Park, Lee, Park, Kim, Lee, and Eoh: Surgical Management with Radiation Therapy for Metastatic Spinal Tumors Located on Cervicothoracic Junction : A Single Center Study
Abstract
Objective
The cervicothoracic junction (CTJ) is a biomechanically and anatomically complex region that has traditionally posed problems for surgical access. In this retrospective study, we describe our clinical experiences of the treatment of metastatic spinal tumors at the CTJ and the results.
Methods
From June 2006 to December 2011, 23 patients who underwent surgery for spinal tumors involving the CTJ were enrolled in our study. All of the patients were operated on through the posterior approach, and extent of resection was classified as radical, debulking, and simple neural decompression. Adjuvant radiation therapy (RT) was also considered. Visual analog scale score for pain assessment and Medical Research Council (MRC) grade for motor weakness were used, while pre- and post-operative performance status was evaluated using the Eastern Cooperative Oncology Group (ECOG).
Results
Almost all of the patients were operated using palliative surgical methods (91.3%, 21/23). Ten complications following surgery occurred and revision was performed in four patients. Of the 23 patients of this study, 22 showed significant pain relief according to their visual analogue scale scores. Concerning the aspect of neurological and functional recovery, mean MRC grade and ECOG score was significantly improved after surgery (p<0.05). In terms of survival, radiation therapy had a significant role. Median overall survival was 124 days after surgery, and the adjuvant-RT group (median 214 days) had longer survival times than prior-RT (63 days) group.
Conclusion
Although surgical procedure in CTJ may be difficult, we expect good clinical results by adopting a palliative posterior surgical method with appropriate preoperative preparation and postoperative treatment.
Key Words: Metastatic spinal tumor ┬Ę Cervicothoracic junction ┬Ę Treatment.
INTRODUCTION
The cervicothoracic junction (CTJ) is subject to unique biomechanical forces because it is a transitional zone between the lordotic, mobile cervical spine, and the kyphotic, more rigid thoracic spine 1). The CTJ is an anatomically complex region that has traditionally posed a problem for surgical access. Important neurovascular structures traverse this area, making exposure of the CTJ challenging 29). Surgical treatment of the CTJ in the spine requires special evaluation due to the anatomical and biomechanical characteristics of this spinal section. The transitional zone between the mobile cervical and the relatively rigid thoracic spine can be the site of serious unstable traumas or neoplastic lesions. Treatments for metastatic CTJ tumors are rare, and no technique is without its drawbacks, so the debate regarding the optimal approach continues. Most previous reports about metastatic spinal tumors concerned the entire spinal column or each spinal segment, for example, the cervical, thoracic, or lumbar spine 5,35). Even if reports dealt with the treatment strategy of CTJ tumor, they were heterogeneous studies composed of primary and metastatic tumors 18,24). In this retrospective study, we describe our clinical experiences of treatment of metastatic spinal tumors at CTJ and results with respect to pain relief, neurological recovery, complication that might occur, and post-operative survival. We propose an appropriate clinical approach to metastatic CTJ tumors.
MATERIALS AND METHODS
Patient selection
This was a retrospective reviewing of the charts of patients with metastatic spinal tumors of the CTJ who underwent surgery. Institutional Review Board approval was obtained. From June 2006 to December 2011, 29 patients underwent surgery for spinal tumors involving the cervicothoracic region at a single center by four surgeons comprising two neurosurgeons and two orthopedic surgeons. Our study included the patient undergone surgery of CTJ extending from vertebral segments C7 to T3 according to some previous reports 17,21,34). We excluded patients experiencing surgery at the same site, involving C7 vertebra alone and there was not available follow-up data. Also, patients harboring hematologic malignancy, multiple myeloma, and other highly radiosensitive tumors were excluded. Finally, 23 patients were enrolled in our study. Surgical treatment was considered when the metastatic lesion involved CTJ and this lesion was regarded to correlate with symptoms, for example, intractable pain or neurological deficit. Patients who were not candidates for surgery based on the advanced systemic disease, significant comorbidities, or short life expectancy less than 3 months as predicted by medical oncologists based on general performance and response of chemotherapy were conservatively treated and were not included in the present study. Preoperative work-ups included routine laboratory test, plain X-ray, computed tomography, and magnetic resonance imaging. According to Tomita's classification 33), in which lesions are classified according to tumor location inside or outside the anatomical barrier, all patients were classified. Tomita type 1-3 is intra-compartmental type, type 4-6 is extracompartmental, and type 7 is multiple lesions.
Surgical and adjuvant treatment
Prior to surgery, in cases of hypervascular tumor or large tumor mass, preoperative angiography and tumor embolization was performed to reduce bleeding during the operation by interventional radiologist. Intraoperative monitoring including motor evoked potential and somatosensory evoked potential was used to reduce neurological injury beginning in March, 2008. All patients who underwent CTJ surgery stayed at the intensive care unit postoperatively to cope with acute complication. Surgical techniques used posterior approaches. Posterior approaches including true posterior and posterolateral approach were simple decompression with laminectomy for tumor involved posterior column, laminectomy plus trans-pedicular anterior decompression for tumor located vertebral body and total spondylectomy. For anterior column support, the corpectomy followed by inserting titunum mesh cage or cement block. All procedures were combined with instrumentation including lateral mass screw, or pedicle screw, except for three patients. The extent of tumor resection was classified into radical surgery, debulking surgery in which residual tumor mass was <30% of its primary volume, and simple neural decompression in which residual tumor mass was >30% of its primary volume. The latter two types were considered palliative surgery. Adjuvant radiation therapy (RT) was considered for those not receiving the treatment prior to surgery. Chemotherapy was also performed as another adjuvant treatment option.
