INTRODUCTION
Intracranial epidermoid cysts represent approximately 1% of all brain tumors and 7% of cerebellopontine angle (CPA) tumors, and generally regarded as slow growing brain tumors8). Intracranial squamous cell carcinoma is a rare complication of epidermoid cysts9,11,15,17). The clinical and radiological course of malignant transformation is more aggressive than epidermoid cysts, and their prognosis remains quite poor9,11,15). Treatment of such malignancies can be problematic, particularly if there is extensive brainstem involvement. We report a case of the CPA epidermoid tumor that transformed into a squamous cell carcinoma. The imaging and clinical features of this case focus attention on the efficacy of radiosurgery in the management of this unusual malignancy.
CASE REPORT
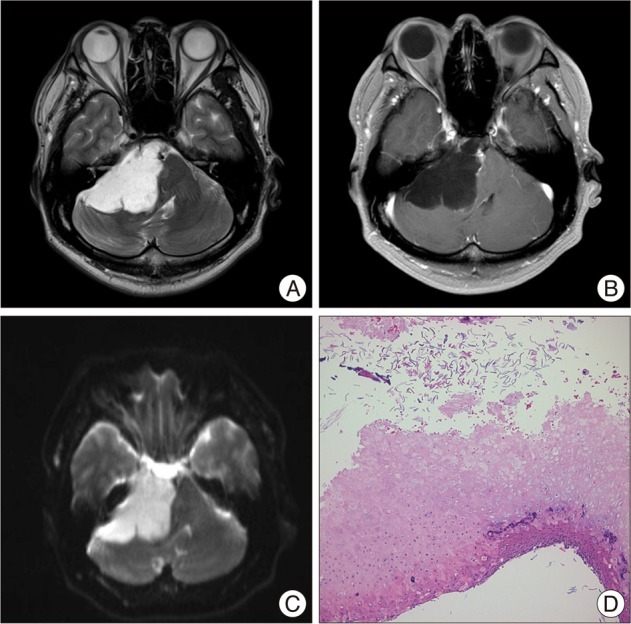
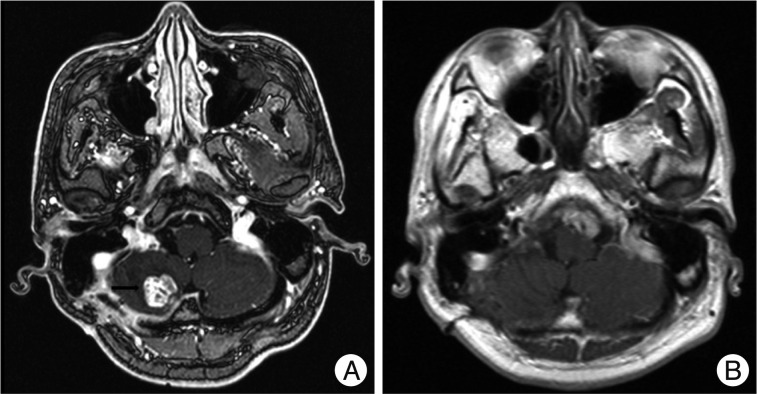
A 43-year-old man visited our clinics in February of 2009 due to the weakness of the right facial expression (House-Brackmann grade III). T2-weighted magnetic resonance image (MRI) showed a high signal intensity (SI) in the CPA (Fig. 1A). A T1-weighted gadolinium enhanced MRI showed a nonenhancing tumor in the right CPA, sized 58Г—38 mm (Fig. 1B). Diffusion-weighted (DW) MRI revealed a high signal intensity lesion in the right CPA (Fig. 1C). A right retrosigmoid suboccipital craniotomy was performed and the epidermoid tumor was resected. The capsule of the tumor adherent to the brainstem and the low cranial nerves was not able to be removed. Cranial nerves V through XI were identified and preserved. Histopathological findings showed keratin debris and squamous epithelium, consistent with an epidermoid cyst (Fig. 1D). In July 2009, follow-up brain MRI showed focal enhanced mass on the right cerebellar hemisphere, there is outside operation field (Fig. 2A). Because the patient refused reoperation, he underwent gamma knife radiosurgery (GKRS) for treatment of the small enhanced tumor on right cerebellar hemisphere in July of 2009 due to the small enhanced tumor which is highly probable malignant transformation. The tumor was covered with a 50% iso-dose gradient and the dose delivered to the tumor margin was 15 Gy; the maximum dose was 25 Gy. Annual radiological surveillance showed no change in residual tumor. In January 2011, follow-up contrast-enhanced axial T1-weighted image shows that there is no enhanced tumor (Fig. 2B). In April 2011, he presented again with facial numbness on the left side and swallowing difficulty. MRI showed a large tumor in the left CPA. T2-weighted MRI showed an iso SI in the CPA (Fig. 3A). Contrast-enhanced T1-weighted images showed strong enhancement of the nodular lesion sized 30Г—15 mm (Fig. 3B, C). These MRI findings were suggestive of the malignant transformation of epidermoid cyst or the benign meningioma. A left retrosigmoid suboccipital approach was done. However, the tumor could not be removed totally due to the highly adherent to the pons, cerebellum, and lower cranial nerves. The immunohistochemistry showed pan-cytokeratin, thereby