INTRODUCTION
Different to a meningocele, the bulging portion of which contains only cerebrospinal fluid and overlaying dura, an encephalocele is a cystic malformation of the brain tissue herniating through bone6). Encephaloceles occur at a rate of one per 4000 live births worldwide1). Encephaloceles are classified according to their localizations in the cranium. They are often located in the occipital region; basal encephaloceles are relatively rare, constituting only 1.5% of all cases7). Encephaloceles are classified according to 5 anatomic sites, namely the spheno-ethmoidal, transsphenoidal, spheno-orbital, transethmoidal and sphenomaxillary6). Congenital absence of portions of the wings of the sphenoid leads to spheno-orbital encephalocele, a rare entity in the literature2). We wanted to share this case who had not seen any treatment until puberty and being purely congenital as being not related to trauma or neurocutaneous syndrome and also in the literature review there isn't any case like our case.
CASE REPORT
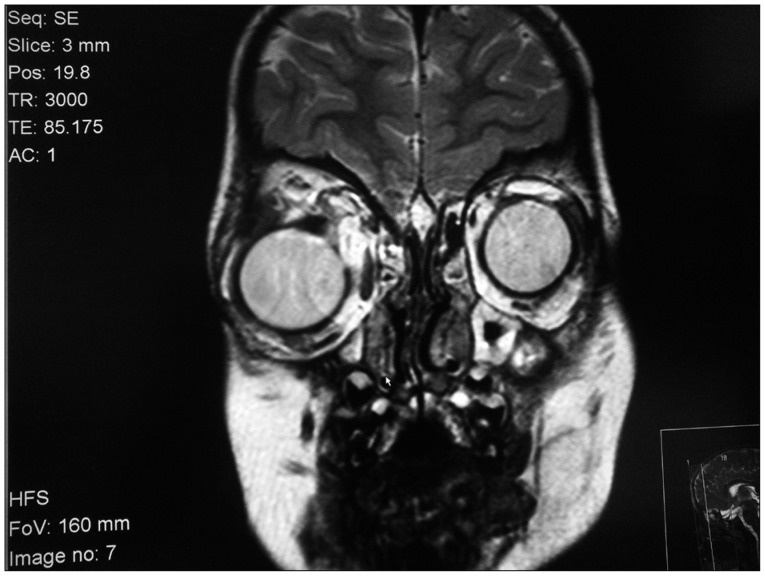
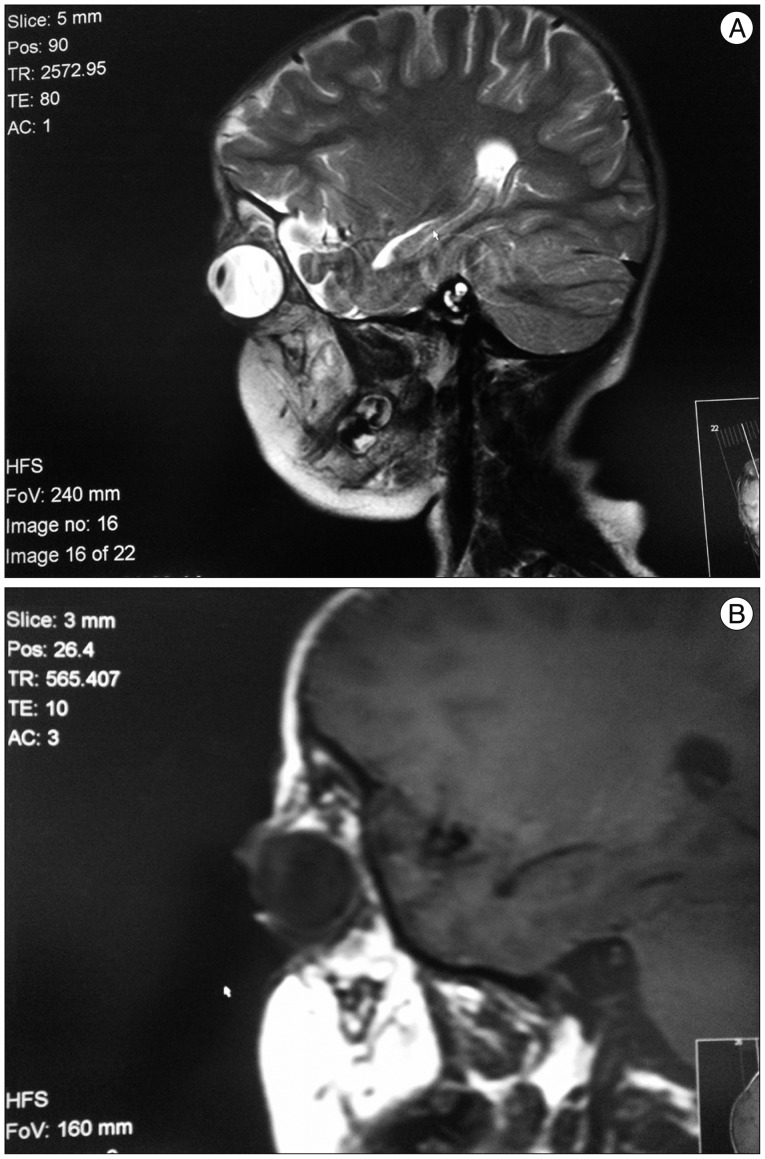
Our case was a 15-year-old female patient, who had progressive pulsatile exophthalmus and dystopia in the right eye, beginning at early age (Fig. 1). The orbital pathology was evaluated with CT scanning and MRI. At age 4, she had undergone trabeculectomy on the right eye for congenital glaucoma. She had no history of chronic disease or trauma. No congenital or acquired patch or rash was detected on her skin. There was no genetic disease in her family history. On the three-dimensional (3D) image of CT, a large hypoplasic bone defect of 20.6×30.7 mm (35.8 cm2) was observed in the superior orbital fissure of the greater wing of the right sphenoid bone (Fig. 2). On MRI, the anterior-posterior diameter of the right bulbus oculi, which measured 27.9 mm, was relatively larger than the anterior-posterior diameter of the left bulbus oculi, which measured 22 mm; the distance between the two medial canthi, which measured 33.1 mm, was increased, and the right bulbus oculi was seen to have been displaced to the inferior by 5.9 mm (Fig. 3). The right orbita was markedly exophthalmic. The T1- and T2-weighted images obtained on MRI showed the left temporal lobe, with the subarachnoid membrane extending into the orbita through the defect (Fig. 4). In studies investigating the possible presence of accompanying neurofibromatosis, no optic glioma was found. Lish nodules were not observed on ophthalmological examination. Following completion of all the examinations, surgery was recommended to the patient. Her parents were informed about the planned surgical intervention, but they didn't accept risks of the surgery, so surgery did not performed and the patient was followed up.