Analysis of clinical and radiologic outcome
Operative chart review identified estimated blood loss (EBL) and length of operation time, major and minor complications, expire date, and last follow-up date. For pain assessment at the preoperative and postoperative periods, we used a visual analogue scale (VAS). Motor status was evaluated by the Medical Research Council (MRC) scale for muscle strength at hospital admission, as well as at follow-up. For prediction of survival period, the Tomita and the revised Tokuhashi scoring system were used. Performance status was evaluated as secondary outcome, and assessed using the Eastern Cooperative Oncology Group (ECOG) scale.
In our institute, all patients were checked using simple X-ray to identify changes in kyphotic angle of the CTJ spine, and to detect possible failure of implants at every 1 month after discharge, except when patient survival was too short or because of follow-up loss. Follow-up ranged from 0.7 to 19.4 months with an average of 5.9 months.
Survival analysis
For survival analysis, we calculated follow-up days from surgery to last follow-up date. To clarify of significant variable related with survival, the aforementioned variables used to analyze clinical results were used. For analysis of these outcomes, we used various predictive factors including Tomita and Tokuhashi scores 30,32), approach side, extent of resection, whether or not preoperative embolization was performed, and presence of radiation therapy and its timing (RT prior to surgery and RT following surgery).
Statistical analyses
For investigation of the baseline characteristics of patients, descriptive statistics was used. Comparison of the pain and motor score between preoperative and postoperative status was analyzed by Wilcoxon signed rank test, one-way analysis of variance, or Kruskal-Wallis test. Two sample t-test or Mann-Whitney test was used to test whether or not preoperative embolization was related to intraoperative blood loss. For analysis of overall survival and survival difference between groups, the Kaplan-Meier method and log-rank test were used. Statistical analyses were performed using IBM SPSS 21.0 statistical software (IBM Corp., Armonk, NY, USA). A probability value <0.05 was accepted as statistically significant.
RESULTS
Patients' demographics
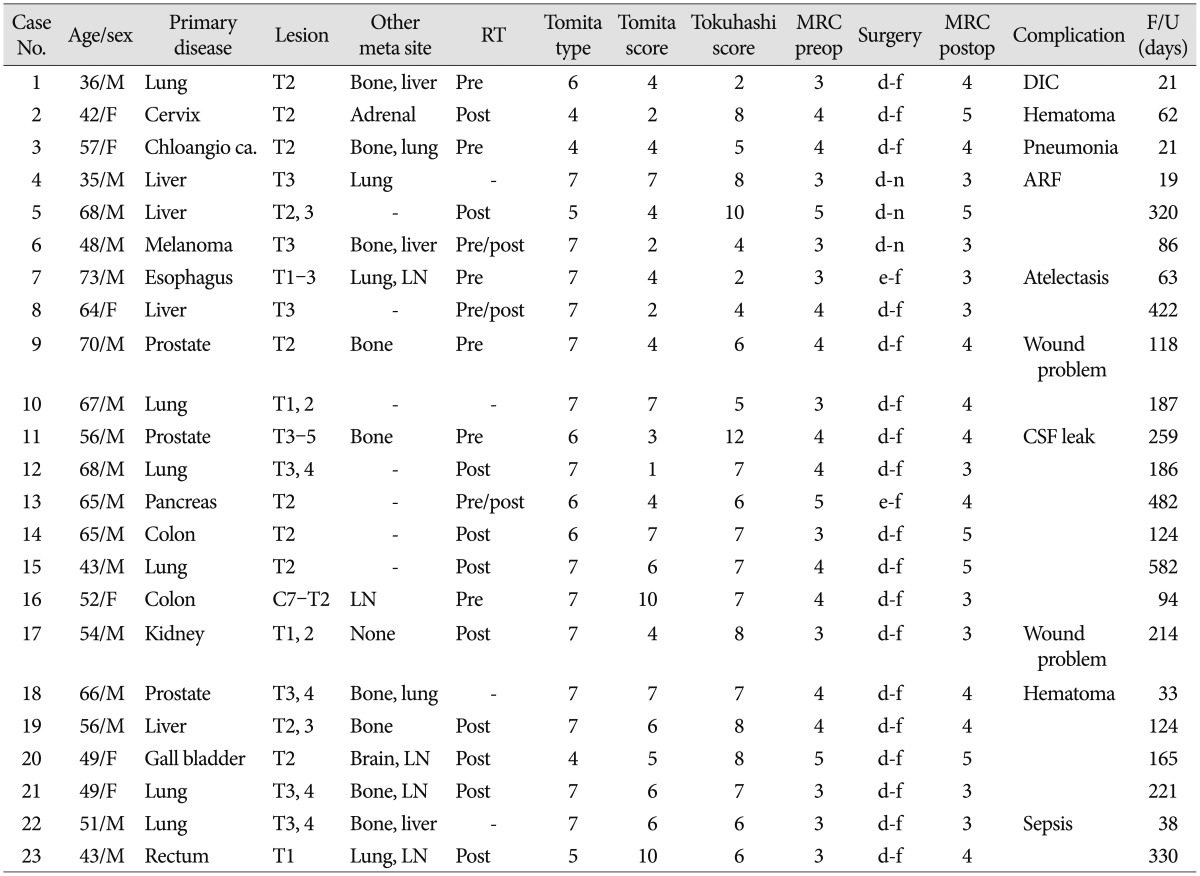
Baseline characteristics of patients are recorded in Table 1. A total of 23 patients underwent resection of CTJ tumors between 35 to 73 years with an average of 54.72 years. There were 17 men and six women. All patients presented with one or both of pain and weakness. MRC scale at hospital admission was grade 3 in 10, grade 4 in 10, and grade 5 in 3 patients. Various primary cancers were metastasized to the spine. The most frequent pathology was lung cancer in six cases, hepatocellular carcinoma in four cases, and colorectal cancer and prostate cancer in three cases respectively. T2 was the most frequent metastatic site followed by T3 and T1. 16 patients had additional metastases of other organ and site (69.6%). All metastatic lesions were Tomita type 4 or higher and 18 patients had multiple spine metastases including Tomita type 6 and 7. 11 patients had a Tomita score exceeding 5 (47.8%). Applying Tokuhashi prognostic score, however, 21 patients (91.3%) were expected to have a poor prognosis (Tokuhashi score <9) ( Table 1). In 9 patients, RT was performed prior to surgery as treatment modality for metastatic tumor. In ECOG performance scores before surgery, two patients were ECOG 2, seven were ECOG 3, and fourteen were ECOG 4.
