Yang, Cho, Kang, and Choi: Neuralgic Amyotrophy Manifesting as Mimicking Posterior Interosseous Nerve Palsy
Abstract
The upper trunk of the brachial plexus is the most common area affected by neuralgic amyotrophy (NA), and paresis of the shoulder girdle muscle is the most prevalent manifestation. Posterior interosseous nerve palsy is a rare presentation in patients with NA. It results in dropped finger on the affected side and may be misdiagnosed as entrapment syndrome or compressive neuropathy. We report an unusual case of NA manifested as PIN palsy and suggest that knowledge of clinical NA phenotypes is crucial for early diagnosis of peripheral nerve palsies.
Key Words: Neuralgic amyotrophy В· Brachial plexus neuritis В· Posterior interosseous nerve В· Entrapment syndrome В· Magnetic resonance neurography.
INTRODUCTION
Though the precise mechanism of neuralgic amyotrophy (NA) remains unknown, it is thought that the brachial plexus or its branches may develop idiopathic inflammation in response to intrinsic or extrinsic conditions, leading to extreme pain at symptom onset and rapid paresis of the upper extremity muscle. In two-thirds of patients with NA, the upper trunk of the brachial plexus is most affected, but any part of peripheral nerve can be involved 9,10). There are few reports of lower trunk involvement; Yu et al. 11) reported three cases of lower trunk plexopathy in 10 patients with NA confirmed by neurophysiologic study, and their initial presentations on admission were ulnar nerve palsies after shoulder pain. The posterior interosseous nerve (PIN) innervates the muscles on the radial side and dorsal surface of the forearm muscle to facilitate finger extension without sensory distribution. Idiopathic PIN palsies are common, but can also be caused by direct injury, repeated overuse of the wrist joint and forearm muscles, or tumors with mass effect 1,24). Here, we describe a case of NA presented with PIN palsy that was treated with medicines and physiotherapy.
CASE REPORT
