Kim, Sohn, Hong, Chang, Lee, and Kim: The Effectiveness of Additional Treatment Modalities after the Failure of Recanalization by Thrombectomy Alone in Acute Vertebrobasilar Arterial Occlusion
Abstract
Objective
Acute vertebrobasilar artery occlusion (AVBAO) is a devastating disease with a high mortality rate. One of the most important factors affecting favorable clinical outcome is early recanalization. Mechanical thrombectomy is an emerging treatment strategy for achieving a high recanalization rates. However, thrombectomy alone can be insufficient to complete recanalization, especially for acute stroke involving large artery atheromatous disease. The purpose of this study is to investigate the safety and efficacy of mechanical thrombectomy in AVBAO.
Methods
Fourteen consecutive patients with AVBAO were treated with mechanical thrombectomy. Additional multimodal treatments were intra-arterial (IA) thrombolysis, balloon angioplasty, or permanent stent placement. Recanalization by thrombectomy alone and multimodal treatments were assessed by the Thrombolysis in Cerebral Infarction (TICI) score. Clinical outcome was determined using the National Institutes of Health Stroke Scale (NIHSS) at 7 days and the modified Rankin Scale (mRS) at 3 months.
Results
Thrombectomy alone and multimodal treatments were performed in 10 patients (71.4%) and 4 patients (28.6%), respectively. Successful recanalization (TICI 2b-3) was achieved in 11 (78.6%). Among these 11 patients, 3 (27.3%) underwent multimodal treatment due to underlying atherosclerotic stenosis. Ten (71.4%) of the 14 showed NIHSS score improvement of >10. Overall mortality was 3 (21.4%) of 14.
Conclusion
We suggest that mechanical thrombectomy is safe and effective for improving recanalization rates in AVBAO, with low complication rates. Also, in carefully selected patients after the failure of recanalization by thrombectomy alone, additional multimodal treatment such as IA thrombolysis, balloons, or stents can be needed to achieve successful recanalization.
Key Words: Vertebrobasilar artery occlusion ┬Ę Mechanical thrombectomy ┬Ę Multimodal treatment.
INTRODUCTION
Acute vertebrobasilar artery occlusion (AVBAO) is generally accepted to have a dismal prognosis 3,510). One of the most important factors affecting favorable clinical outcome in AVBAO is early recanalization 10,1314,15). Intravenous or intra-arterial (IA) thrombolytic agents showed poor outcomes in accomplishing successful recanalization in AVBAO 14,2223,2526,27). Recently, however, endovascular mechanical thrombectomy (MT) devices such as stent retrievers or suction thrombectomy with reperfusion catheters have opened a new era of treatment for successful recanalization in AVBAO 7,916,1719,2024). Also, the result of mechanical recanalization in basilar artery occlusion in the Endovascular Stroke Treatment (ENDOSTROKE) study was published in this year 28). For achieving successful recanalization, multimodal treatments using IA thrombolysis, percutaneous balloon angioplasty (PTA), or stenting regardless of intravenous thrombolytic agent, can be necessary. If recanalization is not achieved after thrombectomy, several causes may be considered : 1) focal underlying atherosclerotic stenosis, 2) large amount of thrombus, or 3) thrombus with long segment intracranial stenosis. Based on the cause of failed thrombectomy alone, we selected various treatment modalities.
This study aimed to investigate the effectiveness of additional treatment modalities after the failure of recanalization by thrombectomy alone in AVBAO.
MATERIALS AND METHODS
Patient populations
Data for all patients with acute stroke who underwent endovascular treatment were prospectively collected from our stroke data base registry. We retrospectively analyzed clinical and angiographic results for patients presenting with acute ischemic stroke with vertebrobasilar artery occlusion and treated with thrombectomy, retrievable stents, or suction thrombectomy with a reperfusion catheter between October 2013 and June 2015.
All patients who presented to the emergency room in our institution were evaluated by two stroke neurologists and assigned a National Institutes of Health Stroke Scale (NIHSS) score. Urgent brain non-contrast computed tomography (CT) with CT angiography, or stroke magnetic resonance imaging (MRI) with diffusion weighted imaging (DWI) and time-of-flight MR angiography, were performed in all patients. For endovascular thrombectomy, our inclusion criteria were as follows : 1) baseline NIHSS score of Ōēź6, 2) evidence of AVBAO on CT or MR angiography, 3) imaging findings consistent with clinical symptoms, and 4) symptom duration after stroke onset <24 hours. The exclusion criteria were : 1) intracerebral hemorrhage on CT or MRI, 2) established large brainstem or cerebellar infarction on non-contrast CT, 3) previous occlusion of another intracranial vessel, or 4) life expectancy of <3 months. Informed consent was obtained from patients or their relatives.