Outcomes of surgical and adjuvant treatment
Almost all patients were operated using palliative surgical methods (91.3%, 21/23) that included debulking surgery or simple decompression. 20 patients were instrumented by cervical lateral mass screws and/or pedicle screws including C7 pedicle screw. Of these patients, bone cement and titanium cage was used in two patients to augment vertebral body. Three patients did not require instrumentation.
In fourteen patients, preoperative tumor embolization was undergone without any complications. In patients who underwent preoperative tumor embolization, more intraoperative blood loss was seen (mean EBL in non-embolization group, 715 mL; in embolization group, 810 mL). When considered for only hypervascular tumor including thyroid cancer, hepatocellular carcinoma and renal cell carcinoma, preoperative embolization helps to reduce operative blood loss (mean EBL in non-embolization group 1490 mL; in embolization group, 918 mL). The preoperative embolization group had a shorter operation time than the non-embolization group (non-embolization group, 284.9 min; embolization group, 232.2 min).
Adjuvant radiation therapy was performed in 13 patients after wound healing, including three patients who received preoperative radiation therapy previously. In most patients who underwent radiation therapy, 30 Gy in 10 fraction planning was used. Nine patients including four patients with adjuvant radiation therapy were treated with chemotherapy.
Perioperative mortality and morbidity
Thirty-day mortality rate were 13.0% (3/23). One lung cancer patient died due to serious disseminated intravascular coagulopathy after severe intraopeative bleeding. Another one cholangiocarcinoma patient with brain metastasis died after posterior surgery due to postoperative pneumonia. One hepatoma patients died with disease progression with acute renal failure, even though his neurological function was good (MRC grade 4).
Postoperative complications were found in ten patients (43.5%). Complications in six patients were related with surgery itself. The other complications were related with systemic causes ( Table 2). The most frequent problem was wound problems, precisely wound dehiscence or infection (3/23, 13.0%) in which two patients underwent reoperation. However there was seen no implant failure or aggravation of kyphosis during perioperative period. Fig. 1 summarized trends of postoperative mortality and morbidity during study period.
Clinical and radiologic outcomes
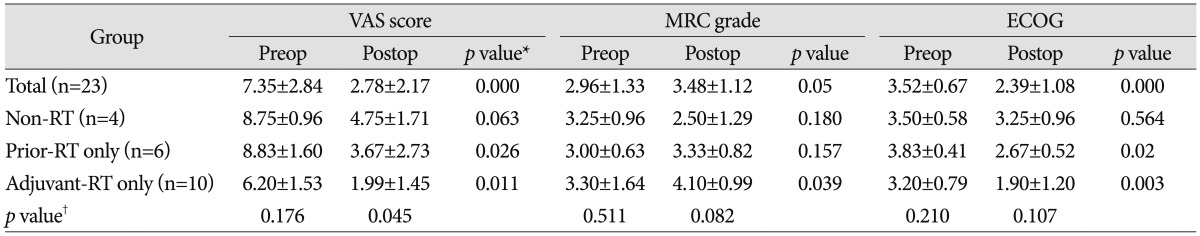
Table 3 summarized clinical and functional outcomes after surgery. Of the 23 patients of this study, 21 patients showed pain relief according to VAS score after surgery. The other two patients did not complain of pain at initial presentation. Mean postoperative VAS score was significantly reduced compared with mean preoperative status, 2.78 and 7.35, respectively ( p<0.001). In the aspect of neurologic recovery, mean MRC grade was significantly improved after surgery (preoperative 2.96, postoperative 3.48, p=0.05).Only one patient showed deterioration of one points MRC grade (preoperative 5, postoperative 4). After surgery, the ECOG either improved or remained unchanged in 22 patients. Specifically, no change between the pre- and post operative ECOG scores was found for one patient. Seventeen patients (73.9%) experienced an improvement in their ECOG score by 1-grade, while two patients (8.7%) experienced an improvement of 2-grades and two patients (8.7%) experienced an improvement of 3-grades.
