Yoon, Choi, and Jo: Comparison of Outcomes of Multi-Level Anterior, Oblique, Transforaminal Lumbar Interbody Fusion Surgery : Impact on Global Sagittal Alignment
Abstract
Objective
To compare the outcomes of anterior lumbar interbody fusion (ALIF), oblique lumbar interbody fusion (OLIF), and transforaminal lumbar interbody fusion (TLIF) in terms of global sagittal alignment.
Methods
From January 2007 to December 2019, 141 adult patients who underwent multilevel interbody fusion for lumbar degenerative disorders were enrolled. Regarding the approach, patients were divided into the ALIF (n=23), OLIF (n=60), and TLIF (n=58) groups. Outcomes, including local radiographic parameters and global sagittal alignment, were then compared between the treatment groups.
Results
Regarding local radiographic parameters, ALIF and OLIF were superior to TLIF in terms of the change in the anterior disc height (7.6±4.5 mm vs. 6.9±3.2 mm vs. 4.7±2.9 mm, p<0.001), disc angle (-10.0°±6.3° vs. -9.2°±5.2° vs. -5.1°±5.1°, p<0.001), and fused segment lordosis (-14.5°±11.3° vs. -13.8°±7.5° vs. -7.4°±9.1°, p<0.001). However, regarding global sagittal alignment, postoperative lumbar lordosis (-42.5°±9.6° vs. -44.4°±11.6° vs. -40.6°±12.3°, p=0.210), pelvic incidence-lumbar lordosis mismatch (7.9°±11.3° vs. 6.7°±11.6° vs. 11.5°±13.0°, p=0.089), and the sagittal vertical axis (24.3±28.5 mm vs. 24.5±34.0 mm vs. 25.2±36.6 mm, p=0.990) did not differ between the groups.
Conclusion
Although the anterior approaches were superior in terms of local radiographic parameters, TLIF achieved adequate global sagittal alignment, comparable to the anterior approaches.
Key Words: Spinal fusion · Lordosis · Lumbar vertebrae · Anterior lumbar interbody fusion · Transforaminal lumbar interbody fusion · Oblique lumbar interbody fusion.
INTRODUCTION
Lumbar interbody fusion (LIF) is the most commonly performed spinal procedure for the treatment of lumbar degenerative disorders. A wide range of fusion methods are available, including anterior, lateral, and posterior approaches, which are used according to the surgical indication, surgeon preference, and patient condition [ 17]. LIF can be divided into the anterior and posterior approaches based on the transverse process. Anterior approaches include anterior lumbar interbody fusion (ALIF), oblique lumbar interbody fusion (OLIF), and lateral lumbar interbody fusion (LLIF), whereas posterior approaches include posterior lumbar interbody fusion (PLIF) and transforaminal lumbar interbody fusion (TLIF) [ 11]. Anterior approaches grant surgeons a direct midline or lateral view of the disc space, which allows for more thorough endplate preparation, larger cage size, and greater increase in lordotic angle [ 8, 11, 27]. Conversely, posterior approaches provide excellent visualization of the nerve roots and spinal canal for direct decompression; however, they only allow cages with smaller footprints owing to the narrow surgical corridor [ 14]. Currently, conclusive evidence to show the superiority of a single approach in terms of fusion or clinical outcomes is lacking [ 11]. Several comparative studies have examined various LIF techniques, focusing on local radiographic characteristics, fusion rates, and clinical outcomes to provide a comparison [ 1, 2, 4, 7, 9, 10, 13, 23, 25]. However, most studies have only conducted one-to-one comparisons between two surgical techniques. Moreover, although multilevel LIF has been shown to impact global sagittal alignment and even result in an iatrogenic flatback, studies evaluating global sagittal alignment after LIF are scarce [ 1, 6, 13, 16, 23]. This study evaluated the surgical outcomes of various LIF approaches (ALIF, OLIF, and TLIF) for lumbar degenerative disorders. We compared the outcomes between the different treatment groups, with special consideration for spinopelvic parameters, to assess the impact of each approach on changes in global sagittal alignment.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board in Kyung Hee University Hospital at Gangdong (KHNMC 2022-02-005).
Patient population
From January 2007 to December 2019, the medical records of patients who underwent multi-level LIF surgeries were retrospectively reviewed. The patient inclusion criteria for this study were as follows : 1) adult (>18 years old) patients with lumbar degenerative disorders, 2) patients who underwent two- or three-level LIF between L1 and S1, and 3) completion of a minimum follow-up of 1 year. The patient exclusion criteria were 1) undergoing more than three-level fusion surgeries; 2) undergoing surgeries for infectious disease, trauma, or malignancy; 3) incomplete radiographic data, pre- or postoperatively (e.g., absent preoperative whole-spine radiographs); and 4) undergoing surgeries for tandem spinal lesions during the same hospitalization period. Additionally, patients who experienced traumatic spine disorder during the follow-up period were also excluded as this could impact global sagittal alignment. Regarding the mode of LIF, a total of 141 patients were divided into three groups : ALIF, OLIF, and TLIF. There were 23 patients in the ALIF group, 60 in the OLIF group, and 58 in the TLIF group who met the criteria and were included for comparison. Demographic data including age, sex, body mass index (BMI), follow-up period, history of lumbar spine surgery, comorbidities including osteoporosis, smoking status, and American Society of Anesthesiologists physical status classification were evaluated. Surgical data, including the level of fused vertebrae, characteristics of interbody cages, duration of surgery, estimated blood loss (EBL), length of hospital stay, and perioperative complications, were also collected.
Radiographic parameters
Spinopelvic parameters, including pelvic incidence (PI), lumbar lordosis (LL), pelvic tilt (PT), and sagittal vertical axis (SVA), were evaluated using whole-spine standing plain radiographs conducted preoperatively, immediately postoperatively, and 1-year postoperatively. LL was defined as the angle between the upper endplates of L1 and S1. Fused segment lordosis (FSL) was measured between the upper endplate of the most cranially fused vertebra and the lower endplate of the most caudally fused vertebra. Disc height (DH), disc angle (DA), and foraminal height (FH) were assessed at each segment using lateral plain radiographs both pre- and postoperatively. Anterior disc height (ADH) was measured as the distance between the inferior endplate and superior endplate at the anterior vertebral body line, and posterior disc height (PDH) was measured as the distance between the inferior endplate and superior endplate at the posterior vertebral body line. FH was measured as the distance between the adjacent pedicles at the index disc space. DA was determined as the angle between the inferior endplate and superior endplate at the index disc level. The fusion status was assessed using radiography. Fusion on the radiograph was defined as <5° of angular motion on flexion and extension radiographs, or where radiolucency lines exceeding 50% of the upper or lower surface of the implant with a width of >2 mm did not appear [ 5, 24]. In cases of ALIF, most (20/23) were performed in a single session, although three cases were staged operations. Posterior decompression was performed in all ALIF cases. Cages with various angles ranging from 8° to 18° were used. In cases of OLIF, the majority of patients (43/58) underwent a staged operation, while the remaining patients (15/58) underwent a single session. In earlier cases, cages with an angle of 6° were used. Thereafter, we used hyperlordotic cages with angles of 18° and 25°. In cases of TLIF, all were performed in a single posterior session, and interbody cages with angles of 4° or 8° were used.