Intravenous thrombolysis with recombinant tissue plasminogen activator (rtPA) (0.6 mg/kg) was administered as bridging therapy in patients with no contraindication.
Endovascular therapies
For all patients, the IA thrombectomy procedure was performed under monitored anesthesia care using intravenous dexmedetomidine (Precedex®). No antiplatelet drugs or intravenous anticoagulants were administered, except for mixed heparin in the flushing system during the procedure.
A 7 Fr sheath was placed in the femoral artery, and diagnostic angiography was performed to identify the dominant and more easily accessible vertebral artery (VA) to the occlusion site. The clot occlusion site was divided into the VA; proximal, middle, or distal segment of the basilar artery (BA); or proximal posterior cerebral artery (PCA). A 6 Fr guiding catheter system (Chaperon, Microvention, Tustin, CA, USA) was introduced and placed in the distal cervical segment of the dominant VA.
Solitaire FR (Covidien, Dublin, Ireland) or Penumbra reperfusion catheters (Hutem, Alameda, CA, USA) were used for mechanical thrombectomy. Using the Solitaire FR device, a Rebar-18 microcatheter (EV3, Irvine, CA, USA) was carefully placed to at least 1 cm beyond the distal extent of the clot. We tried that the thrombus was placed within the center of the total length of a retrievable stent. Because of the absence of a stent strut to the distal 10 mm of the proximal stent marker, the proximal end of the thrombus was placed in more distal side of distal 10 mm of the proximal stent marker; the stent was deployed completely by pulling back the microcatheter nearly proximal to the proximal stent marker. Angiography was then performed to confirm restoration of immediate flow for adequate stent placement. From deployment to pull-back of the stent, about 5 minutes was allowed for the thrombus formation to be embedded within the stent. 4) Before stent retrieval, the microcatheter was advanced to partially resheath the proximal connection site of the stent to the pusher wire to minimize breakage between the stent and pusher wire. 18) The Solitaire FR stent and microcatheter were pulled back simultaneously during blood aspiration with a 50 cc syringe in the guiding catheter to minimize distal emboli, because of the absence of an available balloon-guided catheter. If occlusion persisted or if there was incomplete recanalization of the vessel, the microcatheter and stent were cleaned and reinserted for repeat thrombectomy. Control angiograms were performed after each thrombectomy attempt to evaluate the recanalization and distal emboli in previously unaffected vascular territory. Using a penumbra reperfusion catheter, we placed the catheter just proximal to the clot occlusion site, and applied negative pressure at the proximal tip by continuous aspiration with a 50 cc syringe. The catheter was then carefully pulled back. We defined the difficult case in no successful recanalization despite 3 times mechanical thrombectomy. Next, we applied the additional treatment modalities in this situation.
If there was suspicion of underlying atherosclerotic stenosis, IA tirofiban (Aggrastat®) (0.5-1.5 mg) was infused through the microcatheter just proximal to the occlusion site. For balloon angioplasty, a Gateway® PTA balloon (Stryker Neurovascular, Fremont, CA, USA) was advanced and inflated very carefully using a 0.014-inch exchange microwire (Transend, Stryker Neurovascular, Natick, MA, USA). The balloon was carefully inflated to nearly 80-90% of normal distal vessel diameter. In permanent stent deployment, postprocedure aspirin 300 mg/day was initiated after 24 hours.
In the absence of successful recanalization despite 3 times thrombectomy alone, we considered two situations : 1) repetitive reocclusion after recanalization, or 2) failed first recanalization despite various multimodal methods. In the event of repetitive reocclusion after recanalization, we assumed underlying atherosclerotic stenosis and treated serially with PTA with/without permanent stenting after IA tirofiban infusion (0.5-1.5 mg).
Clinical and angiographic outcome measurements
The recanalization extent was classified according to the TICI grading scale. TICI grades 2b and 3 were rated as successful recanalization, whereas TICI grades 0 to 2a were rated as unsuccessful 11). After the endovascular procedure, all patients were observed in the intensive stroke unit for about 24 hours. Postprocedure routine follow-up at 24 hours and 7 days was performed with CT or MRI. Postprocedure routine and NIHSS and modified Rankin Scale (mRS) scores were assessed by an advanced practice nurse in the stroke unit until discharge; 3-month scores were obtained by telephone follow-up or an outpatient visit by a nurse practitioner. Clinical data for this study included age, gender, hypertension, diabetes mellitus (DM), smoking, hyperlipidemia, cardiac disease, stroke subtype according to the Trial of Org 10172 in Acute Stroke Treatment (TOAST) classification 1), intravenous rtPA use, time from symptom onset to groin puncture, and initial NIHSS scores. Additional angiographic data included occluded vessel site, type of IA thrombectomy device, number of attempts at thrombectomy, type of additional treatment, such as IA thrombolytic agent, balloon, or stent, and time from groin puncture to recanalization (TGR). The outcomes were measured according to postprocedure TICI grade, NIHSS scores at 7 days, and mRS scores at 3 months. A favorable outcome was defined as an mRS score Ōēż2 at 3 months and improvement of Ōēź10 or Ōēż6 points in the NIHSS score. When postprocedure intracerebral hemorrhage occurred, hemorrhage with a decline of Ōēź4 points in the NIHSS score was defined as symptomatic.
