Lee, Yang, Park, Son, Hong, and Lee: Location of Ulnar Nerve Branches to the Flexor Carpi Ulnaris during Surgery for Cubital Tunnel Syndrome
Abstract
Objective
Cubital tunnel syndrome, the most common ulnar nerve entrapment neuropathy, is usually managed by simple decompression or anterior transposition. One of the concerns in transposition is damage to the nerve branches around the elbow. In this study, the location of ulnar nerve branches to the flexor carpi ulnaris (FCU) was assessed during operations for cubital tunnel syndrome to provide information to reduce operation-related complications.
Methods
A personal series (HJY) of cases operated for cubital tunnel syndrome was reviewed. Cases managed by transposition and location of branches to the FCU were selected for analysis. The function of the branches was confirmed by intraoperative nerve stimulation and the location of the branches was assessed by the distance from the center of medial epicondyle.
Results
There was a total of 61 cases of cubital tunnel syndrome, among which 31 were treated by transposition. Twenty-one cases with information on the location of branches were analyzed. The average number of ulnar nerve branches around the elbow was 1.8 (0 to 3), only one case showed no branches. Most of the cases had one branch to the medial head, and one other to the lateral head of the FCU. There were two cases having branches without FCU responses (one branch in one case, three branches in another). The location of the branches to the medial head was 16.3±8.6 mm distal to the medial epicondyle (16 branches; range, 0 to 35 mm), to the lateral head was 19.5±9.5 mm distal to the medial epicondyle (19 branches; range, -5 to 30 mm). Branches without FCU responses were found from 20 mm proximal to the medial condyle to 15 mm distal to the medial epicondyle (five branches). Most of the branches to the medial head were 15 to 20 mm (50% of cases), and most to the lateral head were 15 to 25 mm (58% of cases). There were no cases of discernable weakness of the FCU after operation.
Conclusion
In most cases of cubital tunnel syndrome, there are ulnar nerve branches around the elbow. Although there might be some cases with branches without FCU responses, most branches are to the FCU, and are to be saved. The operator should be watchful for branches about 15 to 25 mm distal to the medial epicondyle, where most branches come out.
Key Words: Cubital tunnel syndrome · Ulnar nerve · Flexor carpi ulnaris · Anterior transposition.
INTRODUCTION
Cubital tunnel syndrome is the second most common entrapment neuropathy in the upper extremity [ 5]. Patients usually complain of tingling of the 4th and 5th fingers and weakness of intrinsic muscles of the hand. This condition might be managed conservatively; however, cases with severe symptoms unresponsive to conservative management require surgical treatment. It can be managed by simple decompression, but some cases with complex anatomy or space-occupying-lesions require anterior transposition of the ulnar nerve [ 5, 6]. Compared to simple in-situ decompression, transposition of the nerve requires more extensive perineural dissection, which might compromise the blood supply to the nerve and damage to branches to the flexor carpi ulnaris (FCU) [ 4, 5]. For this, a thorough understanding of the anatomy of the motor branches of the ulnar nerve is necessary. There are several articles describing the branches to the FCU [ 2, 3, 8]. Previous studies examined cadaveric specimens and quantified the number and location of muscular branches of the ulnar nerve. In this study, we identified motor nerve branches of ulnar nerve to the FCU by intraoperative electrical stimulation and analyzed the location and number of branches and their functions.
MATERIALS AND METHODS
The study was approved by the IRB of Seoul National University Boramae Hospital (No. 30-2021-7). Informed consent was not required in this study due to its retrospective nature.
Patients who underwent surgery due to cubital tunnel syndrome from 2014 to 2019 were retrospectively reviewed. They had typical symptoms of cubital tunnel syndrome and were confirmed with electromyography (EMG) and a nerve conduction study. Surgical treatment was done for patients who did not show improvement of symptoms on conservative management or showed motor weakness of ulnar nerve-innervated muscles. Preoperative ultrasound was done in all patients. Among the surgical cases, anterior transposition was selected for cases with mass lesions in the cubital tunnel, ulnar nerve subluxation/dislocation on ultrasonography, and severe cubitus valgus.