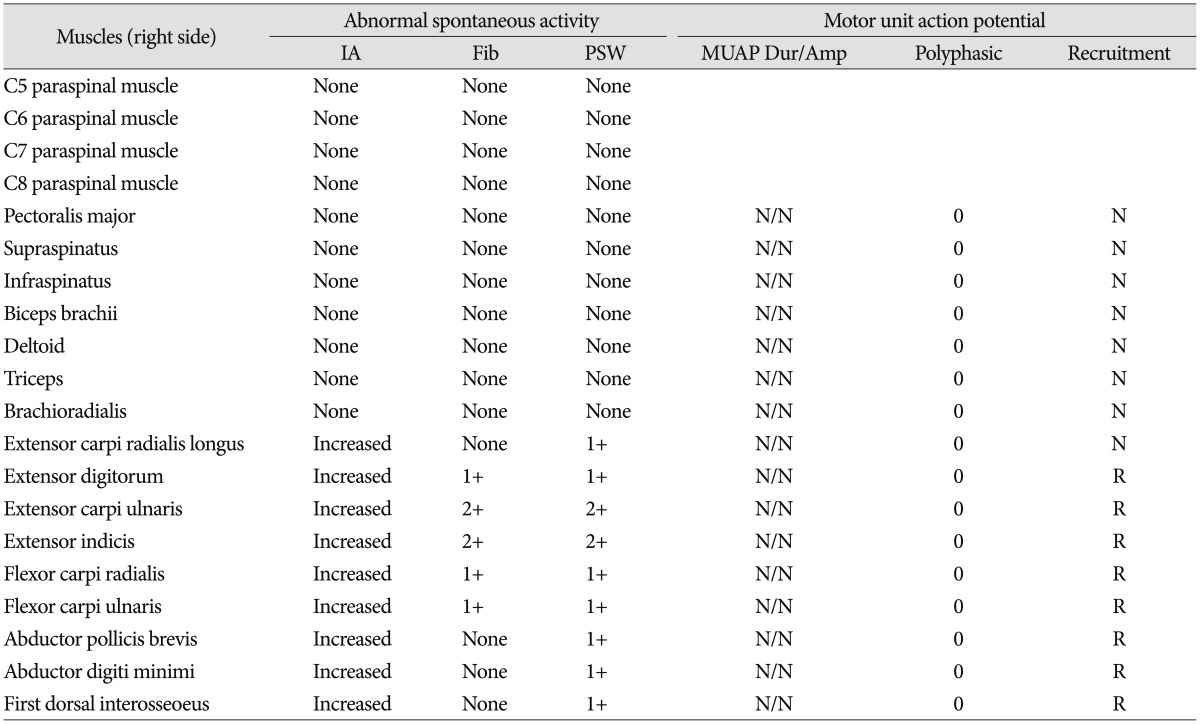
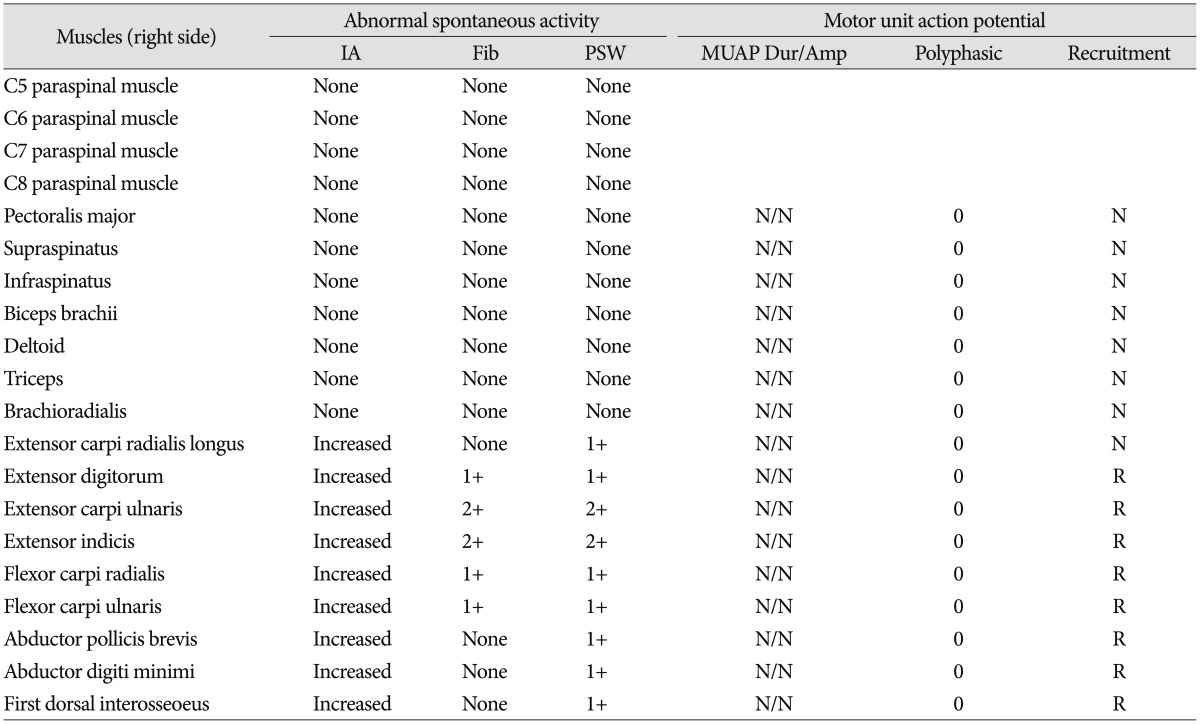
A 53-year old male manual worker presented with right finger extensor muscle paresis. One week prior to presentation, he had experienced severe right neck and shoulder pain that disturbed his sleep. He was initially diagnosed with a herniated cervical disk in a primary clinic, and he experienced intolerable pain that was not easily controlled with analgesics or physiotherapy. After 5 days, the severe pain remitted, but the patient suddenly developed right finger drop. On admission, neurological examination revealed right wrist extension weakness (G4/5), finger extension weakness (Gr1/5), and hand grasp weakness (Gr4/5), but the patient did not exhibit abnormal sensory changes or tenderness on his affected forearm and hand( Fig. 1). Magnetic resonance (MR) imaging demonstrated a cervical spondylosis incompatible with his clinical presentation, and MR neurography (MRN) demonstrated diffuse thickening in the right C6 nerve root with increased signal intensity ( Fig. 2). A neurophysiological examination was performed on 17 days after the initial symptom of pain. Results of nerve conduction studies of the right median, radial, ulnar nerves were normal. Electromyography (EMG) showed signs of abnormal spontaneous activity in the right extensor carpi radialis longus, extensor digitorum, extensor carpi ulnaris, extensor indicis, flexor carpi radialis, flexor carpi ulnaris, abductor digiti minimi, abductor pollicis brevis and first dorsal interosseous with reduced motor unit action potential (MUAP) recruitment ( Table 1). Electrodiagnostic studies revealed a pattern of plexopathy not readily localizable to one or more specific trunks, divisions, cords, or peripheral nerves. He was diagnosed with NA mainly on the lower trunk of brachial plexus and was managed with active physiotherapy. Two months later, his finger extension weakness was improved (Gr3/5), and follow-up EMG revealed improvement of MUAP recruitment for his finger extensor muscles.