Statistical analysis
All continuous variables are presented as the mean±standard deviation for each group and were subjected to statistical analysis using SPSS version 25.0 (IBM Corp., Armonk, NY, USA). Analysis of variance and Kruskal-Wallis tests were used to compare the numerical data between the groups. A post hoc test was conducted using Scheffe’s method if there were significant differences between the groups. The chi-square test and Fisher’s exact test were used to compare categorical data between the groups. The paired t-test was used to analyze changes in radiographic parameters after surgery. Statistical significance was set to p<0.05.
RESULTS
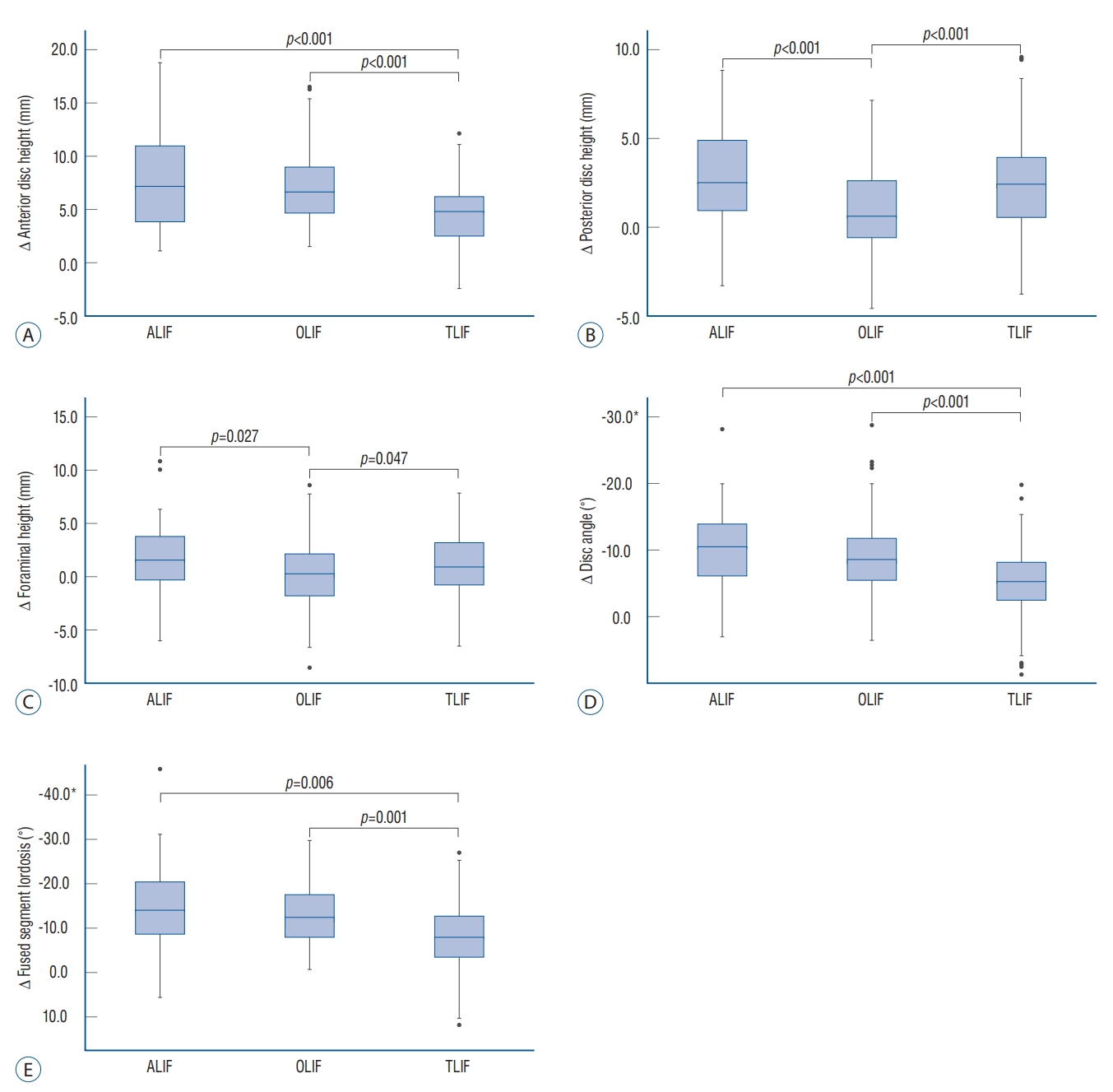
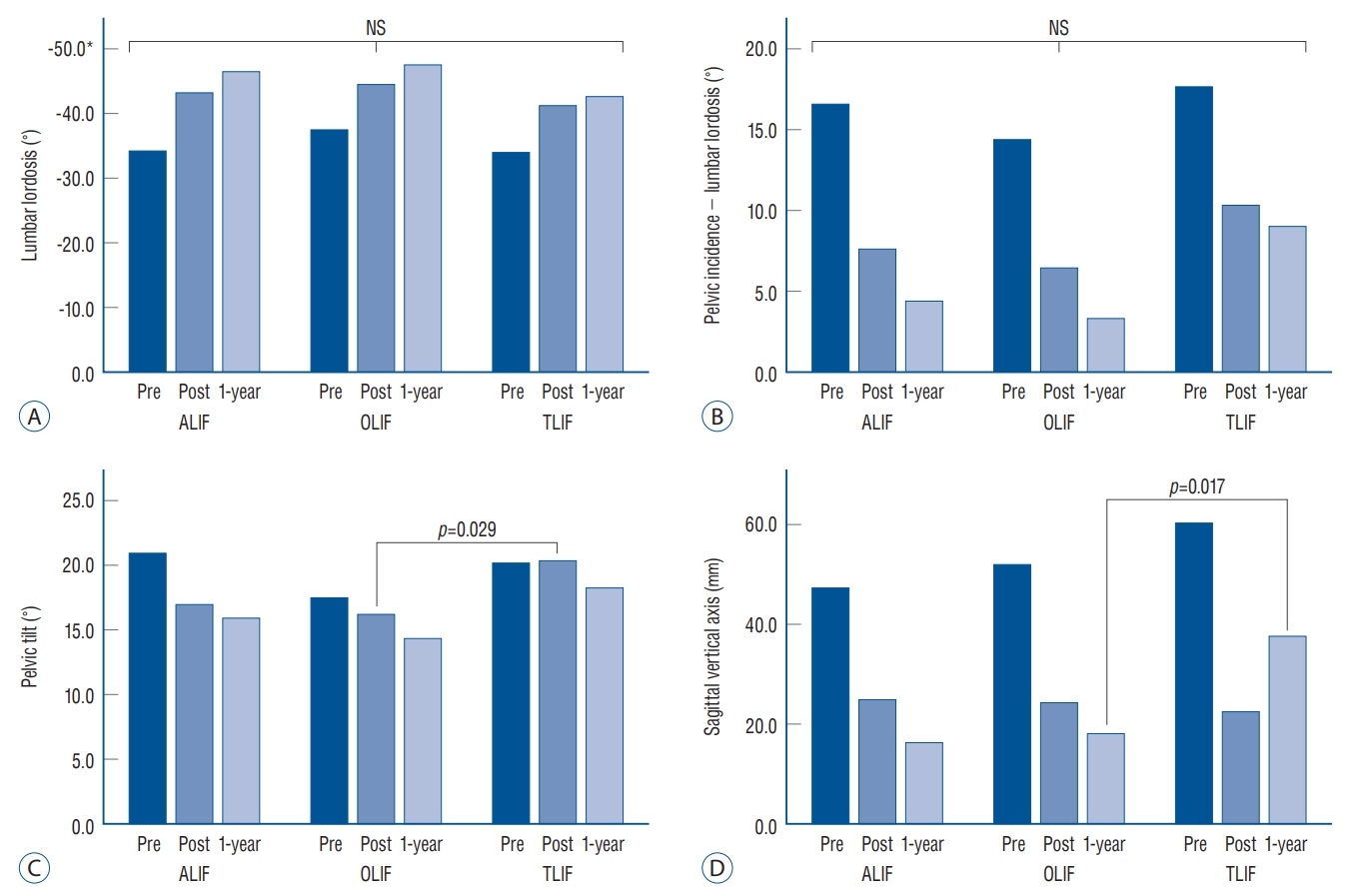
The patient demographic data are summarized in Table 1. The baseline characteristics of patients, including mean age, sex, BMI, comorbidities, and smoking status, did not differ between the treatment groups. The most common level of fusion in all groups was L4/5 (n=137), followed by L3/4 (n=98), and L5/S1 (n=51) ( Table 2). The proportion of fusion at the L5/S1 level was different between the groups. Only eight patients (13.3%) underwent L5/S1 fusion in the OLIF group, whereas 13 (56.5%) and 30 (51.7%) patients underwent L5/S1 fusion in the ALIF and TLIF groups, respectively. The mean height of the interbody cage was significantly greater in the ALIF (14.2±1.7 mm) and OLIF (14.3±1.5 mm) groups than in the TLIF group (11.5±1.2 mm, p<0.001). The mean angle of the interbody cage was also significantly different between the groups (11.8°±2.7° vs. 16.0°±5.6° vs. 5.6°±2.1°, p<0.001). The mean duration of surgery was significantly longer in the ALIF group (265.1±54.2 minutes) than in the OLIF group (226.8±62.3 minutes, p=0.022). The mean EBL and length of hospital stay did not differ between the groups. Moreover, fusion rates (95.7% vs. 96.7% vs. 98.3%, p=0.815) did not differ between the groups. The preoperative and postoperative values of DH, DA, and FH are summarized in Table 3 and Fig. 1. Postoperative ADH was significantly greater in the ALIF (18.5±3.1 mm) and OLIF groups (17.4±2.3 mm) than in the TLIF group (15.3±2.7 mm, p<0.001). The mean increase in ADH was also significantly greater in the ALIF (7.6±4.5 mm) and OLIF (6.9±3.2 mm) groups than in the TLIF group (4.7±2.9 mm, p<0.001). The mean increase in PDH was significantly less in the OLIF group (1.0±2.4 mm, p<0.001) than in the ALIF (2.7±2.7 mm) and TLIF (2.4±2.6 mm) groups. Moreover, the mean increase in FH was lower in the OLIF group (0.2±2.9 mm, p=0.007) than in the ALIF (1.5±3.4 mm) and TLIF (1.1±2.8 mm) groups. Although DA was significantly increased in all groups postoperatively, the mean change in DA was significantly greater in the ALIF (-10.0°±6.3°) and OLIF (-9.2°±5.2°) groups than in the TLIF group (-5.1°±5.1°, p<0.001). The mean