Statistical analysis
Statistical analysis was performed with commercial software (SPSS, version 15.0, SPSS Inc., Chicago, IL, USA). The descriptive analysis for data was presented as mean┬▒standard deviation. Fisher's exact test was used for the statistical analysis of 1) the independent variables (hypertension, DM, smoking, hyperlipidemia, cardiac disease, recent ischemic stroke, and TOAST classification) affecting the treatment modality (thrombectomy alone vs. multimodal treatment), 2) 7-day and 3-month clinical outcome according to arterial recanalization, and 3) 7-day and 3-month clinical outcome according to the type of treatment modality. A p-value less than 0.05 was considered significant.
RESULTS
Between October 2013 and June 2015, there were total 109 patients with acute ischemic stroke treated with mechanical thrombectomy in our institute. Among them, 16 (14.7%) patients with AVBAO were treated with MT in our institution. Two patients were excluded from our study. One patient had previous occlusion of another intracranial vessel. The other patient had failure of advancement of the microcatheter in the VA. The remaining 14 patients (12.8%) underwent MT. Intravenous rtPA was administered in 5 patients (35.7%) because of symptom duration <4.5 hours. We analyzed the clinical and angiographic outcomes in 14 patients with AVBAO.
Patient characteristics
Six patients were men and eight were women. The median age was 71.4┬▒2.4 years (49-83). Among risk factors, 78.6% had hypertension, 64.3% had cardiac disease, 57.1% had atrial fibrillation, 28.6% had DM, 21.4% had hyperlipidemia, 21.4% had previous transient ischemic attack (TIA) or stroke, and 7.1% smoked. The stroke etiology according to TOAST classification was cardioembolic (CE) in 10 (71.4%) and large artery atheroma (LAA) in 4 (28.6%). Median NIHSS score was 20.0 (9-25). Five (35.7%) of 14 patients underwent intravenous rtPA as bridging therapy before MT, with a median dose of 25.5┬▒16.0 mg (4-30).
The occluded site was the distal BA in 6 (42.9%), distal BA with both posterior cerebral arteries in 1 (7.1%), distal BA with VA in 2 (14.3%), middle BA in 4 (28.6%), and proximal BA with distal basilar and VA in 1 (7.1%).
Median time from symptom onset to groin puncture was 221.0┬▒ 219.7 min (24-817). Median time from groin puncture to recanalization was 23.0┬▒14.5 min (10-60). Twelve patients were treated with Solitaire FR and 2 with Penumbra reperfusion catheters. The median number of passes for Solitaire FR or Penumbra reperfusion catheters was 2.57.
Initial TICI score before recanalization was 0 in 13 patients (92.9%) and 1 in 1 patient (7.1%). Final successful (TICI score 2b or 3) or unsuccessful recanalization (TICI score 0 or 2a) was achieved in 11 (78.6%) patients and 3 (21.4%) patients, respectively.
Thrombectomy alone vs. additional multimodal treatment
Ten patients (71.4%) were treated with thrombectomy alone and 4 (28.6%) with multimodal treatment.
In 9 patients with distal BA occlusion, according to the location of occluded vessel, there were successful recanalization using thrombectomy alone in 6 patients (66.7%) and additional treatment modalities in 2 (22.2%), respectively. Unfortunately, one patient (11.1%) underwent no recanalization. In 2 patients treated with additional treatment modalities, the location of occluded vessel were distal BA and VA occlusion (No. 10 and 11). Although successful recanalization of the distal basilar and VA occlusion was performed, repetitive reocclusion after recanalization of the VA occurred. Because of reocclusion after recanalization despite 3 attempts at thrombectomy, we tried IA thrombolysis (IAT) with 1.0 mg tirofiban, and IAT with 1.5 mg tirofiban with balloon angioplasty, respectively, due to underlying atherosclerotic stenosis of the intracranial VA.
In 3 patients with middle BA occlusion, there were successful recanalization using thrombectomy alone in 2 (66.7%) patients and additional treatment modalities in 1 (33.3%), respectively. In one patient treated with additional treatment modalities, reocclusion after recanalization occurred despite several thrombectomy plus IAT attempts with 1.0 mg tirofiban. Because of underlying tight atherosclerotic stenosis of the middle BA, balloon angioplasty after Solitaire stenting was performed. For the in-stent thrombosis, additional IAT with 1.0 mg tirofiban (total 2.0 mg) was administered. Successful recanalization was achieved.