DISCUSSION
PIN palsy may develop due to acute trauma, masses compressing the nerve, or structural compression of the nerve at the arcade of Frohse 1,25), and it leads to weak finger extension with a wrist deviation on the radial side. True neurogenic PIN palsy is not usually accompanied by pain or tenderness. Rosenbaum et al. 6) examined PIN syndrome in previous studies and reported that posterior interosseous neuropathy and NA are often confused with causes of forearm pain. They found that all patients had objective weakness limited to PIN-innervated muscles with or without mild forearm discomfort 6). The present patient experienced intolerable pain in his right neck and shoulder 1 week before paresis developed. Although severe pain remitted on the sixth day, abrupt finger drop spontaneously emerged on that side. Hashizume et al. 4) reported that four of 31 non-traumatic PIN palsy patients exhibited axonal interruption of the brachioradialis muscle on EMG who had experienced acute onset of pain followed by rapid development of paresis. They recommended full examination of these patients to identify additional paralysis to differentiate between posterior interosseous neuropathy and NA. Though MRN is known for an early diagnostic method of NA 3,11), MRN does not reveal an involvement of the trunk, but also C6 spinal nerve incompatible with clinical presentations. MRN has an advantage for diagnosing with NA in acute phase, when it is not appropriate to get a positive result by neurophysiologic study. However, this method does not always show all pathologic lesions of inflamed nerves because of the differences of their severity or technical error 11). Over 90% of patients with NA presents with acute, severe pain in the upper extremities. The pain is typically constant, but is often worse at night, with most patients reporting pain scores over 7 on a numerical rating scale of 0-10. After the initial pain disappears or improves, NA usually presents as involvement of the upper brachial plexus with weakness of the peri-scapular and pray-glenohumeral muscles, including the infraspinatus, supraspinatus, Serratus anterior, and deltoid 10). NA has a complex etiology, and the pathophysiological feature of the upper trunk of the brachial plexus being mostly affected is still un-clear. Alfen et al. suggested that the predilection of NA to affect the brachial plexus is mediated by wear-and-tear-induced weakening of the blood-nerve-barrier that normally prevents immune factors from accessing the peripheral nerve system; this is especially true of the upper trunk that is highly involved in shoulder movement 10). In this patient, EMG indicated that the median and ulnar nerves were also involved, but the PIN-innervated muscles were severely damaged. Therefore, if a physician is not aware of the clinical characteristic of NA which are episodic pain attack and subsequent weakness of rapid onset with muscle atropy 7,10), they might perform unnecessary studies and misdiagnose the patient with herniated cervical disk, PIN syndrome or other musculoskeletal problems. Though there has been anecdotal evidence that corticosteroids can have a good effect on pain and recovery, there were no randomized clinical trial studies to validate the effects of this treatment 9). Tsairis et al. 8)reported that early administration of steroids did not alter the course of the disease and only a few patients reported pain relief. Similar to previously reported favorable outcomes for NA 6,910), this patient recovered from paresis following conservative treatments.
CONCLUSION
Mimicking complete PIN palsy is a rare presentation of NA. Although unusual, an awareness of clinical characteristics of NA may help clinicians make correct diagnoses and help them avoid inappropriate and unnecessary evaluations when assessing patients with peripheral nerve palsy.
Acknowledgements
This study was supported by BioGreen 21 Program (PJ01121401) of Rural Development Administration.