postoperative FSL was significantly greater in the ALIF (-33.7°±9.4°) and OLIF (-33.7°±9.7°) groups than in the TLIF group (-27.3°±9.0°, p=0.001). The mean change in FSL was also greater in the ALIF (-14.5°±11.3°) and OLIF (-13.8°± 7.5°) groups than in the TLIF group (-7.4°±9.1°, p<0.001). The perioperative spinopelvic parameters are summarized in Table 4 and Fig. 2. The mean postoperative LL (-42.5°±9.6° vs. -44.4°±11.6° vs. -40.6°±12.3°, p=0.210) and correction amount of LL (-8.6°±10.5° vs. -8.1°±9.5° vs. -6.4°±11.0°, p=0.574) did not differ between the groups ( Figs. 3 and 4). Although the differences were not statistically significant, the PI-LL mismatch tended to be less in the ALIF and OLIF groups than in the TLIF group postoperatively (7.9°±11.3° vs. 6.7°±11.6° vs. 11.5°±13.0°, p=0.089) and 1-year postoperatively (4.4°±11.0° vs. 3.4°±12.9° vs. 9.0°±15.5°, p=0.091). The mean postoperative PT was significantly lower in the OLIF group (16.3±8.9 mm) than in the TLIF group (20.9±9.9 mm, p=0.029). However, the difference between the groups disappeared at 1-year postoperatively (15.9±8.0 mm vs. 14.3±8.9 mm vs. 18.2±13.0 mm, p=0.159) ( Fig. 5). The postoperative SVA (24.3±28.5 mm vs. 24.5±34.0 mm vs. 25.2±36.6 mm, p=0.990) did not differ between the groups. However, the 1-year postoperative SVA was significantly lower in the OLIF group (18.0±29.1 mm) than in the TLIF group (37.7±40.7 mm, p=0.017). The perioperative complications are summarized in Table 5. The incidence of total perioperative complications was the highest in the ALIF group (47.8% vs. 23.3% vs. 25.9%); however, the difference was not statistically significant ( p=0.725). The most common perioperative complications were urinary disturbances (n=13), wound infections (n=4), and pulmonary congestion (n=4). Two patients each had an incisional hernia (both in the ALIF group) and minor vascular injury (one each in the ALIF and OLIF groups). No visceral or ureteral injuries occurred in patients who underwent the anterior approach.
DISCUSSION
In the present study, we compared the surgical outcomes among various LIF approaches, including ALIF, OLIF, and TLIF, paying particular attention to global sagittal alignment. The anterior approaches, including ALIF and OLIF, achieved superior correction of the ADH, DA, and FSL compared with TLIF. Regarding global sagittal alignment, however, the three approaches were not significantly different in terms of the postoperative spinopelvic parameters LL, PI-LL mismatch, and SVA. Although postoperative PT was significantly greater in the TLIF group than in the OLIF group (20.9° vs. 16.3°), the difference disappeared 1-year postoperatively (18.2° vs. 14.3°). Therefore, despite the greater improvement in local radiographic parameters in ALIF and OLIF than in TLIF, the superiority of the anterior approach for global sagittal alignment was not clear.