All patients received RT showed significant pain reduction and improvement of ECOG score regardless of RT timing ( Table 3). However, motor strength was significantly recovered only in patients undergone postoperative RT regardless of receiving preoperative RT ( p=0.017). During follow-up, spinal stability were actually achieved in all patients, whilst two patients with adjacent new metastasis had subsequent progressive kyphosis. A case of anterior slippage of mesh cage on X-ray was observed at five months after surgery. There was no new neurological symptom or sign related to progressive kyphosis and slippage of case. The average preoperative kyphosis measured 25┬░ (range, 15-37┬░). The average Cobb angles in the last follow-up examination was 18┬░ with a range of 12-26┬░.
Survival after surgery
Totally, median overall survival was 124 days (95% CI, 50.4-197.6) after surgery ( Fig. 2). Additionally, there was no significant difference of survival according to the Tomita and Tokuhashi scores, primary pathology, ambulatory ability, ECOG performance, neurological improvement and extent of resection. Patient who underwent RT had longer survival period compared with patients who did not undergo RT ( Fig. 3). Despite primary pathology of prior-RT only group and adjuvant-RT group did not differ, there was no significant survival difference between the prior-RT group and non-prior RT group. However there was significant survival difference between the adjuvant-RT group and non-adjuvant-RT group. Median survivals are 63 days in prior-RT only group (95% CI, 0-150.6) and 186 days (95% CI, 110.1-261.9) in adjuvant-RT only group, respectively.
DISCUSSION
The CTJ has unique anatomical and biomechanical properties. Various bony structures, such as chest wall, shoulder, rib cage, clavicle, and scapula, and visceral structures including the lung, heart, and great vessels disturb the surgical approach 13,19,29) and use of intraoperative C-arm fluroscopy 20). Biomechanical transition property also makes this region difficult to reconstruct. Although many surgical approaches and methods, and modifications, have been described1, 2,7,9,16,19,21,27), no technique is without its drawbacks.
Surgical option for CTJ metastasis
Combined anterior-posterior approach is indicated in most traumatic lesions involving the CTJ vertebral body 13,15,17). In the neoplastic series, however, surgical procedure was usually posterior, because of patients' poor general status and short life expectancy. The anterior approach may be contraindicated in relation to clinical status and/or life expectancy. Especially, the anterior approach to CTJ is technically demanding and some risks and complication may arise. For example, performing a manubriotomy increases surgical time, bleeding, postoperative pain intensity, and length of hospital stay 3,10,15). Dissection of the sternoclavicular joint or clavicle resection induces shoulder instability, weakness, and deformity 7,9). In patients harboring metastatic tumor, however, the goal of surgery is palliation in most cases, so usually there is no need to bear the risk. In our study, surgery was performed through the posterior approach, similar to two previous studies about posterior approach about CTJ tumors 18,24) that also displayed usefulness of posterior approach, although they were combined primary and metastatic cases. Generally, posterior approaches are disadvantageous because of a destabilization effect, inadequate visualization of the vertebral body pathology, and the need for a long posterior construct to restore stability with a higher complication rate than anterior or lateral approaches. In neoplastic condition, advantages of this approach include a relative blood and time saving procedure since the main tumor mass is regularly located in the anterior region of the spine, and a rigid fusion even for polysegmental distances.
Survival and prognostic factors
Concerning the extent of resection, more resection of tumor was associated with a longer median survival time than the limited surgery in thoracic and thoracolumbar metastasis, which was also concluded through an international multicenter prospective observational study 12). In addition, Tomita et al. 31) reported that local recurrences were absent after total en bloc spondylectomy. However, in the CTJ, radical surgery including en bloc spondylectomy may be difficult due to the aforementioned biomechanical and anatomical reasons. Aggressive surgery showed severe intraoperative blood loss, longer operation time, and more complications. Several recent studies 8,23) elucidated the role of limited or palliative surgery. In our study, the degree of surgical resection did not show to significantly alter survival in CTJ spinal metastasis. However, our data support a significant improvement in postoperative overall survival following postoperative radiation. The survival rate of adjuvant RT group was statistically better than that of non RT or prior RT group.
Perioperative management for CTJ metastasis
Our surgical results showed high mortality and morbidity rate, even though surgery had a palliative role in the patient's pain and functional outcome. Post-operative complication rate was 43.5% and thirty-day mortality rate was 13% in our study. When compared with previous reports dealing with metastatic spine tumor, these rates are relatively high.