Unfortunately, in 2 patients including proximal BA occlusion, there were no successful recanalization. A schematic diagram of treatment modalities and grade of recanalization according to the location of the occluded vessel is shown in Fig. 1. There were no fatal complications such as vascular rupture or symptomatic intracerebral hemorrhage. There were distal emboli in the right PCA during the procedure in one patient (No. 2) and asymptomatic subarachnoid hemorrhage in the peripontine cistern (No. 5). These two patients had no neurological deficits.
Median initial NIHSS score was 19.5. Ten patients (71.4%) of the 14 patients experienced NIHSS score improvement of Ōēź10 or Ōēż6 points at 7 days. One patient showed a poor outcome at 7 days. Median NIHSS score at 7 days was 4.4┬▒7.4 points. The mRS score at 3 months was 0-2 in 7 (50%) of 14 patients, and 3-5 in 4 patients (28.6%), and the remaining 3 patients (21.4%) without recanalization died. Clinical and angiographic characteristics in AVBAO patients treated with thrombectomy are summarized in Table 1.
Analysis of variable factors affecting outcome
As noted above, we classified the 2 groups into thrombectomy alone and multimodal treatment. According to variables such as hypertension, DM, smoking, hyperlipidemia, atrial fibrillation, cardiac disease, previous TIA or stroke, and TOAST classification, we compared the thrombectomy alone vs. multimodal treatment groups. In 10 patients with thrombectomy alone, 9 (90%) were classified as having CE. In 4 patients with multimodal treatment, 3 (75%) showed a statistically significant correlation between TOAST classification and multimodal treatment (p<0.05). Except for the TOAST classification, there were no statistically significant correlations between other variables and treatment modalities (p>0.05).
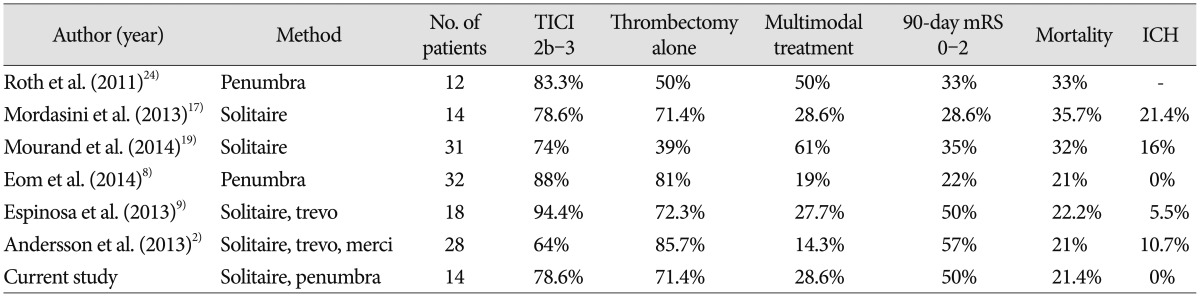
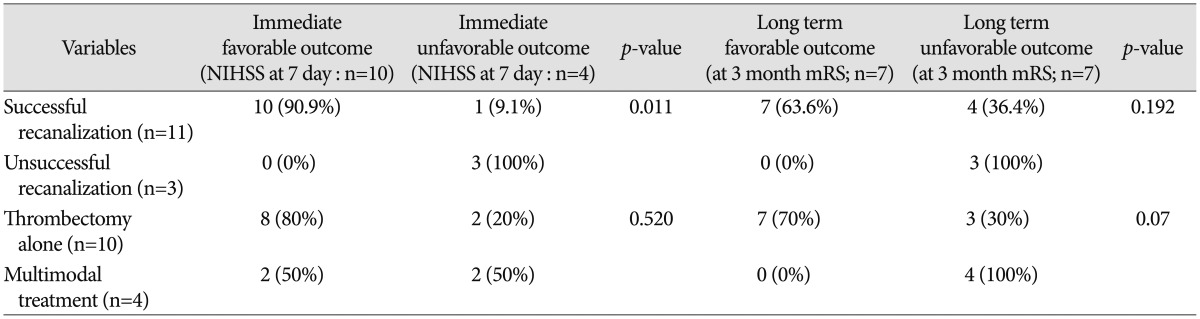
In 11 patients with successful recanalization, 10 had immediate favorable outcomes (NIHSS score improvement of Ōēź10 or Ōēż6 points at 7 days). There was a statistically significant correlation between successful recanalization and immediate favorable outcome ( p<0.05). Although there was no correlation between recanalization and mRS score at 3 months, unsuccessful recanalization showed a trend toward poor outcomes ( Table 2). Moreover, in 10 patients treated with thrombectomy alone, 8 (80%) and 7 (70%) had 7-day and 3-month favorable outcomes, respectively. In 4 patients who underwent multimodal treatment, 2 (50%) and 4 (100%) had 7-day and 3-month unfavorable outcomes, respectively.
