INTRODUCTION
Dural arteriovenous fistulas (DAVFs) are abnormal vascular connections consisting abnormally of one or more meningeal feeding arteries that drain directly into a venous sinus or intracranial vein1,47,1018).
DAVFs can be found in any age group but they are mostly acquired lesions that present in the middle or late in life. Distal sinus occlusion or stenosis plays a major role behind fistula formation. Dural sinus thrombosis and inflammation play an important role in the development of acquired DAVFs. Pediatric DAVFs may be congenital malformation of the sinus that present early in neonatal or infantile period, or acquired lesions like those presenting late in life13,1416,17).
The pattern of venous drainage and the location of the fistula are the main factors affecting clinical presentation, also the presence of associated venous hypertension17). The range of presentations reported include audible bruit, headache, seizures, progressive neurological deficit, cerebellar symptoms and heart failure2,615,16). The risk of intra-cerebral hemorrhage increases markedly with the retrograde venous drainage, venous hypertension, and cortical venous reflux2,516). Drainage through the ophthalmic vein may cause ocular symptoms which include engorged vessels of the sclera, chemosis, proptosis, increase intraocular pressure and secondary glaucoma, diplopia, periorbital edema, limitation of extraocular muscle movement, and papillaedema2,56,1516,19). The severity of the ophthalmic symptoms might be related to the location and duration of intracranial DAVF which in turn affects the degree of venous drainage through the ophthalmic veins2,919). In general, posteriorly located DAVFs have fewer ocular symptoms than anterior ones16,1719).
We recently encountered two young children with exophthalmos resulting from direct fistula between the dural branches of the external carotid artery (ECA) and the transverse sinus, and both cases have retrograde venous drainage back to the cavernous sinus then to the ophthalmic veins.
CASE REPORT
Patient 1
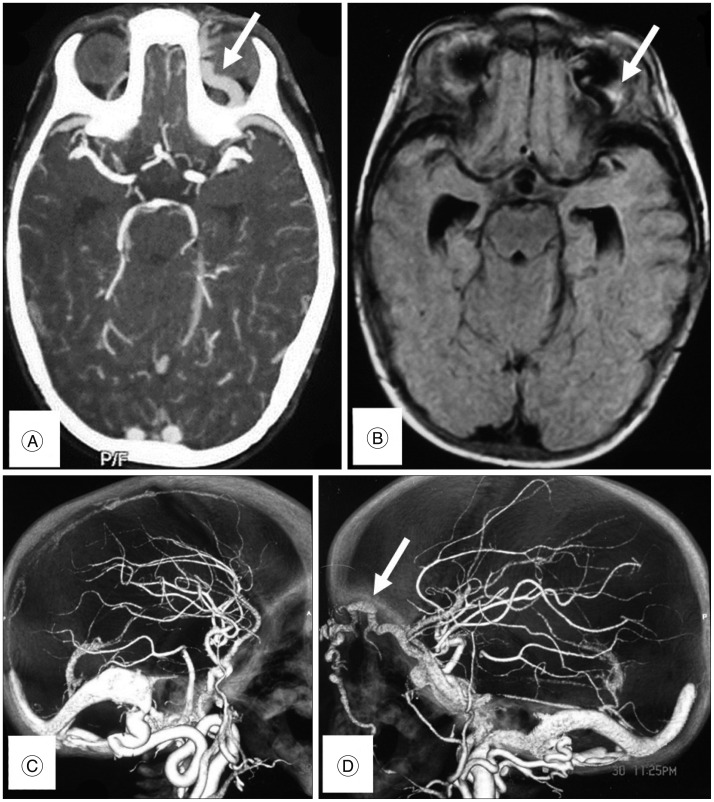
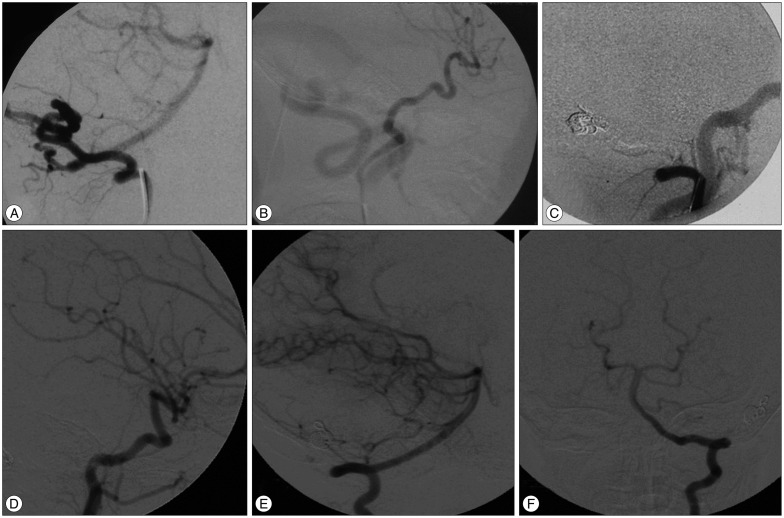
A Male child aged 2.5 year, had an orbital swelling of the left eye since birth with slow progressive course. On physical examination there was only exophthalmos with conjunctival congestion. MRI brain confirmed the presence of dilated tortuous cavernous sinus and left superior ophthalmic vein. CT angiography was done and it showed direct fistulous communication between left ECA branches and left transverse sinus with venous reflux into the deep venous system, cavernous sinus, and left superior ophthalmic vein. DSA revealed direct fistula of the transverse sinus supplied mainly by a hugely dilated occipital artery with minimal supply from the dural branches of left vertebral artery. Dysmaturation of the sigmoid sinus distal to the fistulous communication explained the occurrence of retrograde deep venous reflux, superior ophthalmic vein varicosity and exophthalmos. The DAVF of this patient was classified as type IIa according to Cognard's classification because of the retrograde flow through the sinus but with no retrograde flow into cortical veins. Endovascular embolization was performed with the patient under general anesthesia. A transarterial transfemoral approach was chosen. A 5 Fr Envoy guiding catheter (Cordis Neurovascular, Miami Lakes, FL, USA) was placed in the ECA after confirmation of the fistula site by DSA. An Excelsior® SL-10® microcatheter (Boston Scientific, Natick, MA, USA) was subsequently navigated over Transend 10 wire (Boston Scientific, Natick, MA, USA) to reach the site of the fistula at the left transverse sinus. Superselective angiography was then performed to confirm optimal position. The microcatheter was flushed continuously with hepranized normal saline. Guglielmi Detachable Coils (GDC; Boston Scientific Corporation, Natick, MA, USA) were