Many studies have evaluated the local radiographic findings following various LIF methods. Hsieh et al. [ 4] reported that ALIF resulted in significantly improved DA and FH compared to TLIF. In a study comparing the three different approaches, Watkins et al. [ 25] concluded that ALIF and LLIF resulted in greater changes in DH and FSL than TLIF. These findings suggest that the anterior approach enables the insertion of larger cages and the creation of greater lordosis and are consistent with the present study in terms of greater correction of ADH, DA, and FSL. However, in contrast to several other studies, improvements in PDH and FH were not obvious in this study [ 4, 25]. Because lordosis is considered more important than foraminal widening with indirect decompression, we routinely placed hyperlordotic cages as anteriorly as possible, combined with direct foraminal decompression and posterior column shortening. These processes would have resulted in minimal changes in PDH and FH. Regarding global sagittal alignment, the authors noticed two principal findings in the present study. 1) In general, postoperative spinopelvic parameters, including LL, PI-LL mismatch, and SVA, were not significantly different among the three groups. 2) All measured postoperative spinopelvic parameters, including PI-LL mismatch (≤10°), PT (≤20°), and SVA (≤4 cm), were within the acceptable range in all three groups according to the Scoliosis Research Society-Schwab classification [ 19- 21]. Although the postoperative PT was 20.9° immediately post-operatively, which was significantly greater in the TLIF group than in the OLIF group, the value decreased to 18.2° (≤20°), and the difference disappeared at 1-year postoperatively. These findings conflict with those of previous studies which reported the inferiority of the posterior approach compared with the anterior approach in terms of the correction of spinopelvic parameters. Nakashima et al. [ 13] reported that LLIF produced significantly better postoperative spinopelvic parameters, including LL, PI-LL mismatch, and PT (exclusively in three-level surgery) than TLIF. Other researchers have also demonstrated that anterior approaches achieve significantly greater postoperative LL than posterior approaches [ 1, 9, 10, 26]. The main disparity between our study and previous studies resulted from the amount of spinopelvic parameter correction in TLIF. Previous studies achieved additional lordosis following PLIF or TLIF to a mild degree, sometimes even achieving a negative value (from -5.2° to 4.2°) owing to little correction of the Cobb angle per segment (from -0.7° to 2.6°). In this study, we achieved a greater amount of LL correction (6.4°) owing to the 5.1° of correction per segment following TLIF. We believe that the greater amount of TLIF correction could be attributed to bilateral facetectomies, which allowed posterior column shortening. Following bilateral facetectomies, we could achieve posterior column shortening and resultant lordosis by rod assembly with compressive force. Therefore, with careful consideration of LL through posterior column shortening, TLIF can achieve adequate LL as well as global sagittal alignment comparable to anterior approaches such as ALIF and OLIF. It is worth noting that the increase in LL (-8.6° vs. -8.1° vs. -6.4°) was less than that in FSL (-14.5° vs. -13.8° vs. -7.4°) in all three groups. This finding correlated with the previous study by Sembrano et al. [ 22], which demonstrated a trend toward a decrease in adjacent lordosis after LIF, in contrast to increased FSL. We considered that the decrease in intraspinal compensation could be a reason for the smaller change in LL than in FSL. The shorter duration of surgery in OLIF in this study may reflect the easier exposure and lower manipulation of visceral and vascular structures compared with ALIF, although the difference was not significant in another study [ 2]. Some researchers have reported that the duration of surgery was shorter with OLIF than with TLIF or minimally invasive TLIF; however, the difference between OLIF and TLIF did not reach statistical significance in this study. EBL did not differ between the groups in this study. According to previous studies, the impact of the surgical approach on EBL was also inconclusive [ 2, 9], although some reported that TLIF was associated with an increased EBL compared with ALIF or OLIF [ 10, 12]. Fusion and complication rates did not differ between the groups, which is consistent with most previous reports [ 2, 9, 15, 23]. This study has several limitations. First, this study was retrospective and did not involve randomization. Therefore, there was significant heterogeneity between the groups in terms of surgical details. For example, the proportion of fusion at the L5/S1 level was much lower in the OLIF group (13.3%) than in the other groups (56.5% in ALIF group, 51.7% in TLIF group). In the initial stages of OLIF adoption, if fusion at the L5/S1 level was necessary, we conducted ALIF more often than OLIF due to technical considerations. Such a decision on approach could impact the heterogeneity between the groups. Second, the sample size was relatively small, particularly in the ALIF group. Because we shifted the principal anterior approach from ALIF to OLIF, the number of patients in the ALIF group was small. Third, we only included multi-level LIF surgeries and excluded single-level surgeries, although single-level LIFs vastly outnumber multi-level LIFs. However, we evaluated global sagittal alignment exclusively for multilevel LIF surgeries because the impact of single-level surgeries on global sagittal alignment is limited [ 3, 9, 18, 23]. Lastly, we did not collect patient-reported outcome questionnaires for short-level fusion surgeries; therefore, the lack of clinical outcomes was another weakness of this study.
CONCLUSION
The anterior approaches, including ALIF and OLIF, resulted in greater changes in ADH, DA, and FSL than TLIF. However, regarding global sagittal alignment, there were no significant differences in postoperative LL, PI-LL mismatch, or SVA between the groups, and the postoperative spinopelvic parameters were acceptable in all three groups. Although anterior approaches, including ALIF and OLIF, were superior to TLIF in terms of local radiographic parameters, TLIF could provide adequate global sagittal alignment, comparable to that of the anterior approaches.
Fig. 1.
