4 days later post-presentation with patient already on aspirin and clopidogrel. Angiogram showed a critical stenosis at the left cervical ICA origin (Fig. 2B). An anticholinergic drug (atropine) was administered before CSA and under full systemic heparinization, a catheter was placed in the left common carotid artery. A Transend EX SOFT TIP microcatheter (Boston Scientific Corporation, Global Park, Heredia, Costarica) with micro-guidewire were navigated past the stenosis; then an exchange wire was used to position a 6×40 mm Sterling Monorail angioplasty balloon (Boston Scientific Corporation, Maple Grove, MN, USA) across the stenosis and angioplasty was carried out (Fig. 2C). An excellent result was achieved with the neurological baseline. His postoperative blood pressure was 144/91 mm Hg and maintained continuously at 160/90 mm Hg. After using antihypertensive agents, his blood pressure was kept normal range. Heparin was stopped and 24 hours later he developed headache. A CT scan was obtained, which showed multiple small subarachnoid hemorrhages within the right hemisphere. The MRI showed additionally blood in the left temporal lobes (Fig. 2D). This was treated conservatively with temporary cessation of the antiplatelet agents and strict monitoring of the blood pressure.
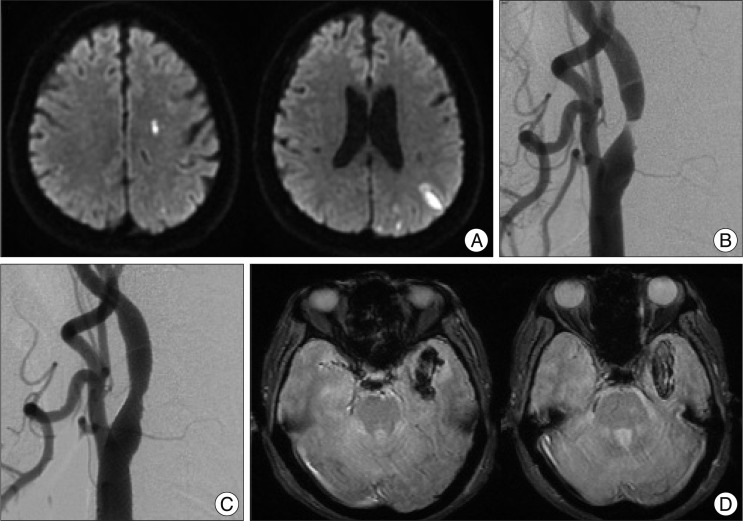
A 75-year-old male patient's brain MRI and cerebral angiography. Diffusion weighted MRI before the intervention reveals a few tiny foci of infarcts in the left subcortical watershed distribution (A). Cerebral angiogram shows a critical stenosis at the left cervical ICA origin before (B) and after the intervention (C). The gradient echo sequence MRI after the intervention shows additionally blood in the left temporal lobes (D). ICA : internal carotid artery.
Assessment of the autonomic function test was performed. In cold pressor test, blood pressure increased by 63/29 mm Hg, showing a normal reaction. During the deep-breathing test, the difference between the maximal and minimal heart rate was 14 beats/min indicated abnormal function. The 30/15 ratio was calculated 1.02 as a borderline response. During Valsalva-maneuver testing, the Valsalva ratio for this patient was 1.19 and defined as an abnormal autonomic response (Table 1)11).
DISCUSSION
The incidence of CHS after intervention has not been extensively studied. Meyers et al.7) reported that five (6.6%) of 76 patients with carotid artery stenosis developed CHS after CSA. Ogasawara et al.8) reported one of 30 patients with CHS. CHS is not a common complication. However, considering it is a serious complication and patients have minimal to no neurological deficits, attention should be given to the prevention of CHS. Studies investigating the risk factors for CHS after CSA have generally identified factors like severe ipsilateral stenosis, old age, severe contralateral disease, poor collateral flow, and hypertension1,6).
CHS may be due to the failure of normal cerebral autoregulation and secondary to long-standing changes in perfusion pressure. Maximal dilation of cerebral arterioles for long periods of time causes a loss of cerebral blood flow autoregulation. Increased cerebral blood flow, which cannot be controlled by autoregulatory mechanisms, leads to transudation of fluid into the pericapillary astrocytes and interstitium, and results in vasogenic white matter edema or hemorrhage10). Stimulation of carotid baroreceptors with a balloon or carotid artery stent may play an important role in the prevention of CHS. This is because carotid baroreceptor stimulation induces transient or prolonged bradycardia and hypotension2). For this reason, some studies recommended pre-management with the parasympathetic blocking agent atropine for preventing hemodynamic instability7). However, nervous system disorders that are often accompanied by autonomic dysfunction such as central nervous system disorders (multiple system atrophy, Parkinson disease, Huntington's disease, leprosy, HIV infection, and Fabry's disease) and peripheral nervous system disorders involve decreased baroreceptor reflex9,13). Decreased baroreceptor reflex may increase risk of post-intervention hypertension, so the autonomic dysfunction patient may be required consideration of the atropine use seriously.
Since the autonomic nervous system (ANS) is divided into the sympathetic and parasympathetic nervous systems, there are separate test batteries that have been developed for each division to assess those ANS functions11). Through these autonomic function tests, the damaged autonomic nerves can be identified and treatments can be applied.
In the present cases, the patients had diabetes mellitus. In autonomic function tests of both cases, the sympathetic nervous function was spared, which demonstrated that Cold pressor test was within normal range, but parasympathetic function was impaired. Such HR variation with respiration and Valsalva ratio did not reach the normal range (Table 1). Parasympathetic stimulation may have been low due to baroreceptor dysfunction during the balloon stent procedure, and the atropine used before the procedure may have been influential in causing hypertension after the procedure. In the case 1, the sudden increase in cerebral blood flow right hemisphere may have induced cerebral edema and neurologic deficit, and the patient's blood pressure may have continued to increase in the process of restraining his movement. In the case 2, post procedural high blood pressure may influence the left temporal lobe hemorrhage formation and induced headache. In these two cases, we underwent CHS with autonomic dysfunction that might be related to chronic diabetes mellitus. However, it is ideal to perform autonomic function test immediately before carotid stent insertion, there is the major limitation of this case report that autonomic function test was conducted after an unexpected occurrence of CHS.
CONCLUSION
As previously mentioned, CSA is performed on patients with minimal to no symptoms. Therefore, complications following the procedure are inevitably a big burden on doctors. Through careful analysis of risk factors associated with hyperperfusion syndrome along with autonomic tests that can be performed during hospitalization, post-procedural blood pressure can be predicted for a better prognosis and treatment for the patient.