Surgery was done under general anesthesia with initial loading of rocuronium before intubation. Immediately after intubation, neostigmine was administered to reverse muscle relaxant administered during the induction of anesthesia, and an assessment of function of ulnar nerve branches was performed about 15 minutes later. General anesthesia was maintained by propofol thereafter.
During anterior transposition, the branching pattern of the ulnar nerve was assessed. The location of branches of the ulnar nerve was measured from the center of the medial epicondyle, and the branches emerging distal to the medial epicondyle were expressed as positive numbers and proximal branches were expressed as negative numbers. The function of branches was confirmed by intraoperative nerve stimulation with NIM-Eclipse E3 software 3.5.353 (Medtronic®; Minneapolis, MN, USA).
The function of ulnar nerve branches was assessed by the following protocol. The EMG needle electrode was inserted at the hypothenar muscle and FCU medial and lateral heads. First, we found the main trunk of the ulnar nerve from the proximal cubital tunnel and directly applied electrical stimulation (0.5-1 mA). The strength of stimulus that evoked an EMG response on the hypothenar muscle was used for stimulating the branches of the ulnar nerve. Finally, we assessed a nerve branch as a motor branch when it showed an EMG response at the FCU on electrical stimulation.
RESULTS
In total, 61 cubital tunnel syndrome patients were reviewed, of which 31 cases were operated by transposition, and 21 cases with a description about the location of branches to the FCU were included for analysis.
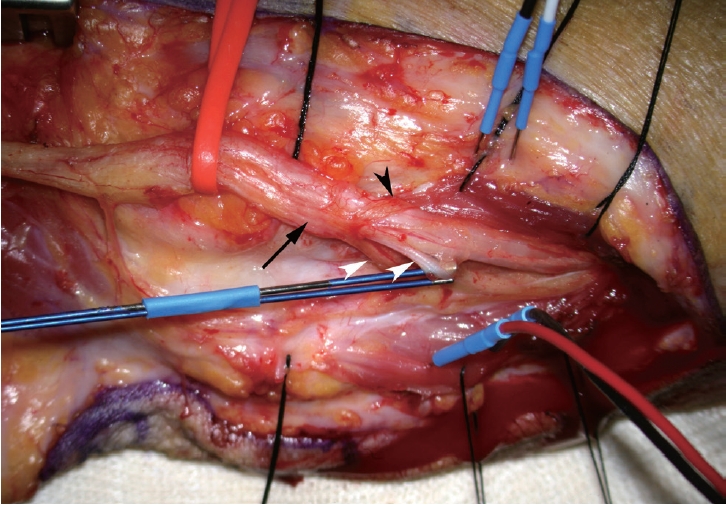
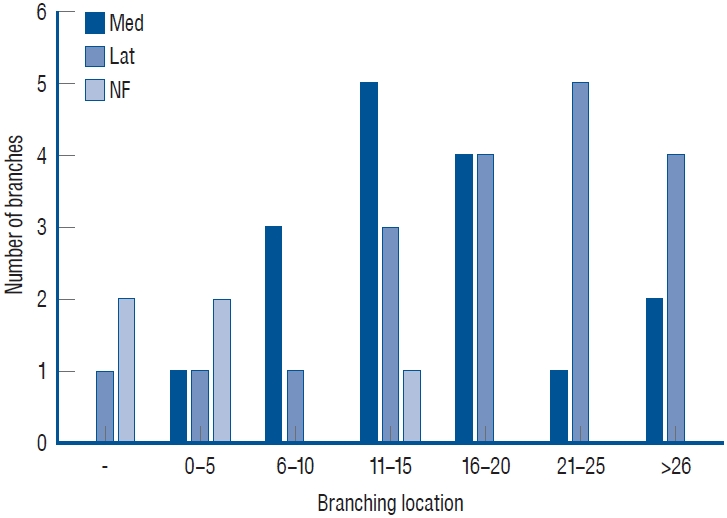
The number of ulnar nerve branches around the elbow was 0 to 3 (average, 1.8), and there was only one case that had no branches. In most of the cases, there was one branch to the medial head, and one other to the lateral head of the FCU. A branch without FCU response was found in three cases. Among them, branches with/without FCU responses co-existed in two cases, and there were only branches without FCU responses in the remaining case. The number of branches and their functions are summarized in Table 1. There was one case in which one common branch emerged from the main trunk of the ulnar nerve and divided into two branches, each supplying the medial and lateral heads of the FCU ( Fig. 1). The average location of branches to the medial head was 16.3±8.6 mm distal to the medial epicondyle (16 branches; range, 0 to 35 mm), while that of branches to the lateral head was 19.5±9.5 mm distal to the medial epicondyle (19 branches; range, -5 to 30 mm). Branches without FCU responses were found at -2+12.5 mm distal to the medial epicondyle (five branches; range, -20 to 15 mm) ( Fig. 2). Most branches to the medial head were located within 15 to 20 mm (50% of cases) and most branches to the lateral head were located within 15 to 25 mm (58% of cases). It was possible to save all the ulnar nerve branches by dissecting them from the main trunk of the ulnar nerve. There were no cases of discernable weakness of the FCU after operation.
DISCUSSION