Changes in local radiographic parameters after multilevel lumbar interbody fusion according to the approaches. A : changes in anterior disc height. B : changes in posterior disc height. C : changes in foraminal height. D : changes in disc angle. E : changes in fused segment lordosis. *Negative values indicate lordosis. ALIF : anterior lumbar interbody fusion, OLIF : oblique lumbar interbody fusion, TLIF : transforaminal lumbar interbody fusion. 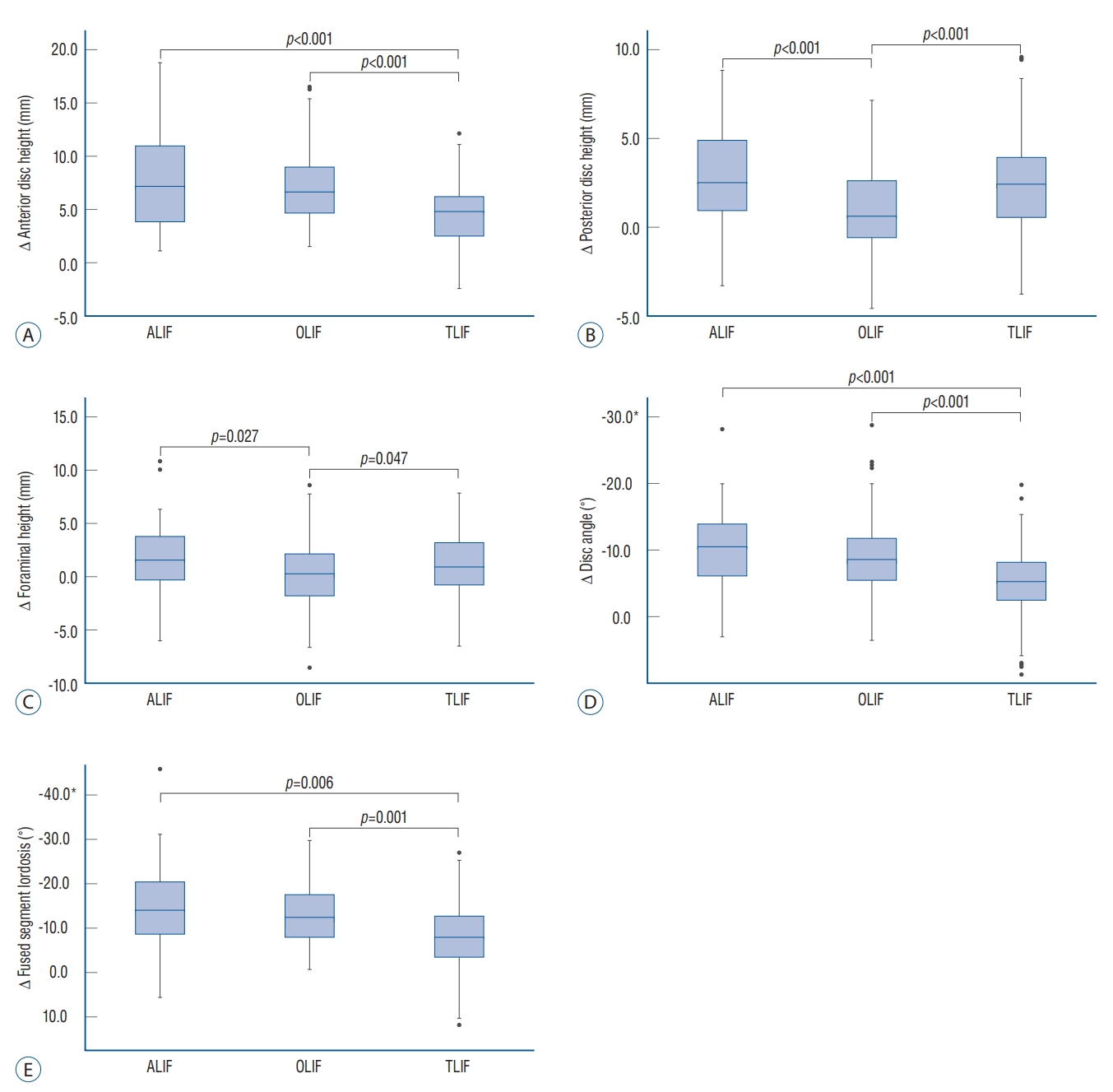
Fig. 2.
Changes in global sagittal alignment after multilevel lumbar interbody fusion according to the approaches. A : changes in lumbar lordosis. B : changes in pelvic incidence - lumbar lordosis. C : changes in pelvic tilt. D : changes in sagittal vertical axis. *Negative values indicate lordosis. NS : not significant, ALIF : anterior lumbar interbody fusion, OLIF : oblique lumbar interbody fusion, TLIF : transforaminal lumbar interbody fusion. 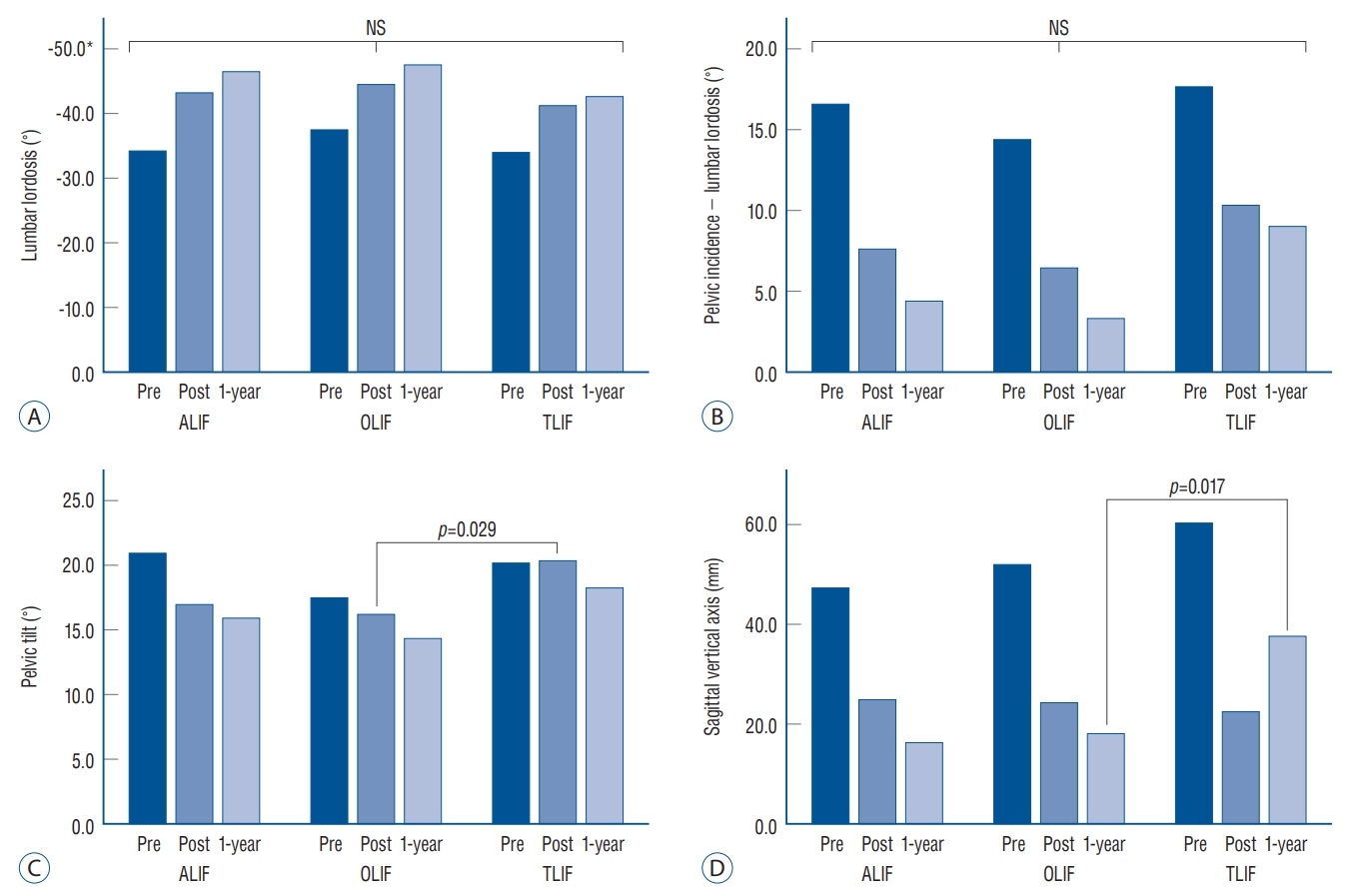
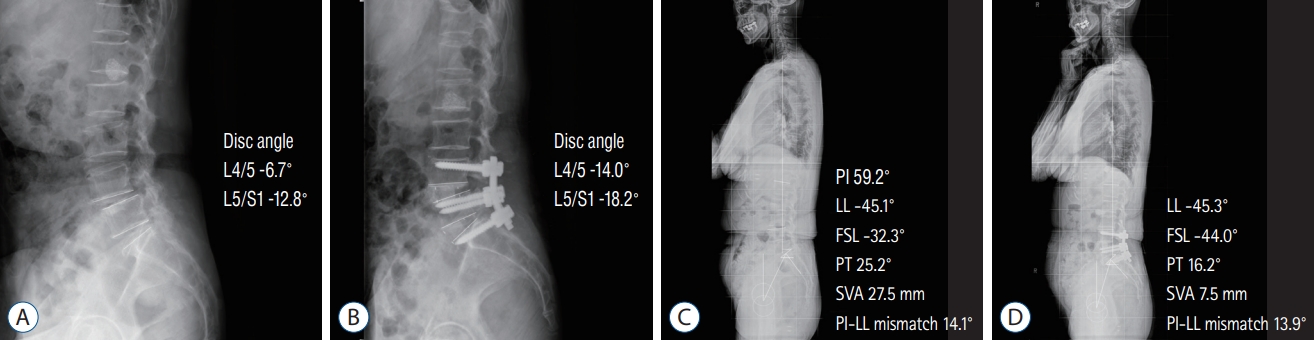
Fig. 3.