In our study, the most common complication was also wound problems, consistent with another report about metastatic spinal tumors 24). Failure of primary healing can lead to wound dehiscence, infection, and neurological compromise. Especially, CTJ has various muscles involved in shoulder movement. Therefore, wound problems like dehiscence could occur frequently. Even in other series, major complications were not found in the anterior approach but in the posterior surgery 15,16,17,18,19,34). Poor wound closure technique and postoperative wound infection, although superficial, have played a role. Securing the posterior paraspinal muscles to the remaining cephalad and caudad spinous processes and bringing the fascia closure to midline may also help to reduce this complication. In addition, preoperative embolization has been useful in reducing blood loss, length of surgery, and postoperative hemorrhage to remove the vertebral body pathology via posterior approach, and spinal angiography does not pose significant procedure-related complications 14). In our study, most of medical complication occurred in the early period. Recent improvements of various conservative care and intensive medical care skills have reduced complication rate as seen Fig. 1. As these supports, no more death was due to a surgical complication-related cause during recent 4 years in our series.
Role of radiotherapy
Even though the reported functional superiority of the surgical arm has be 23), RT as an initial treatment of choice for metastatic spinal tumor showed good clinical outcome including pain reduction and neurologic symptoms 11,28). Many institutes select RT as the initial treatment modality, because of surgery-related complications. Naturally, in the case of radiosensitive tumors, the expected survival of less than 3 months and inability of the patient to tolerate an operation, RT is the primary treatment option. Although baseline epidemiological characteristics between the prior-RT group and adjuvant-RT group did not show significant differences in this study, the prior-RT group had no longer survival time than the adjuvant-RT group. A previous report speculated that preoperative radiation may have direct (radiation-induced myelitis) and indirect (reactive gliosis, fibrosis, compromised spinal cord blood supply) effects that may prevent neurological recovery after surgery 4). Neurological function, especially ambulatory function, is a factor that has been most consistently cited as determining survival 22,26).
Limitations of study
Recently, quality of life as well as surgical outcome and survival has been emphasized to treat metastatic spinal tumors 6,8,25). This study lacked this analysis. Data on the natural progression in patients with spinal metastasis with palliative care only and the results of nonsurgical treatment are required. Due to the nature of the location, limited and diverse cases were available for this study. A future comprehensive prospective study will need to resolve these limitations.
CONCLUSION
Our study suggests that metastatic spinal tumor at cervicothoracic junction should be considered a unique area, and surgical procedures in this area may be difficult. When deciding on surgery for CTJ tumor, preoperative embolization would be helpful in reducing blood loss and operation time, therefore helping to reduce morbidity. Appropriate surgical procedures including posterior approach, debulking surgery, and stabilization under neurophysiologic monitoring followed adjuvant radiation therapy are considered very important part of the treatment. In addition, intensive postoperative care is another component for good clinical outcome.
References
1. An HS, Vaccaro A, Cotler JM, Lin S : Spinal disorders at the cervicothoracic junction. Spine (Phila Pa 1976) 1994, 19 : 2557-2564,   2. Boockvar JA, Philips MF, Telfeian AE, O'Rourke DM, Marcotte PJ : Results and risk factors for anterior cervicothoracic junction surgery. J Neurosurg 2001, 94( 1 Suppl):12-17,   3. Cauchoix J, Binet JP : Anterior surgical approaches to the spine. Ann R Coll Surg Engl 1957, 21 : 237-243,   4. Chaichana KL, Woodworth GF, Sciubba DM, McGirt MJ, Witham TJ, Bydon A, et al : Predictors of ambulatory function after decompressive surgery for metastatic epidural spinal cord compression. Neurosurgery 2008, 62 : 683-692; discussion 683-692,   5. Cho W, Chang UK : Neurological and survival outcomes after surgical management of subaxial cervical spine metastases. Spine (Phila Pa 1976) 2012, 37 : E969-E977,   6. Choi D, Crockard A, Bunger C, Harms J, Kawahara N, Mazel C, et al : Review of metastatic spine tumour classification and indications for surgery : the consensus statement of the Global Spine Tumour Study Group. Eur Spine J 2010, 19 : 215-222,   7. Dartevelle PG, Chapelier AR, Macchiarini P, Lenot B, Cerrina J, Ladurie FL, et al : Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J Thorac Cardiovasc Surg 1993, 105 : 1025-1034,   8. Fujibayashi S, Neo M, Miyaki K, Nakayama T, Nakamura T : The value of palliative surgery for metastatic spinal disease : satisfaction of patients and their families. Spine J 2010, 10 : 42-49,   9. Grunenwald D, Spaggiari L : Transmanubrial osteomuscular sparing approach for apical chest tumors. Ann Thorac Surg 1997, 63 : 563-566,   10. Hodgson AR, Stock FE, Fang HS, Ong GB : Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott's disease of the spine. Br