Cubital tunnel syndrome is the second most common entrapment neuropathy in the upper extremity caused by ulnar nerve entrapment. Ulnar nerve decompression through surgical treatment is indicated when motor weakness occurs or conservative treatment fails [ 3]. In situ decompression, transposition of ulnar nerve into the subcutaneous, intramuscular, or submuscular plane, and medial epicondylectomy are surgical options for cubital tunnel syndrome [ 5]. While circumferentially dissecting the ulnar nerve during surgery, the motor branch to the FCU might be injured. The function of the FCU is flexion and adduction of the wrist, so an injury of the motor branch to the FCU can result in weakness of wrist motion. To avoid complications, thorough knowledge of the branching position is essential for preserving the function of the FCU. There have been several studies describing the location of ulnar nerve branches. Marur et al. [ 3] classified muscular branching patterns of the ulnar nerve to the FCU and flexor digitorum profundus (FDP) into four groups by analyzing 37 formalin-fixed forearms and showed that one or two branches were usually associated with the innervation of the FCU. The mean distances from the interepicondylar line to the location of the first muscular branch to the FCU or FDP were 15 mm and 35 mm, respectively [ 3]. Paulos and Leclercq [ 7] also dissected the ulnar nerve in 20 upper limbs of fresh frozen cadavers and classified the muscular branching patterns into four groups and 11 types. The locations of the first muscular branch to the FCU or FDP from the medial epicondyle were 14 mm and 50 mm, respectively [ 7]. The average location of the motor branch to the medial head of the FCU was 16.3 mm distal from the medial epicondyle in our study, so the data of this study are consistent with those reported in previous studies. Previous studies could give information about the location of ulnar nerve branches. However, the functions of the branches would not be confirmed by electrical stimulation considering the nature of cadaveric studies. To overcome this limitation, our study assessed the functions of the branches by intraoperative nerve stimulation, which was not attempted in previous studies. It has been reported that there are branches to the elbow joint in addition to muscular branches, such as articular branches [ 9]. Therefore, it is meaningful to check the function of nerve branches, and doing so provides more accurate information about the surgical anatomy of the ulnar nerve during operations for cubital tunnel syndrome. According to our results from 21 patients, it seems that the branching points of ulnar nerve branch show specific tendencies according to the branch function. The average locations of branches from the medial epicondyle of the humerus were -2.0 cm, 16.3 cm, and 19.5 cm for branches without FCU responses, medial, and lateral branches, respectively. This means that branches without FCU responses tended to emerge from more proximal locations, whereas branches from the distal side tended to be branches to the lateral head of the FCU. This tendency has not been previously reported. Most of the branches to the medial head were found within 15 to 20 mm (50% of cases) and those to the lateral head were found within 15 to 25 mm (58% of cases). Therefore, the surgeon needs to be aware of this area of the ulnar nerve during circumferential dissection. It is also notable that there was an anatomical variation of the common branch in one of the 21 cases, in which there was a common branch of the medial and lateral branch to the FCU, and this finding highlights the need for caution during dissection.