A 74-year-old woman underwent anterior lumbar interbody fusion (ALIF) at L4-S1. A and B : Preoperative and postoperative radiographs revealed an increased disc angle following ALIF. D and D : Preoperative and 1-year postoperative standing radiographs, respectively. Improvements in fused segment lordosis (FSL) (from -32.3° to -44.0°) and pelvic incidence (PI) (from 25.2° to 16.2°) were observed after surgery. However, the change in lumbar lordosis (LL) was trivial (from -45.1° to -45.3°), possibly due to a decrease in intraspinal compensation. PT : pelvic tilt, SVA : sagittal vertical axis. 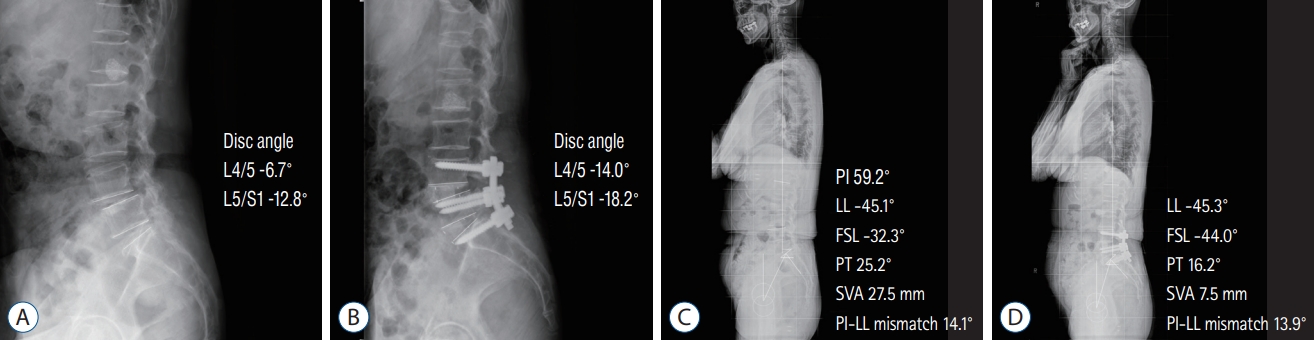
Fig. 4.
A 66-year-old woman underwent oblique lumbar interbody fusion (OLIF) at L3-5. A and B : Preoperative and postoperative radiographs revealed an increased disc angle following OLIF. C and D : Preoperative and 1-year postoperative standing radiographs, respectively. Improvements in fused segment lordosis (FSL) (from -12.7° to -38.6°) and pelvic incidence (PI) (from 32.4° to 13.1°) were observed following surgery. Lumbar lordosis (LL) was markedly increased following surgery (from -25.1° to -46.4°). PT : pelvic tilt, SVA : sagittal vertical axis. 
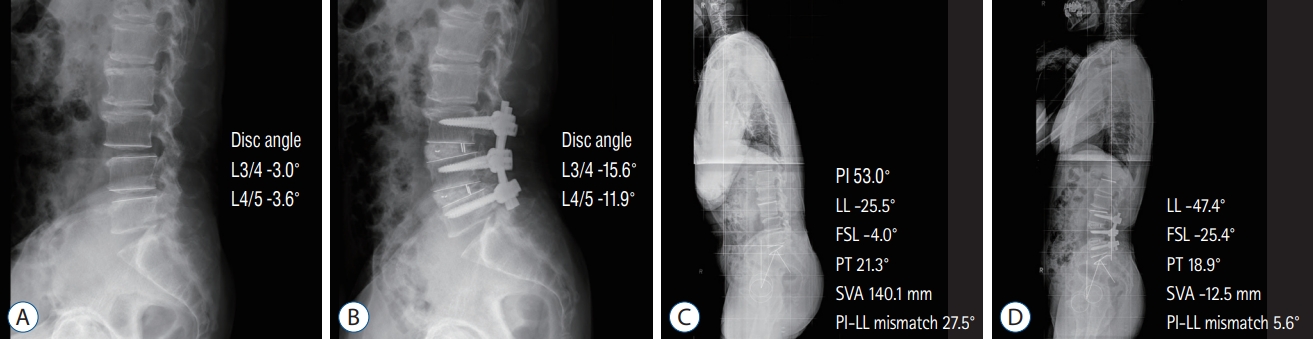
Fig. 5.