References
1. Avram R, Hynes NM : Posterior interosseous nerve compression secondary to a parosteal lipoma : case report and literature review. Can J Plast Surg 2004, 12 : 69-72,    2. Derkash RS, Niebauer JJ : Entrapment of the posterior interosseous nerve by a fibrous band in the dorsal edge of the supinator muscle and erosion of a groove in the proximal radius. J Hand Surg Am 1981, 6 : 524-526,   3. Duman I, Guvenc I, Kalyon TA : Neuralgic amyotrophy, diagnosed with magnetic resonance neurography in acute stage : a case report and review of the literature. Neurologist 2007, 13 : 219-221,   4. Hashizume H, Nishida K, Nanba Y, Shigeyama Y, Inoue H, Morito Y : Non-traumatic paralysis of the posterior interosseous nerve. J Bone Joint Surg Br 1996, 78 : 771-776,   5. Jou IM, Wang HN, Wang PH, Yong IS, Su WR : Compression of the radial nerve at the elbow by a ganglion : two case reports. J Med Case Rep 2009, 3 : 7258,    6. Rosenbaum R : Disputed radial tunnel syndrome. Muscle Nerve 1999, 22 : 960-967,   7. Tjoumakaris FP, Anakwenze OA, Kancherla V, Pulos N : Neuralgic amyotrophy (Parsonage-Turner syndrome). J Am Acad