J Surg 1960, 48 : 172-178,   11. Hoegler D : Radiotherapy for palliation of symptoms in incurable cancer. Curr Probl Cancer 1997, 21 : 129-183,   12. Ibrahim A, Crockard A, Antonietti P, Boriani S, B├╝nger C, Gasbarrini A, et al : Does spinal surgery improve the quality of life for those with extradural (spinal) osseous metastases? An international multicenter prospective observational study of 223 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2007. J Neurosurg Spine 2007, 8 : 271-278,  13. Karikari IO, Powers CJ, Isaacs RE : Simple method for determining the need for sternotomy/manubriotomy with the anterior approach to the cervicothoracic junction. Neurosurgery 2009, 65( 6 Suppl):E165-E166; discussion E166,   14. Kato S, Murakami H, Minami T, Demura S, Yoshioka K, Matsui O, et al : Preoperative embolization significantly decreases intraoperative blood loss during palliative surgery for spinal metastasis. Orthopedics 2012, 35 : e1389-e1395,   15. Kn├Čller SM, Brethner L : Surgical treatment of the spine at the cervicothoracic junction : an illustrated review of a modified sternotomy approach with the description of tricks and pitfalls. Arch Orthop Trauma Surg 2002, 122 : 365-368,   16. Korst RJ, Burt ME : Cervicothoracic tumors : results of resection by the "hemi-clamshell" approach. J Thorac Cardiovasc Surg 1998, 115 : 286-294; discussion 294-295,   17. Lehman RM, Grunwerg B, Hall T : Anterior approach to the cervicothoracic junction : an anatomic dissection. J Spinal Disord 1997, 10 : 33-39,   18. Mazel C, Hoffmann E, Antonietti P, Grunenwald D, Henry M, Williams J : Posterior cervicothoracic instrumentation in spine tumors. Spine (Phila Pa 1976) 2004, 29 : 1246-1253,   19. Mihir B, Vinod L, Umesh M, Chaudhary K : Anterior instrumentation of the cervicothoracic vertebrae : approach based on clinical and radiologic criteria. Spine (Phila Pa 1976) 2006, 31 : E244-E249,   20. Moulton C, Griffiths PD : The adequacy of cervical spine radiographs in the accident and emergency department. J R Soc Med 1993, 86 : 141-143,     21. Nazzaro JM, Arbit E, Burt M : "Trap door" exposure of the cervicothoracic junction. Technical note. J Neurosurg 1994, 80 : 338-341,   22. North RB, LaRocca VR, Schwartz J, North CA, Zahurak M, Davis RF, et al : Surgical management of spinal metastases : analysis of prognostic factors during a 10-year experience. J Neurosurg Spine 2005, 2 : 564-573,   23. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ, et al : Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer : a randomised trial. Lancet 2005, 366 : 643-648,   24. Placantonakis DG, Laufer I, Wang JC, Beria JS, Boland P, Bilsky M : Posterior stabilization strategies following resection of cervicothoracic junction tumors : review of 90 consecutive cases. J Neurosurg Spin 2008, 9 : 111-119,  25. Pointillart V, Vital JM, Salmi R, Diallo A, Quan GM : Survival prognostic factors and clinical outcomes in patients with spinal metastases. J Cancer Res Clin Oncol 2011, 137 : 849-856,   26. Rades D, Veninga T, Stalpers LJ, Basic H, Hoskin PJ, Karstens JH, et al : Improved posttreatment functional outcome is associated with better survival in patients irradiated for metastatic spinal cord compression. Int J Radiat Oncol Biol Phys 2007, 67 : 1506-1509,   27. Sundaresan N, Shah J, Foley KM, Rosen G : An anterior surgical approach to the upper thoracic vertebrae. J Neurosurg 1984, 61 : 686-690,   28. Tancioni F, Navarria P, Pessina F, Attuati L, Mancosu P, Alloisio M, et al : Assessment of prognostic factors in patients with metastatic epidural spinal cord compression (MESCC) from solid tumor after surgery plus radiotherapy : a single institution experience. Eur Spine J 2012, 21( Suppl 1):S146-S148,   29. Tarantino R, Donnarumma P, Marruzzo D, Landi A, De Giacomo T, Delfini R : Anterior surgical approaches to the cervicothoracic junction : when to use the manubriotomy? Spine J 2013, 13 : 1064-1068,   30. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J : A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976) 2005, 30 : 2186-2191,   31. Tomita K, Kawahara N, Baba H, Tsuchiya H, Nagata S, Toribatake Y : Total en bloc spondylectomy for solitary spinal metastases. Int Orthop 1994, 18 : 291-298,   32. Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T : Surgical strategy for spinal metastases. Spine (Phila Pa 1976) 2001, 26 : 298-306,   33. Tomita K, Kawahara N, Murakami H, Demura S : Total en bloc spondylectomy for spinal tumors : improvement of the technique and its associated basic background. J Orthop Sci 2006, 11 : 3-12,    34. Wang JC, Boland P, Mitra N, Yamada Y, Lis E, Stubblefield M, et al : Single-stage posterolateral transpedicular approach for resection of epidural metastatic spine tumors involving the vertebral body with circumferential reconstruction : results in 140 patients. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine 2004, 1 : 287-298,   35. Weber MH, Burch S, Buckley J, Schmidt MH, Fehlings MG, Vrionis FD, et al : Instability and impending instability of the thoracolumbar spine in patients with spinal metastases : a systematic review. Int J Oncol 2011, 38 : 5-12, 
Fig.┬Ā1
Annual prevalence of perioperative mortality and morbidity during enrolled period. 
Fig.┬Ā2
Overall survival of 23 patients underwent surgery for spinal metastases involving the cervicothoracic junction. Median overall survival was 124 days (95% CI, 50.4-197.6). 