A 70-year-old man underwent transforaminal lumbar interbody fusion (TLIF) at L3-5. A and B : Preoperative and postoperative radiographs revealed an increased disc angle following TLIF. C and D : Preoperative and 1-year postoperative standing radiographs, respectively. Fused segment lordosis (FSL) (from -4.0° to -25.4°) was improved following surgery. Spinopelvic parameters, including lumbar lordosis (LL) (from -25.5° to -47.4°), pelvic incidence (PI) (from 21.3° to 18.9°), and sagittal vertical axis (SVA) (from 140.1 mm to -12.5 mm) were also improved following surgery. PT : pelvic tilt. 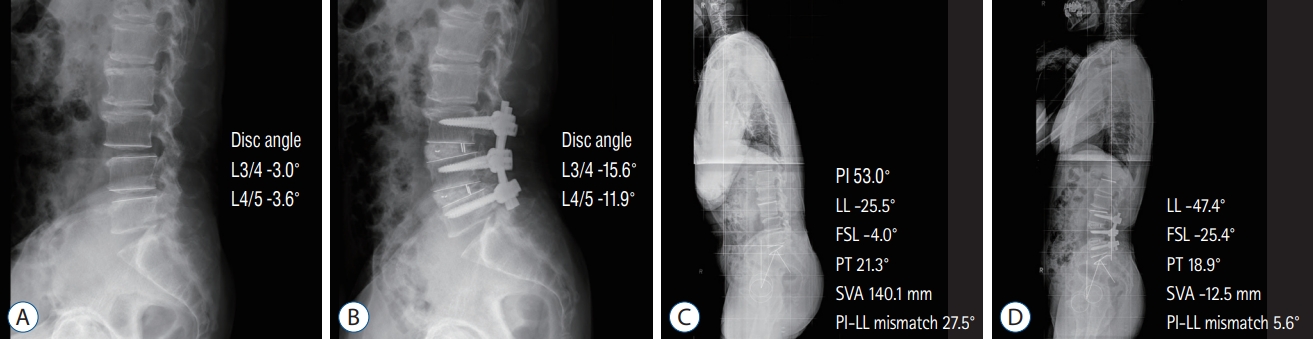
Table 1.
demographic data of the different treatment groups
|
ALIF (n=23) |
OLIF (n=60) |
TLIF (n=58) |
p-value |
|
Age (years) |
60.3±9.3 |
66.0±8.4 |
66.3±9.6 |
0.174 |
|
Male : female |
8 : 15 |
23 : 37 |
19 : 39 |
0.707 |
|
Body mass index (kg/m2) |
25.6±3.7 |
25.0±2.9 |
24.8±3.0 |
0.628 |
|
Follow-up period (years) |
3.7±2.9 |
2.4±1.3 |
4.3±2.8 |
0.003 |
|
Previous operation (%) |
26.1 |
21.7 |
13.8 |
0.362 |
|
Hypertension (%) |
47.8 |
53.3 |
62.1 |
0.435 |
|
Diabetes mellitus (%) |
21.7 |
21.7 |
25.9 |
0.847 |
|
Osteoporosis (%) |
36.8 |
25.5 |
34.7 |
0.513 |
|
BMD (T-score) |
-1.9±1.2 |
-1.6±1.0 |
-2.0±0.9 |
0.168 |
|
Antiplatelet medication (%) |
21.7 |
18.3 |
25.9 |
0.847 |
|
Smoking (%) |
17.4 |
13.3 |
10.3 |
0.627 |
|
ASA PS classification |
2.1±0.5 |
2.0±0.5 |
2.0±0.4 |
0.615 |
Table 2.
|
ALIF (n=23) |
OLIF (n=60) |
TLIF (n=58) |
p-value |
|
Number of fused segments |
|
|
|
|
|
2-level |
21 |
40 |
51 |
|
|
3-level |
2 |
20 |
7 |
|
|
Level of fused |
|
|
|
|
|
L1/2 |
|
|
1 |
|
|
L2/3 |
2 |
16 |
6 |
|
|
L3/4 |
10 |
57 |
31 |
|
|
L4/5 |
23 |
59 |
55 |
|
|
L5/S1 |
13 |
8 |
30 |
|
|
Interbody cage height (mm) |
14.2±1.7 |
14.3±1.5 |
11.5±1.2 |
<0.001 |
|
Interbody cage angle (˚) |
11.8±2.7 |
16.0±5.6 |
5.6±2.1 |
<0.001 |
|
Surgical time (minutes) |
265.1±54.2 |
226.8±62.3 |
236.5±48.9 |
0.022 |
|
Estimated blood loss (mL) |
687.0±230.2 |
735.0±268.0 |
675.9±231.2 |
0.547 |
|
Length of hospital stay (days) |
16.0±8.3 |
12.9±4.3 |
13.2±5.4 |
0.287 |
|
Fusion rate (%) |
95.7 |
96.7 |
98.3 |
0.815 |
Table 3.
Pre- and postoperative values of local radiographic parameters
|
ALIF (n=23) |
OLIF (n=60) |
TLIF (n=58) |
p-value |
|
Anterior disc height (mm) |
|
|
|
|
|
Preoperative |
10.9±4.3 |
10.5±3.4 |
10.6±3.5 |
0.765 |
|
Postoperative |
18.5±3.1 |
17.4±2.3 |
15.3±2.7 |
<0.001 |
|
Correction |
7.6±4.5 |
6.9±3.2 |
4.7±2.9 |
<0.001 |
|
Posterior disc height (mm) |
|
|
|
|
|
Preoperative |
6.6±2.4 |
6.3±2.0 |
6.3±2.1 |
0.782 |
|
Postoperative |
9.2±2.4 |
7.3±2.1 |
8.7±2.3 |
<0.001 |
|
Correction |
2.7±2.7 |
1.0±2.4 |
2.4±2.6 |
<0.001 |
|
Foraminal height (mm) |
|
|
|
|
|
Preoperative |
18.0±3.6 |
19.3±3.2 |
17.7±3.1 |
<0.001 |
|
Postoperative |
19.5±3.0 |
19.5±3.3 |
18.8±2.9 |
0.121 |
|
Correction |
1.5±3.4 |
0.2±2.9 |
1.1±2.8 |
0.007 |
|
Disc angle (˚) |
|
|
|
|
|
Preoperative |
-5.3±5.6 |
-6.0±4.4 |
-6.9±5.2 |
0.101 |
|
Postoperative |
-15.2±4.6 |
-15.2±4.7 |
-12.0±4.8 |
<0.001 |
|
Correction |
-10.0±6.3 |
-9.2±5.2 |
-5.1±5.1 |
<0.001 |
|
Fused segment lordosis (˚) |
|
|
|
|
|
Preoperative |
-19.2±8.2 |
-19.9±11.1 |
-19.9±10.8 |
0.958 |
|
Postoperative |
-33.7±9.4 |
-33.7±9.7 |
-27.3±9.0 |
0.001 |
|
Correction |
-14.5±11.3 |
-13.8±7.5 |
-7.4±9.1 |
<0.001 |
Table 4.