Orthop Surg 2012, 20 : 443-449,   8. Tsairis P, Dyck PJ, Mulder DW : Natural history of brachial plexus neuropathy. Report on 99 patients. Arch Neurol 1972, 27 : 109-117,   9. van Alfen N : Clinical and pathophysiological concepts of neuralgic amyotrophy. Nat Rev Neurol 2011, 7 : 315-322,   10. van Alfen N, van Engelen BG : The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain 2006, 129( Pt 2):438-450,   11. Yu DK, Cho YJ, Heo DH, Hong MS, Park SH : Neuroradiologic and neurophysiologic findings of neuralgic amyotrophy. J Korean Neurosurg Soc 2010, 48 : 423-428,   
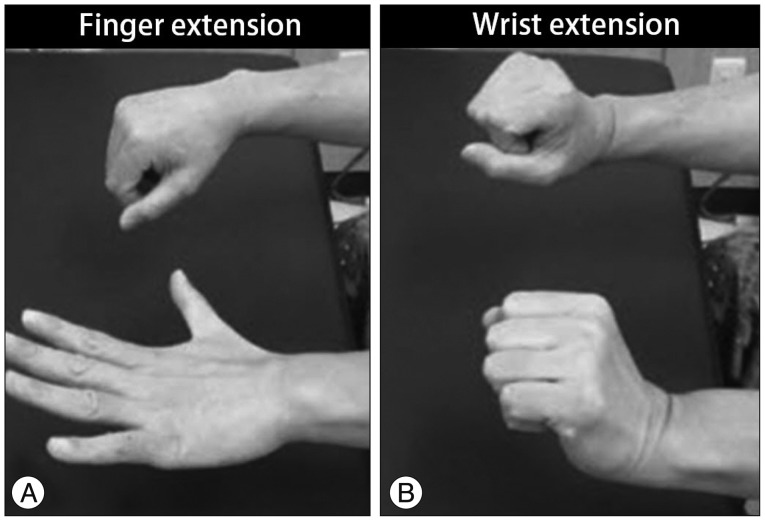
Fig.В 1
On physical examination, the patient showed a complete finger drop (A) with sparing of wrist extension (B) on right side.
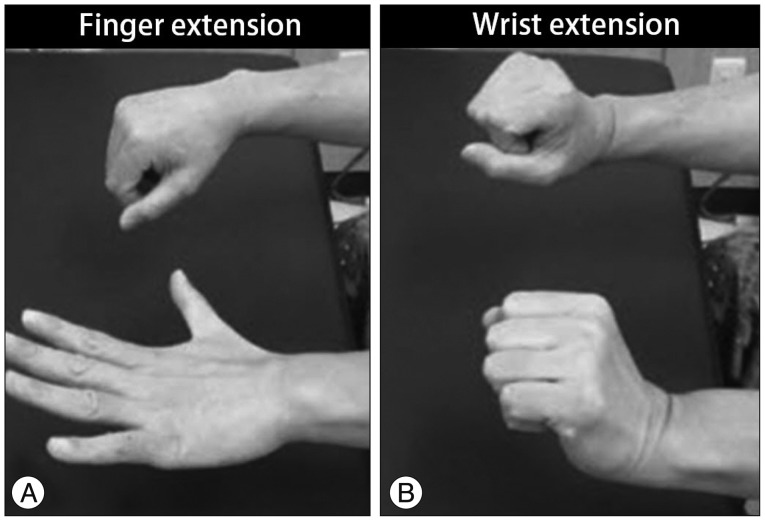
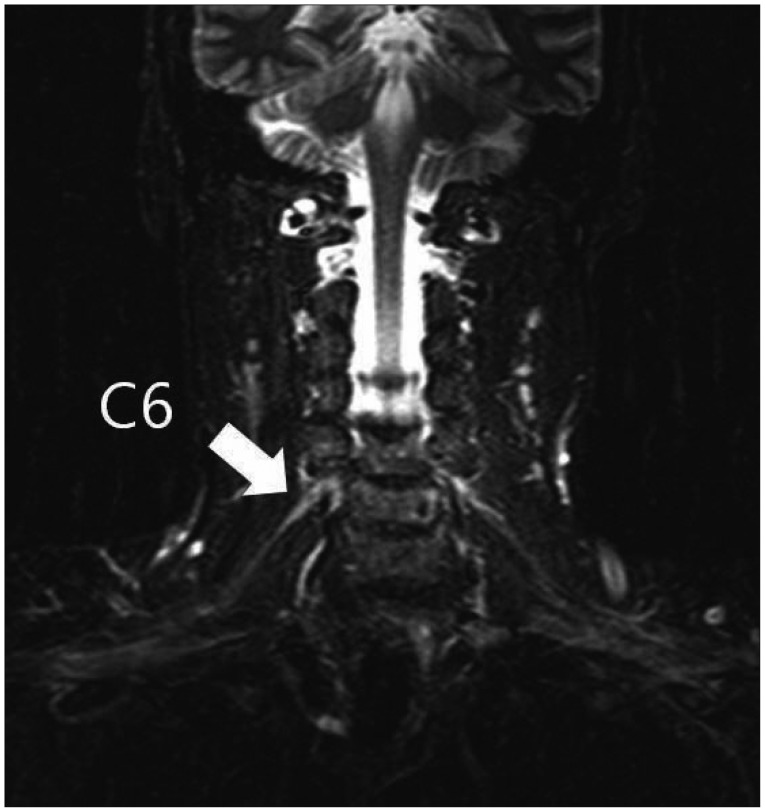
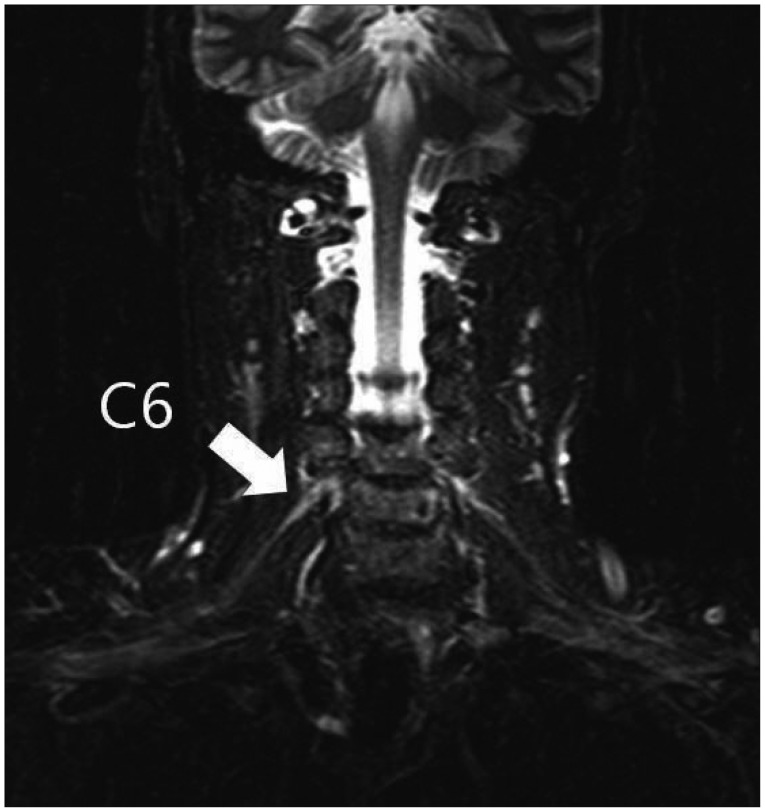
Fig.В 2
Coronal short tau inversion recovery imaging at TR/TE 50000/52 demonstrated a thickening and increased signal intensity in the right C6 root of the brachial plexus (white arrow).
TableВ 1
Initial electrophysiologic study in the right upper extremity
|
|