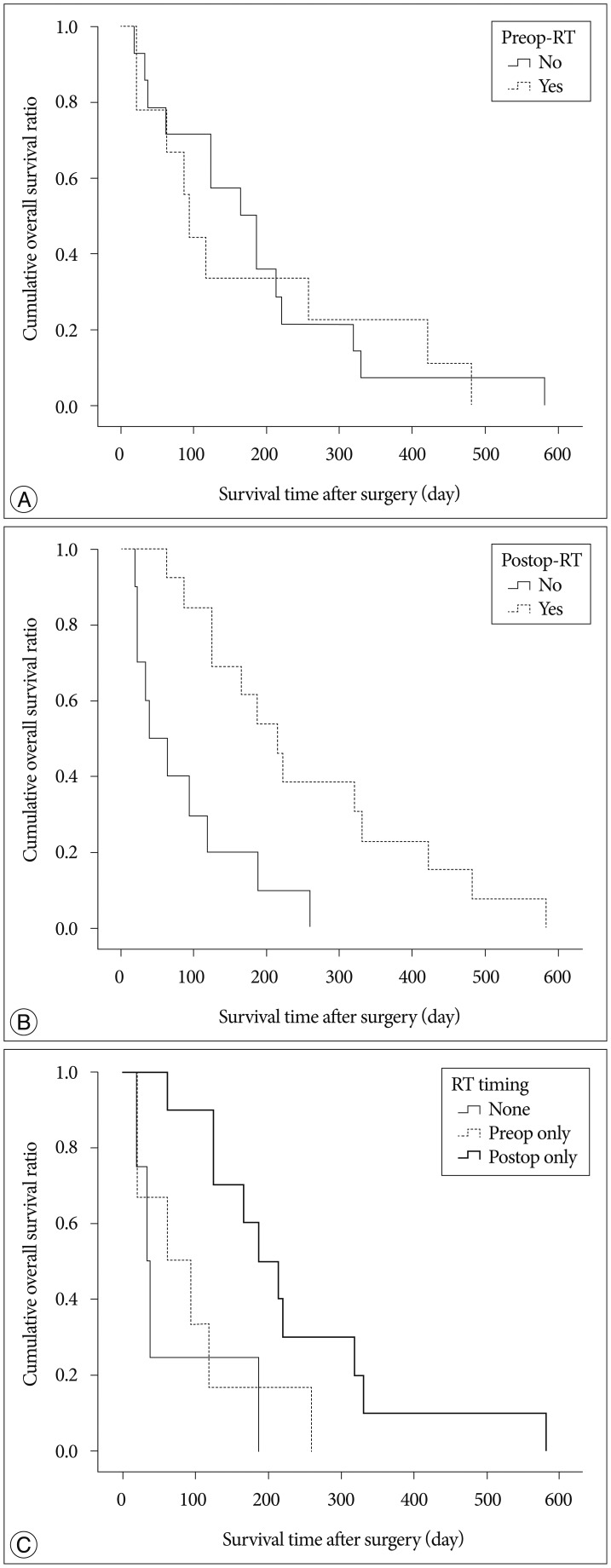
Fig.┬Ā3
A : Survival of 23 patients received surgery for cervicothoracic junction (CTJ) metastasis according to whether prior-RT was performed (log-rank test; p=0.808). B : Survival of 23 patients received surgery for CTJ metastasis according to whether adjuvant-RT was performed (log-rank test; p=0.002). C : Survival of 20 patients excluding 3 patients received prior-RT and adjuvant-RT according to RT timing (no RT