DISCUSSION
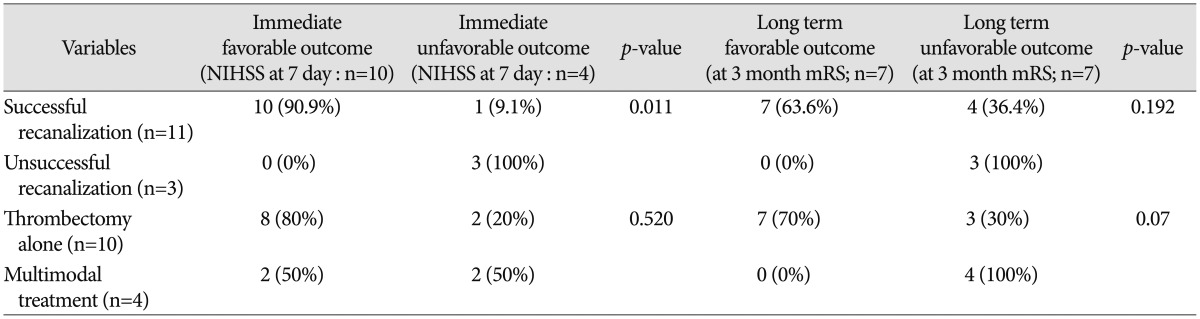
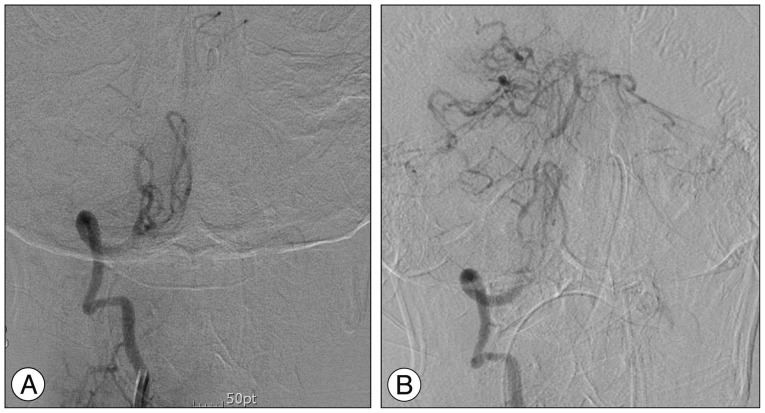
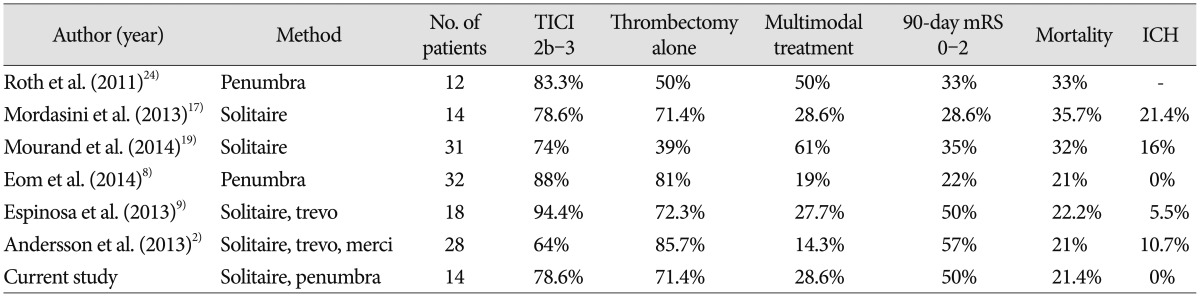
Since the MT device was first used, stent retrievers or reperfusion catheters have introduced a new strategy for treating large intracranial vessel occlusions, and achieving higher recanalization rates and better clinical outcomes than previous treatments 2,67,815,1722,24). However, compared with anterior circulation (internal carotid artery and middle cerebral artery occlusion) stroke, there have been few reports about results in AVBAO. Accordingly, detailed investigations on treatment methods and outcomes of thrombectomy in AVBAO are reported in this study. In a recent study on the effect of thrombectomy in AVBAO 2,89,1719,24), successful recanalization rates and 90-day mRS scores (0-2) were 64-94.4% and 22-57%, respectively. In a review of several published reports on recanalization and outcomes in patients with AVBAO treated with thrombectomy, treatment methods and the percentages of final successful recanalization (TICI 2-3) are usually described. Thus, we focused on additional treatment methods for achieving successful recanalization after the failure of thrombectomy alone, and the causes of failure after thrombectomy alone in AVBAO. Espinosa de Rueda et al. 9) reported that definitive post-clot-retrieval intracranial stents were used in 5 patients (27.7%) due to atherosclerotic intracranial stenosis. In addition, Mordasini et al. 17) reported that 4 (28.6%) of 14 patients underwent insufficient recanalization after thrombectomy alone was due to underlying atherosclerotic stenosis. Additional deployment of a permanent intracranial stent was achieved in 3 patients (21.4%) and percutaneous transluminal angioplasty (7.1%) in 1 patient. In our study, except for 1 patient (7.1%) with failed recanalization after pre-balloon angioplasty and repeated thrombectomy, 3 patients (21.4%) treated with additional treatment modalities in the repetitive reocclusion after recanalization underwent successful recanalization; IA tirofiban infusion after thrombectomy was performed in 1 patient, IA tirofiban infusion plus balloon angioplasty in 1, and IA tirofiban infusion plus post-balloon angioplasty after stenting in 1. Atherothrombotic occlusion in the presence of underlying intracranial stenosis can make successful recanalization more difficult. Mordasini et al. 17) suggested several causes : 1) more adhesive thrombus occurring on the surface of ulcerated atherosclerotic plaques than embolic thrombi, 2) a higher risk of reocclusion after partial recanalization by stent retrieval on the basis of a high-grade atherothrombotic lesion, and 3) insufficient radial outward force during temporary deployment to overcome a high-grade atherosclerotic stenosis. Additionally, thrombectomy can induce endothelial injury and thrombus formation at the site of atherosclerotic ulcerative plaque. This endothelial damage after Solitaire thrombectomy was reported in an animal study. 