introduced with simultaneous mechanical external compression of the occipital artery to decrease the flow in the fistula to allow for settling of the coils. Coiling is continued until disappearance of the flow inside the fistula. Then the microcatheter was flushed with 25% dextrose solution. Then N-butyl Cyanoacrylate (NBCA) at 50% concentration was used to achieve complete obliteration of the fistula. Control angiography was done at the end of the procedure to confirm obliteration of the fistula. The patient recovered completely without deficits. The ocular manifestation disappeared at 3 months follow up. Two years after embolization clinical and radiological follow up using DSA showed permanent obliteration of the fistula (Fig. 1, 2).
Patient 2
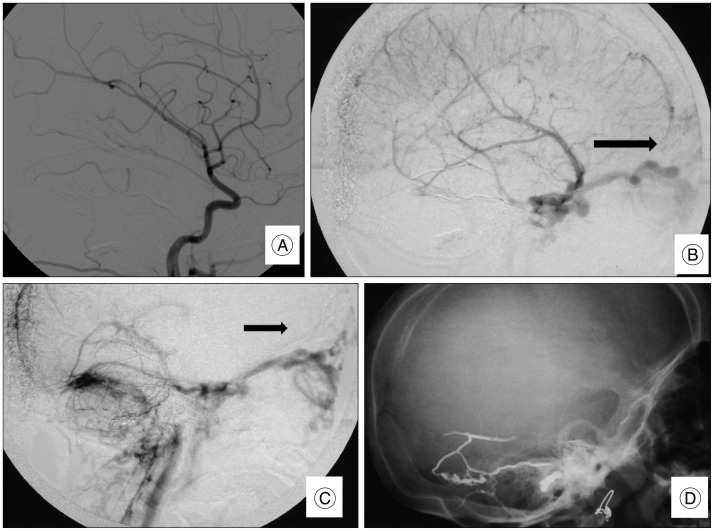
A female child aged 1.5 years, had an exophthalmos, conjunctival congestion, and eye lid varices since birth. MRI brain showed dilated and tortuous left ophthalmic veins. Endovascular intervention was decided under general anesthesia. Transfemoral DSA revealed bilateral direct fistulous communication between the left transverse sinus and the ECA branches. We observed bilateral dysmaturation of the sigmoid sinus that explained the retrograde venous reflux into the superficial and deep venous systems. The DAVF of this patient was classified as type IIb according to Cognard's classification because of the retrograde venous reflux through the sinus and cortical veins. The two fistulas were embolized over two sessions due to dye volume limitation in this young child. In the first session catheterization of the right ECA was performed via a transfemoral approach using standard coaxial techniques and with the catheter subject to continuous flushing with heparinized saline (4000 U of heparin per liter). A 4 Fr femoral sheath was introduced, followed by introduction of a 4 Fr catheter into the right ECA. An Excelsior® SL-10® microcatheter (Boston Scientific) was subsequently navigated over Transend 10 wire (Boston Scientific) through the right occipital artery to reach the fistula site. Superselective angiography was then performed to confirm optimal position. GDC (Boston Scientific Corporation) were introduced with simultaneous mechanical external compression of the occipital artery to decrease the flow in the fistula in order to allow the coils to settle in their desired location. Coiling was continued until disappearance of the flow inside the fistula. Then the microcatheter was flushed with 25% dextrose solution, and 50% NBCA was injected to fully obliterate the fistula. DSA was done at the end of the procedure to confirm obliteration of the fistula. The ocular manifestation disappeared partially after 3 month. The exophthalmos decreased but some orbital varicosities remained. A 2nd sessions was done after 6 months to occlude the left sided fistula. Under general anesthesia, a 5 Fr sheath was introduced through the right femoral artery. A 5 Fr Envoy guiding catheter (Cordis Neurovascular, Miami Lakes, FL, USA) was introduced through the left ECA. A 1.5 Fr Marathon microcatheter (Covidien, Irvine, CA, USA) microcatheter was navigated through the middle meningeal artery to reach the fistula then superselective angiogram was done. After reaching the optimum site and preparing the microcatheter using dimethyl-sulfoxide, Onyx-18 (Covidien, Irvine, CA, USA) was infused until complete obliteration. Final DSA revealed complete fistulous obliteration bilaterally, but the retrograde venous drainage through the whole venous system was observed due bilateral occlusion of the sigmoid sinuses. DSA follow up after 4 years revealed complete obliteration of the fistula, absence of the sigmoid sinus bilaterally, and the final venous drainage rerouted through the prevertebral, paravertebral, pterygoid venous plexus, and ophthalmic veins. Clinical follow up of this patient revealed presence of eye lid varicosities but no proptosis (Fig. 3, 4, 5).