Pre- and postoperative values of global sagittal alignment
|
ALIF (n=23) |
OLIF (n=60) |
TLIF (n=58) |
p-value |
|
PI (˚) |
50.4±10.2 |
51.0±10.6 |
52.1±9.9 |
0.748 |
|
LL (˚) |
|
|
|
|
|
Preoperative |
-33.9±10.5 |
-36.3±14.0 |
-34.2±12.5 |
0.610 |
|
Postoperative |
-42.5±9.6 |
-44.4±11.6 |
-40.6±12.3 |
0.210 |
|
Correction |
-8.6±10.5 |
-8.1±9.5 |
-6.4±11.0 |
0.574 |
|
1-year postoperative |
-46.2±10.5 |
-47.4±12.3 |
-42.5±13.8 |
0.124 |
|
PI-LL mismatch (˚) |
|
|
|
|
|
Preoperative |
16.4±13.3 |
14.7±15.2 |
17.9±13.6 |
0.480 |
|
Postoperative |
7.9±11.3 |
6.7±11.6 |
11.5±13.0 |
0.089 |
|
1-year postoperative |
4.4±11.0 |
3.4±12.9 |
9.0±15.5 |
0.091 |
|
Pelvic tilt (˚) |
|
|
|
|
|
Preoperative |
20.7±10.1 |
17.6±8.6 |
20.6±9.1 |
0.151 |
|
Postoperative |
17.2±8.3 |
16.3±8.9 |
20.9±9.9 |
0.024 |
|
Correction |
-3.5±7.9 |
-1.3±5.9 |
0.3±7.0 |
0.171 |
|
1-year postoperative |
15.9±8.0 |
14.3±8.9 |
18.2±13.0 |
0.159 |
|
Sagittal vertical axis (mm) |
|
|
|
|
|
Preoperative |
43.8±54.2 |
54.9±66.2 |
59.4±62.2 |
0.367 |
|
Postoperative |
24.3±28.5 |
24.5±34.0 |
25.2±36.6 |
0.990 |
|
Correction |
-19.5±47.5 |
-30.5±60.4 |
-34.1±61.7 |
0.606 |
|
1-year postoperative |
16.3±37.5 |
18.0±29.1 |
37.7±40.7 |
0.012 |
Table 5.
Perioperative complications
|
ALIF (n=23) |
OLIF (n=60) |
TLIF (n=58) |
p-value |
|
Total |
11 (47.8) |
14 (23.3) |
15 (25.9) |
0.725 |
|
Urinary disturbance |
2 |
5 |
6 |
|
|
Wound infection |
1 |
1 |
2 |
|
|
Pulmonarycongestion |
1 |
3 |
|
|
|
Delirium |
1 |
|
2 |
|
|
Dermatitis |
|
1 |
2 |
|
|
Incisional hernia |
2 |
|
|
|
|
Dural tear |
1 |
1 |
|
|
|
Vascular injury |
1 |
1 |
|
|
|
Deep vein thrombosis |
1 |
|
1 |
|
|
Pseudomembranous colitis |
1 |
|
|
|
|
Ileus |
|
1 |
|
|
|
Myocardial infarction |
|
1 |
|
|
|
Asthma attack |
|
|
1 |
|
|
Urinary tract infection |
|
|
1 |
|
References
2. Chung HW, Lee HD, Jeon CH, Chung NS : Comparison of surgical outcomes between oblique lateral interbody fusion (OLIF) and anterior lumbar interbody fusion (ALIF). Clin Neurol Neurosurg 209 : 106901, 2021   3. Han SH, Hyun SJ, Jahng TA, Kim KJ : A comparative radiographic analysis of fusion rate between L4-5 and L5-S1 in a single level posterior lumbar interbody fusion. Korean J Spine 12 : 60-67, 2015    4. Hsieh PC, Koski TR, O’Shaughnessy BA, Sugrue P, Salehi S, Ondra S, et al : Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine 7 : 379-386, 2007   5. Hyun SJ, Yoon SH, Kim JH, Oh JK, Lee CH, Shin JJ, et al : A prospective, multi-center, double-blind, randomized study to evaluate the efficacy and safety of the synthetic bone graft material DBM gel with rhBMP-2 versus DBM gel used during the TLIF procedure in patients with lumbar disc disease. J Korean Neurosurg Soc 64 : 562-574, 2021     6. Jo DJ, Seo EM : Efficacy and radiographic analysis of oblique lumbar interbody fusion in treating adult spinal deformity. PLoS One 16 : e02573162021    9. Lee N, Kim KN, Yi S, Ha Y, Shin DA, Yoon DH, et al : Comparison of outcomes of anterior, posterior, and transforaminal lumbar interbody fusion surgery at a single lumbar level with degenerative spinal disease. World Neurosurg 101 : 216-226, 2017   10. Li R, Shao X, Li X, Liu Y, Jiang W : Comparison of clinical outcomes and spino-pelvic sagittal balance in degenerative lumbar spondylolisthesis: minimally invasive oblique lumbar interbody fusion (OLIF) versus transforaminal lumbar interbody fusion (TLIF). Medicine (Baltimore) 100 : e237832021   11. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ : Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1 : 2-18, 2015   12. Moses ZB, Razvi S, Oh SY, Platt A, Keegan KC, Hamati F, et al : A retrospective comparison of radiographic and clinical outcomes in single-level degenerative lumbar disease undergoing anterior versus transforaminal lumbar interbody fusion. J Spine Surg 7 : 170-180, 2021    14. Patel DV, Yoo JS, Karmarkar SS, Lamoutte EH, Singh K : Interbody options in lumbar fusion. J Spine Surg 5( Suppl 1):S19-S24, 2019    15. Phan K, Thayaparan GK, Mobbs RJ : Anterior lumbar interbody fusion versus transforaminal lumbar interbody fusion--systematic review and meta-analysis. Br J Neurosurg 29 : 705-711, 2015   16. Potter BK, Lenke LG, Kuklo TR : Prevention and management of iatrogenic flatback deformity. J Bone Joint Surg Am 86 : 1793-1808, 2004   17. Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP : Trends in lumbar spinal fusion-a literature review. J Spine Surg 6 : 752-761, 2020    18. Saadeh YS, Joseph JR, Smith BW, Kirsch MJ, Sabbagh AM, Park P : Comparison of segmental lordosis and global spinopelvic alignment after single-level lateral lumbar interbody fusion or transforaminal lumbar interbody fusion. World Neurosurg 126 : e1374-e1378, 2019   19. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V : Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 35 : 2224-2231, 2010  20. Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, et al : Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37 : 1077-1082, 2012  21. Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, et al : Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38 : E803-E812, 2013  22. Sembrano JN, Yson SC, Horazdovsky RD, Santos ER, Polly DW Jr : Radiographic comparison of lateral lumbar interbody fusion versus traditional fusion approaches: analysis of sagittal contour change. Int J Spine Surg 9 : 16, 2015    24. Villavicencio AT, Burneikiene S, Nelson EL, Bulsara KR, Favors M, Thramann J : Safety of transforaminal lumbar interbody fusion and intervertebral recombinant human bone morphogenetic protein-2. J Neurosurg Spine 3 : 436-443, 2005   25. Watkins RG 4th, Hanna R, Chang D, Watkins RG 3rd : Sagittal alignment after lumbar interbody fusion: comparing anterior, lateral, and transforaminal approaches. J Spinal Disord Tech 27 : 253-256, 2014  26. Wu PK, Wu MH, Shih CM, Lin YK, Chen KH, Pan CC, et al : Comparison of incidence of adjacent segment pathology between anterior lumbar interbody fusion and transforaminal lumbar interbody fusion treatments for lumbosacral junction. Tomography 7 : 855-865, 2021    27. Xu DS, Walker CT, Godzik J, Turner JD, Smith W, Uribe JS : Minimally invasive anterior, lateral, and oblique lumbar interbody fusion: a literature review. Ann Transl Med 6 : 104, 2018   
|
|