21) In our study, 3 (75%) of 4 patients who underwent multimodal treatments had LAA in stroke etiology according to the TOAST classification ( p<0.05). These 3 patients with multimodal treatments had repetitive reocclusion after transient recanalization by thrombectomy alone; therefore, we suggested that there was underlying intracranial stenosis in the occluded vessel sites. For overcoming repetitive reocclusion by thrombectomy alone in lesions involving intracranial stenosis, it can be helpful to use IA thrombolytic agents, balloon angioplasty, or permanent stent placement. In 3 patients with failed recanalization despite multimodal treatment, the cause was large thrombus burden in 2 patients (No. 3 and 7) and long segment intra-luminal narrowing in 1 (No. 6) ( Fig. 2). Although patients with failed recanalization are much decreased in number since the introduction of MT devices, failed recanalization is possible because of underlying long segment severe intracranial stenosis. Because of the risk of vascular rupture, a procedure may be terminated after one trial of thrombectomy. According to thrombectomy alone vs. additional multimodal treatment, we reviewed published reports with AVBAO treated with thrombectomy ( Table 3). In this study, we report the effectiveness of treatment in 14 AVBAO patients in our institution with thrombectomy. Successful recanalization rate of our study is 78.6%, this rate is comparable with that of other studies. We performed the additional multimodal treatment in 4 patients (28.6%) compared with 61% in Mourand et al. 19), 28.6% in Mordasini et al. 17), and 27.7% in Espinosa et al. 9) These findings mean that thrombectomy alone maybe not sufficient to recanalize the occluded vessel. A 90-day mRS score of 0-2 in our series was seen in 50%, compared with 57% in Andersson et al. 2), 50% in Espinosa et al. 9), 28.6% in Mordasini et al. 17), and 35% in Mourand et al. 19) We observed a mortality rate of 21.4% in our series, compared to 21% in Andersson et al., 22.2% in Espinosa et al. 9), 32% in Mourand et al. 19), and 35.7% in Mordasini et al. 17) It was reported that age, hypertension, NIHSS scores, collateral status, and the use of MRI prior to EVT predicted clinical outcome, the latter 3 remaining independent predictors in multivariate analysis. Independent predictors of recanalization were better collateral status and the use of a stent retriever 28). Because detailed additional multimodal treatment was not described well in this study, it was not included in our analysis. In the current study, there was a procedure-related complication in 1 (7.1%) patient with distal emboli during thrombectomy. There was no sign of vessel perforation or dissection. Postprocedure subarachnoid hemorrhage occurred in 1 (7.1%) patient. Fortunately, no symptomatic intracranial hemorrhage occurred according to Prolyse in Acute Cerebral Thromboembolism (PROACT) II criteria 12). This low rate of hemorrhage compares favorably with the rates of symptomatic intracranial hemorrhage reported in other studies (0-21.4%) 2,89,1719,24). This study has several limitations due to the different thrombectomy devices, retrospective analysis, single center experience, and small number of patients. Moreover, because multimodal treatment was applied due to underlying intracranial stenosis, the effect of MT alone can be unclear. There can be racial differences of underlying intracranial stenosis in vertebrobasilar arterial occlusion. Different applications of revascularization methods for intracranial stenosis may be needed in AVBAO. Large prospective, randomized trials is necessary in this aspect.