DISCUSSION
Most of DAVFs are acquired and occur mostly after the 4th decade. Some lesions are reported to be congenital which are usually large direct shunts4,1318,19). The pathogenesis of DAVF is controversial. Various factors may contribute to their formation, such as sinus thrombosis, trauma or tumor invasion8,1819). The clinical presentations are related to the location of the fistula and the pattern of venous drainage12,17).
Ocular manifestation are related to the location and duration of the fistula, these manifestations occur mainly with anteriorly located fistulas17,19). In general, the more posterior the fistula, the fewer the ocular symptoms noted, and reported cases of associated ocular manifestations with posterior fossa DAVF are rare19). To our knowledge there are no reported cases of congenital direct AVF between the ECA and transverse sinus that present with proptosis. All reported cases are acquired and many arterial feeders are encountered from ECA and VA, the venous sinus involved included transverse, occipital, marginal, and IPS.
Liu et al.11) reported 2 cases of posterior fossa DAVFs presenting with exophthalmos, chemosis, and eyelid swelling resulting from retrograde venous drainage into the cavernous sinus and superior ophthalmic vein but the transverse sinus was not involved. The retrograde venous reflux passes through either the SPS or the cortical veins of the temporal lobe to the Sylvian veins to the cavernous sinus then to the ophthalmic veins.
McDougall et al.12) reported 14 adult patients with marginal sinus DAVF; One of these patients also had diplopia, chemosis, and proptosis due to retrograde venous drainage up the inferior petrosal sinus. Similarly, a second patient had chemosis but without proptosis or diplopia i.e., only 2 patients has ocular abnormalities related to posterior fossa DAVF again the transverse sinus was not involved.
Outlet obstruction increases the retrograde venous reflux; one of our cases (patient one) had dysmaturation of the sigmoid sinus which increased the venous reflux and the 2nd case had bilateral congenital obliteration of the sigmoid sinus. Mironov13) reported a case of inferior petrosal sinus DAVF presenting with contralateral exophthalmos which had distal obstruction of the IPS resulting in retrograde venous reflux into the cavernous sinus and ophthalmic veins. In our 2nd case the larger fistula was on the right side and the proptosis affected the left eye.
Endovascular treatment using platinum coils followed by glue used in our cases was an effective method in occlusion of DAVF. Liu et al.11) used the platinum coils and NBCA effectively in embolization of DAVFs. In our cases we used coils plus liquid embolic agents to obliterate the fistulae.
DAVFs usually develops after sinus occlusion due congenital atresia or acquired causes. Complete sinus occlusion results in interruption of the venous outflow and redirection of the venous drainage into the deep or superficial systems3). Cortical venous reflux is dangerous and results in intracranial hemorrhage. Retrograde venous drainage into the cavernous sinus, ophthalmic veins, emissary veins and vertebral venous plexuses represents an alternate pathway for sigmoid sinus dysmaturation. This was found typically in case two. It is important not to interrupt the anterior venous pathway during embolization in cases with occlusion or dysmaturation of the sigmoid sinus, as this anterior drainage takes up the normal venous drainage of the brain.
CONCLUSION
This report suggests that DAVF of the transverse sinus supplied by the external carotid branches can present with ophthalmic manifestations especially if there is distal venous stenosis or obliteration involving sigmoid sinus. Transarterial embolization using coils and liquid embolic agents could be safe and feasible to obliterate the fistula.