This study has a few drawbacks. First, this was not an anatomical study that would involve dissection of all branches of the ulnar nerve from its origin to the distal end. Nerve dissection was done in the surgical field around the elbow required for anterior transposition of the ulnar nerve. The purpose of our research was to provide practical information for neurosurgeons, so we did not perform extensive dissection to find branches outside the surgical field. Second, 21 cases are not sufficient to show a statistically significant trend of nerve branch location, so a study with more cases might validate the findings of our study. Third, we defined a branch without FCU responses as a branch that did not exhibit an EMG response on electrical stimulation. Although efforts were made to standardize conditions, such as applying an appropriate electrical stimulus strength to the ulnar nerve branch, there may be limitations in confirming the true function of this branch. It is not easy to elucidate the true function of the branches without FCU responses. It is known that there are articular branches to elbow joint, which usually originates in the cubital tunnel up to approximately 1 cm proximal to the medial epicondyle of ulnar nerve [ 1]. Ulnar nerve also gives off branches to other forearm muscles, especially for FDS. However, it is known that the first branch to the FDP usually arose on average 5.0 cm distal to the medial epicondyle [ 7]. Considering the branching locations, the branches without FCU responses might be an articular branch, but it is unlikely that they are branches to other muscles. That is one of the probable explanations for not significant dysfunctions of forearm muscles after operation. However, this study is meaningful in that there have been no reports of these functions being tested during surgery and we revealed the tendency for a relationship between the location and function of branches of the ulnar nerve. Although the number of cases analyzed in this study is not large, it is comparable to those of previously reported studies.
CONCLUSION
In this study, the function and location of ulnar nerve branches were analyzed. There was a tendency for branches without FCU responses to emerge from a more proximal location, with successively more distal locations observed for muscular branches to the medial head of the FCU and muscular branches to the lateral head of the FCU. When considering the distribution of motor nerve branches to the FCU, the operator should be watchful for branches about 15 to 25 mm distal to the medial epicondyle, where most branches emerge.
Acknowledgements
This work was partly supported by a clinical research fund of Seoul National University Boramae Hospital.
Fig. 1.
Photograph showing a common branch to the flexor carpi ulnaris (FCU) from the ulnar nerve taken during anterior transposition of the ulnar nerve left arm. A common branch emerges from the main trunk of the ulnar nerve (black arrow) and then splits into two branches to the medial head of the FCU (white arrowheads) and one branch to the lateral head of the FCU (black arrowhead). The left side of figure is the proximal side of the arm, and the upper side is the anterior side of the arm. 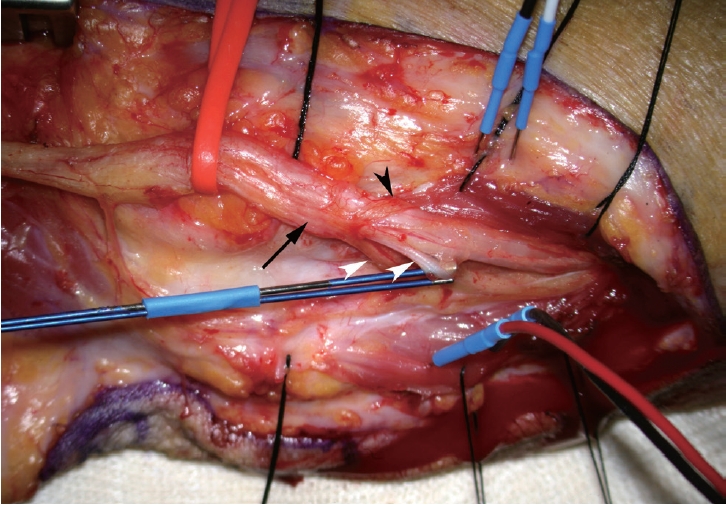
Fig. 2.