proving an epithelial cell origin. These histopathological and immunohistochemical features were consistent with a diagnosis of squamous cell carcinoma (Fig. 3D). To rule out the possibility of the intracranial metastasis of a squamous cell carcinoma, systemic workup was necessary, which yielded negative results. He underwent GKRS for treatment of the remnant malignant tumor. The tumor was covered with a 60% iso-dose gradient and the dose delivered to the tumor margin was 15 Gy; the maximum dose was 25 Gy. Thirteen months later, however, the enhanced volume had again enlarged. He underwent a second GKRS procedure with a marginal dose of 12 Gy; the maximum dose was 20 Gy. The adjacent brain stem tissue showed no evidence of adverse effects of radiation.
DISCUSSION
An epidermoid tumor is a congenital lesion that arises from inclusion of ectodermal epithelial elements8). Epidermoid cysts are benign and slow growing lesions representing about 1% of all intracranial tumors7-9). The CPA is the most common site of occurrence of intracranial epidermoid tumors, accounting for 7% of tumors in this region8). Grossly, epidermoid tumors are typically well defined lesions with an irregular nodular outer surface and a shiny "mother of pearl" appearance8,9). Microscopically, the wall of the epidermoid cyst consists of a layer of stratified squamous epithelium without vascularity. The cyst content is derived from desquamated epithelial cells composed mainly of keratin in concentric layers and cholesterol in a solid crystalline state6). Five months later, follow-up brain MRI showed focal enhanced mass on the right cerebellar hemisphere, there is outside operation field in our case. This finding was atypical. The small enhanced tumor was highly suggested malignant transformation. We performed a retrospective review of the initial pathological specimen did not uncover any evidence of squamous cell carcinoma. We recommended reoperation, but patient refused. Kida et al.10) reported that GKRS has also been used to treat recurrent benign epidermoids with reported shrinkage of the tumor and resolution of the patient's symptoms. Patient underwent GKRS. In cases of previously resected epidermoids when new contrast-enhancing lesions are seen, surgical exploration is necessary to document malignant transformation before adjuvant therapy is considered.
Their complication by squamous cell carcinoma is an unusual occurrence. Primary intracranial squamous cell carcinoma shares a rare but well-described association with benign intracranial epidermoid cysts7,9). These mechanisms of such transformation remain unclear. Malignant change in the epithelium-lining cyst is well documented. An 'in situ' carcinoma has been observed in an epidermoid cyst12,16). Concerning the mechanisms of malignant transformation of benign epidermoid cysts, some authors have suggested that introduction of a foreign material intraoperatively in combination with the inflammation-inducing contents of the epidermoid cyst, may be a cause of cellular atypia leading to neoplasia1,13).