CONCLUSION
We suggest that mechanical thrombectomy is safe and effective for improving recanalization rates in AVBAO, with low complication rates. Also, in carefully selected patients after the failure of recanalization by thrombectomy alone, additional multimodal treatment such as IA thrombolysis, balloons, or stents can be needed to achieve successful recanalization.
References
1. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al : Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24 : 35-41,   2. Andersson T, Kuntze S├Čderqvist ├ģ, S├Čderman M, Holmin S, Wahlgren N, Kaijser M : Mechanical thrombectomy as the primary treatment for acute basilar artery occlusion : experience from 5 years of practice. J Neurointerv Surg 2013, 5 : 221-225,   3. Archer CR, Horenstein S : Basilar artery occlusion : clinical and radiological correlation. Stroke 1977, 8 : 383-390,   4. Brekenfeld C, Schroth G, Mordasini P, Fischer U, Mono ML, Weck A, et al : Impact of retrievable stents on acute ischemic stroke treatment. AJNR Am J Neuroradiol 2011, 32 : 1269-1273,    5. Caplan LR, Wityk RJ, Glass TA, Tapia J, Pazdera L, Chang HM, et al : New England Medical Center Posterior Circulation registry. Ann Neurol 2004, 56 : 389-398,   6. Casta├▒o C, Dorado L, Guerrero C, Mill├Īn M, Gomis M, Perez de, et al : Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation : a pilot study. Stroke 2010, 41 : 1836-1840,   7. Costalat V, Machi P, Lobotesis K, Maldonado I, Vendrell JF, Riquelme C, et al : Rescue, combined, and stand-alone thrombectomy in the management of large vessel occlusion stroke using the solitaire device : a prospective 50-patient single-center study : timing, safety, and efficacy. Stroke 2011, 42 : 1929-1935,   8. Eom YI, Hwang YH, Hong JM, Choi JW, Lim YC, Kang DH, et al : Forced arterial suction thrombectomy with the penumbra reperfusion catheter in acute basilar artery occlusion : a retrospective comparison study in 2 Korean university hospitals. AJNR Am J Neuroradiol 2014, 35 : 2354-2359,    9. Espinosa de Rueda M, Parrilla G, Zamarro J, Garc├Ła-Villalba B, Hern├Īndez F, Moreno A : Treatment of acute vertebrobasilar occlusion using thrombectomy with stent retrievers : initial experience with 18 patients. AJNR Am J Neuroradiol 2013, 34 : 1044-1048,    10. Hacke W, Zeumer H, Ferbert A, Br├╝ckmann H, del Zoppo GJ : Intra-arterial thrombolytic therapy improves outcome in patients with acute vertebrobasilar occlusive disease. Stroke 1988, 19 : 1216-1222,   11. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al : Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke 2003, 34 : e109-e137,   12. Kase CS, Furlan AJ, Wechsler LR, Higashida RT, Rowley HA, Hart RG, et al : Cerebral hemorrhage after intra-arterial thrombolysis for ischemic stroke : the PROACT II trial. Neurology 2001, 57 : 1603-1610,   13. Kim HY, Chung CS, Moon SY, Lee KH, Han SH : Complete nonvisualization of basilar artery on MR angiography in patients with vertebrobasilar ischemic stroke : favorable outcome factors. Cerebrovasc Dis 2004, 18 : 269-276,   14. Lindsberg PJ, Mattle HP : Therapy of basilar artery occlusion : a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke 2006, 37 : 922-928,   15. Lutsep HL, Rymer MM, Nesbit GM : Vertebrobasilar revascularization rates and outcomes in the MERCI and multi-MERCI trials. J Stroke Cerebrovasc Dis 2008, 17 : 55-57,   16. Miteff F, Faulder KC, Goh AC, Steinfort BS, Sue C, Harrington TJ : Mechanical thrombectomy with a self-expanding retrievable intracranial stent (Solitaire AB) : experience in 26 patients with acute cerebral artery occlusion. AJNR Am J Neuroradiol 