DISCUSSION
Encephaloceles are seen in the rate of one in every 4000 live births and defined as the protrusion of the intracranial structures1,3). Most of them occur sporadically and do not accompany to hereditary syndromes6). Encephaloceles are classified according to their intracranial localizations and basal encephaloceles are classified under 5 main headings according to their localizations including spheno-ethmoidal, trans-sphenoidal, spheno-orbital, transethmoidal and spheno-maxillary6,7). Absence of the sphenoidal wings leads to spheno-orbital encephaloceles and brain tissue and menings protrude to orbital cavity through superior orbital fissure2,6). Increased herniation due to the dural defects and the absence of the limited effect of the bone during physiologic growing of the brain and the cranium, continuous pulsation of the brain are the accepted mechanisms of the enlargement of the bone defect7). Impairment of dura is important for encephaloceles and cerebrospinal fluid (CSF) pulsation erodes the bone gradually7). The pulsation of the brain in the intraorbital field leads to the pulsation of the globe through the defect4). Although encepheloceles are one of the important causes of pulsatile exopthalmus accompanying to dystopia, they are rare in this localization and usually accompany with neurofibromatosis type 18). It is quite rare without trauma and NF 1, as in our case.
Definite diagnosis of encephalocele is made through imaging techniques5). 3D CT imaging is the first step recommended for detection of the orbital bone defect7). The greater wing of the left sphenoidal bone was hypoplastic and the left superior orbital fissure was enlarged on 3D CT examination in our case, consistently with the congenital orbital encephaloceles which does not accompany with a few syndromes in literature, although it is quite frequent. As in our case, there was the right sphenoidal wing dysplasia on 3D CT in a 22-year-old patient described by Sharma et al.8) and the patient had progressive exopthalmus since 7 years of age and the right temporal lobe was herniated to orbita1,3). MRI provides definite data about the localization of the bone defect, the content of the encephalocele and surrounding tissues (5). Continuity of the herniated tissue with brain is shown with MRI examination. In our case, the encephalocele sac contained CSF and brain tissue of the left temporal lobe on MRI. The herniated brain tissue may vary depending on the encephalocele localization. While the orbital encephalocele defined by Sharma et al.8) contained the brain tissue of the left temporal lobe, the orbital encephalocele defined by Morihara et al.7) contained the encephalomalasic brain tissue of the right frontal lobe. The 25-year-old male patient had orbital roof defect due to a motorbike accident experienced when 10-year-old7). MRI examination is superior for detection of any accompanying anomalies and the association of the encephalocele with the vascular structures and determination of the majort vascularization supplying blood to this field1).
The definite treatment method is surgical intervention after determination of encephaloceles and assessment of their structure5). The whole encephalocele sac should be repaired in a multidisciplinary way. The whole gliotic structures in the orbital cavity should be removed and the dura defect should be closed watertight and reconstructive cranioplasty should be performed. Temporal muscle fascia and watertight repair is sufficient for preventing CSF pulsation if the orbital defect area is below 2.5×2.5 cm2. Autogenous bones and artifical materials should be used for prevention of CSF pulsation if the defect area is above 3×3 cm2. Retraction of foramen rotundum and foramen ovale and cranial nerve, cavernous sinus, sagittal sinus injuries, intraorbital traumas and hemorrhages should be avoided during surgery. The artificial materials used during cranioplasty should be fixed so as not to allow dead space. Tight bandage and dressing should be applied in postoperative period and subcutaneous hydrops should be prevented. The most frequent complication is CSF leakage4,7).
Most authors recommend surgery within the first weeks. Early surgery enables better fixation of sutures and complete closure of dura. CSF leakage-related complications are seen more frrequently in delayed cases8).
CONCLUSION
For spheno-orbital encephaloceles, the following can be concluded : the important clinical findings are : pulsating exophthalmos induced by pulsating brain and orbital dystopia; 3D CT scanning and MRI are important modalities in the preoperative diagnosis, and the only effective treatment is surgery.