Malignant transformation of intracranial epithelial cysts has been classified into five groups. These five groups include an initial malignant transformation of an epidermoid cyst, malignant transformation from a remnant epidermoid cyst, malignant transformation with leptomeningeal carcinomatosis, squamous cell carcinoma from other benign cysts, and other malignancies arising from the benign cysts9). According to Hamlat's classification, our case can be classified as malignant transformation from a remnant epidermoid cyst.
On MRI, epidermoid tumors typically have low signal intensity on T1-weighted images, high signal intensity on T2-weighted images that is similar to that of cerebrospinal fluid, and no enhancement on gadolinium-enhanced images6,11). In echo-planar DW imaging, all epidermoid tumors appeared sharply hyperintense relative to the brain and CSF3). DW imaging could differentiate epidermoid tumors from other cystic lesions, in that the apparent diffusion coefficient (ADC) of epidermoid tumors were similar to that of brain tissue whereas the ADCs of cystic lesions were similar to that of CSF3). Fast fluid-attenuated inversion recovery (fast-FLAIR) imaging of epidermoid tumors is featured by the increased signal intensity of surrounding CSF in the subarachnoid cisterns and ventricles2). In previous reports, characteristic MRI findings of malignant transformation of epidermoid cysts include a focal enhancing part within the mass and leptomeningeal metastasis7,9). The diagnosis of malignant transformation is still remained controversial, because of atypical features2,4,5,8). In the present case, MRI can show an enhanced part with associated vasogenic edema in the cerebellum and pons adjacent to the enhancing nodule. These findings were suggestive of malignant transformation of epidermoid cyst. Therefore, ongoing clinical and neuroimaging follow-up at yearly intervals is necessary for previous subtotal resection of the epidermoid cysts.
The treatment options are controversial. Only short-term follow up was available but the results were encouraging. Patients with subtotal resection should be followed up for the identification of recurrence and malignant transformation. In case suggesting malignant transformation, surgical exploration is necessary to confirm diagnosis. Unfortunately, the complete surgical resection of malignant transformation is usually limited to partial removal because the tumor firmly adheres to the neurovascular structures, as was the case with our case17). Surgery alone is not curative and limited. Radiation therapy (external-beam radiation or GKRS) after surgical treatment may offer better control of an intracranial squamous cell carcinoma. Tamura et al.17) performed a meta-analysis for the survival of intracranial squamous cell carcinomas arising in epidermoid cysts. They are compared among different treatment modalities (surgery alone, surgery plus external-beam radiation, and surgery plus GKRS)17). They suggested that GKRS appears to offer the best survival benefits on patients with intracranial squamous cell carcinomas17). Surgery plus GKRS is recommended for residual squamous cell carcinoma11,17). Most recently, Nagasawa et al.14) suggest that when determining the management for malignant transformation of epidermoid tumors, the combination of surgical resection and radiotherapy may be associated with improved short-term survival. Further investigation is necessary to obtain a beneficial treatment strategy against malignant transformation of epidermoid cysts.
CONCLUSION
We report a case of an epidermoid tumor in the CPA that transformed into a squamous cell carcinoma after resective surgery and GKRS. Malignant transformation is a rare cause of enhancement on MR images, as is progressive neurological deficit in a patient with an epidermoid cyst. The presence of contrast enhancement or progressive clinical symptoms within a typical epidermoid cyst along with rapid growth should alert the physician to the possibility of malignant transformation. GKRS has also been used to treat malignant transformation of epidermoids with reported shrinkage of the tumor and resolution of the patient's symptoms, however, only short-term follow up was available. Further investigation is necessary to obtain a beneficial treatment strategy against malignant transformation of epidermoid cysts.