Location of branches measured from the medial epicondyle. The numbers on the horizontal axis are the distance from the medial epicondyle in millimeters (a negative number means proximal location) and the vertical axis represents the number of medial, lateral, and branches without flexor carpi ulnaris (FCU) responses. More proximal locations are associated with branches without FCU responses (NF), with successively more distal locations for the by medial heads of the flexor carpi ulnaris (Med) and lateral heads (Lat). 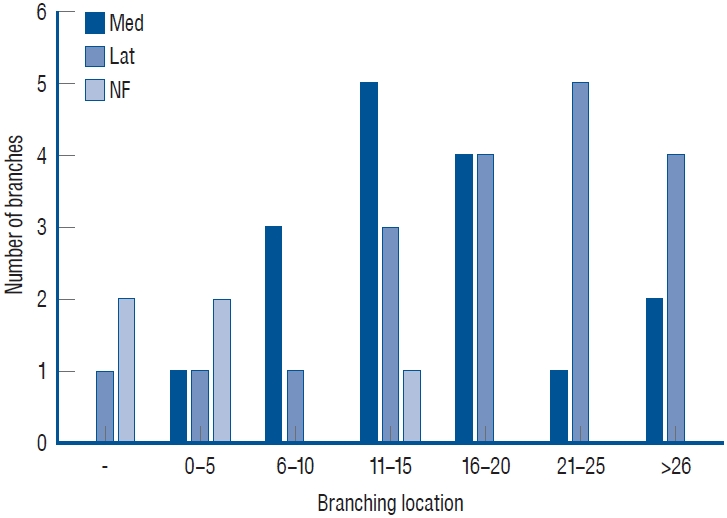
Table 1.
Number and function of ulnar nerve branches around the cubital tunnel
|
Number of branches |
Case |
Medial |
Lateral |
NF |
|
0 |
1 |
0 |
0 |
0 |
|
1 |
8 |
5*
|
4*
|
0 |
|
2 |
6 |
5 |
7 |
0 |
|
3 |
6 |
6 |
7 |
5 |
References
1. Doyle JR : Surgical Anatomy of the Hand and Upper Extremity. Philadelphia : Lippincott Williams & Wilkins, 2003, p204
2. Dugan SH, Lundgren M, Inouye S, Molen JV, Freemyer-Brown A : Variation in the origin of the first motor branch of the ulnar nerve to the flexor carpi ulnaris muscle. FASEB J 34( S1):1, 2020   3. Marur T, Akkin SM, Alp M, Demirci S, Yalçin L, Ogüt T, et al : The muscular branching patterns of the ulnar nerve to the flexor carpi ulnaris and flexor digitorum profundus muscles. Surg Radiol Anat 27 : 322-326, 2005    4. Ogata K, Manske PR, Lesker PA : The effect of surgical dissection on regional blood flow to the ulnar nerve in the cubital tunnel. Clin Orthop Relat Res ( 193):195-198, 1985  5. Palmer BA, Hughes TB : Cubital tunnel syndrome. J Hand Surg Am 35 : 153-163, 2010   7. Paulos R, Leclercq C : Motor branches of the ulnar nerve to the forearm: an anatomical study and guidelines for selective neurectomy. Surg Radiol Anat 37 : 1043-1048, 2015    8. Tubbs RS, Custis JW, Salter EG, Blount JP, Oakes WJ, Wellons JC 3rd : Quantitation of and landmarks for the muscular branches of the ulnar nerve to the forearm for application in peripheral nerve neurotization procedures. J Neurosurg 104 : 800-803, 2006   9. Watchmaker GP, Lee G, Mackinnon SE : Intraneural topography of the ulnar nerve in the cubital tunnel facilitates anterior transposition. J Hand Surg Am 19 : 915-922, 1994  
|
|