2011, 32 : 1078-1081,    17. Mordasini P, Brekenfeld C, Byrne JV, Fischer U, Arnold M, Heldner MR, et al : Technical feasibility and application of mechanical thrombectomy with the Solitaire FR Revascularization Device in acute basilar artery occlusion. AJNR Am J Neuroradiol 2013, 34 : 159-163,    18. Mordasini P, Frabetti N, Gralla J, Schroth G, Fischer U, Arnold M, et al : In vivo evaluation of the first dedicated combined flow-restoration and mechanical thrombectomy device in a swine model of acute vessel occlusion. AJNR Am J Neuroradiol 2011, 32 : 294-300,    19. Mourand I, Machi P, Milhaud D, Picot MC, Lobotesis K, Arquizan C, et al : Mechanical thrombectomy with the Solitaire device in acute basilar artery occlusion. J Neurointerv Surg 2014, 6 : 200-204,   20. M├Čhlenbruch M, Stampfl S, Behrens L, Herweh C, Rohde S, Bendszus M, et al : Mechanical thrombectomy with stent retrievers in acute basilar artery occlusion. AJNR Am J Neuroradiol 2014, 35 : 959-964,    21. Park S, Hwang SM, Song JS, Suh DC, Lee DH : Evaluation of the Solitaire system in a canine arterial thromboembolic occlusion model : is it safe for the endothelium? Interv Neuroradiol 2013, 19 : 417-424,    22. Pfefferkorn T, Holtmannsp├Čtter M, Schmidt C, Bender A, Pfister HW, Straube A, et al : Drip, ship, and retrieve : cooperative recanalization therapy in acute basilar artery occlusion. Stroke 2010, 41 : 722-726,   23. Pfefferkorn T, Mayer TE, Opherk C, Peters N, Straube A, Pfister HW, et al : Staged escalation therapy in acute basilar artery occlusion : intravenous thrombolysis and on-demand consecutive endovascular mechanical thrombectomy : preliminary experience in 16 patients. Stroke 2008, 39 : 1496-1500,   24. Roth C, Mielke A, Siekmann R, Ferbert A : First experiences with a new device for mechanical thrombectomy in acute basilar artery occlusion. Cerebrovasc Dis 2011, 32 : 28-34,   25. Sairanen T, Strbian D, Soinne L, Silvennoinen H, Salonen O, Artto V, et al : Intravenous thrombolysis of basilar artery occlusion : predictors of recanalization and outcome. Stroke 2011, 42 : 2175-2179,   26. Sarikaya H, Arnold M, Engelter ST, Lyrer PA, Mattle HP, Georgiadis D, et al : Outcomes of intravenous thrombolysis in posterior versus anterior circulation stroke. Stroke 2011, 42 : 2498-2502,   27. Schulte-Altedorneburg G, Hamann GF, Mull M, K├╝hne D, Liebetrau M, Weber W, et al : Outcome of acute vertebrobasilar occlusions treated with intra-arterial fibrinolysis in 180 patients. AJNR Am J Neuroradiol 2006, 27 : 2042-2047,   28. Singer OC, Berkefeld J, Nolte CH, Bohner G, Haring HP, Trenkler J, et al : Mechanical recanalization in basilar artery occlusion : the ENDOSTROKE study. Ann Neurol 2015, 77 : 415-424,  
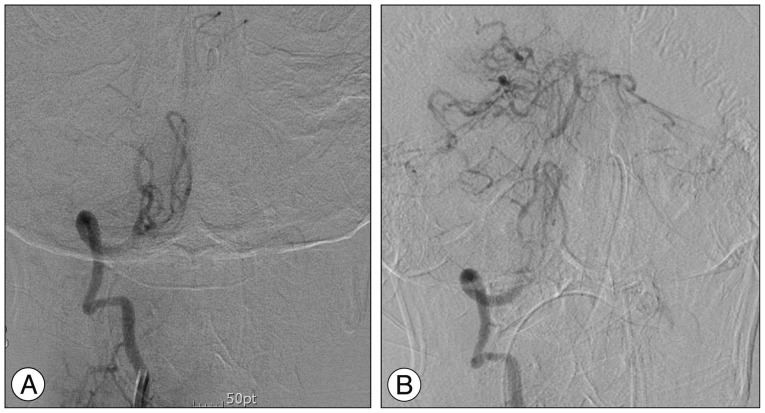
Fig.┬Ā1
Schematic diagram of treatment modalities and grade of recanalization according to the location of the occluded vessel. PCA : proximal posterior cerebral artery, VA : vertebral artery, SR : successful recanalization, BA : basilar artery, IA : intra-arterial, NR : no recanalization.

Fig.┬Ā2
(A) Preoperative angiographic finding of distal VA occlusion, (B) angiographic finding of long-segment intra-luminal narrowing of the proximal BA and distal VA segment after thrombectomy. BA : basilar artery, VA : vertebral artery.
Table┬Ā1
The summary of clinical and angiographic data of 14 patients with AVBAO treated with thrombectomy

Table┬Ā2
Grade of recanalization and treatment modalities according to clinical outcomes
Table┬Ā3
Review of published data on recanalization and outcome of patients with AVBAO treated with thrombectomy alone and multimodal treatment
|
|