vs. prior RT only vs. adjuvant RT only; log-rank test; p=0.025). RT : radiation therapy. 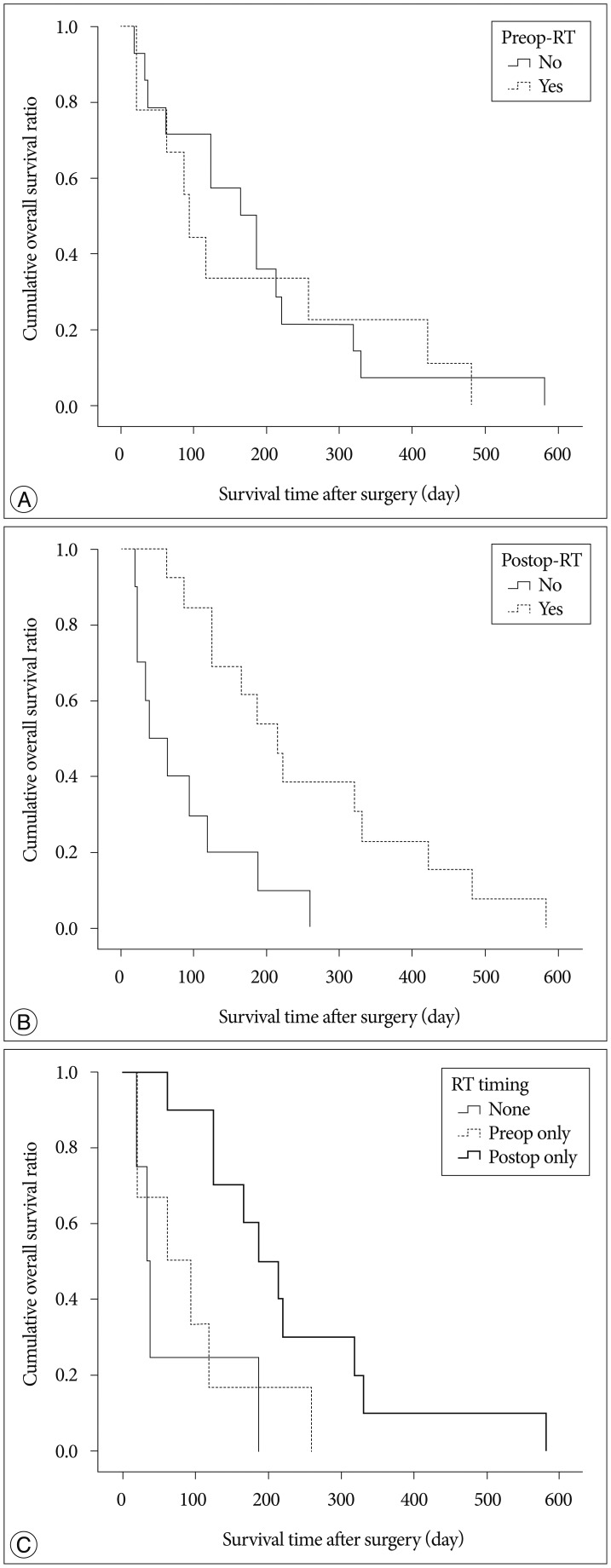
Table┬Ā1
Epidemiologic and clinical information of 23 patients enrolled in the study 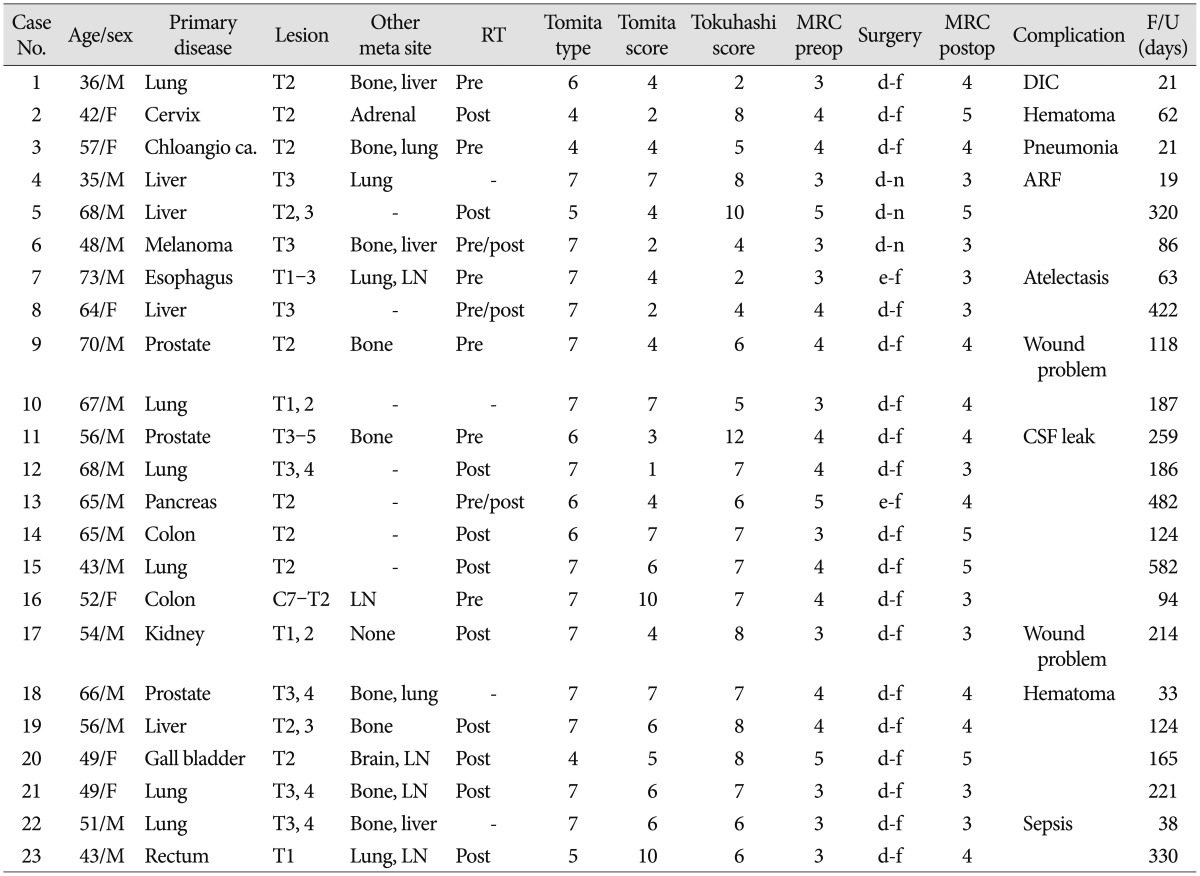
Table┬Ā2
Postoperative complications reoperation and perioperative death after surgery 
Table┬Ā3
Comparison of VAS score, MRC grade, and ECOG scale in 23 patients according to timing of radiation therapy 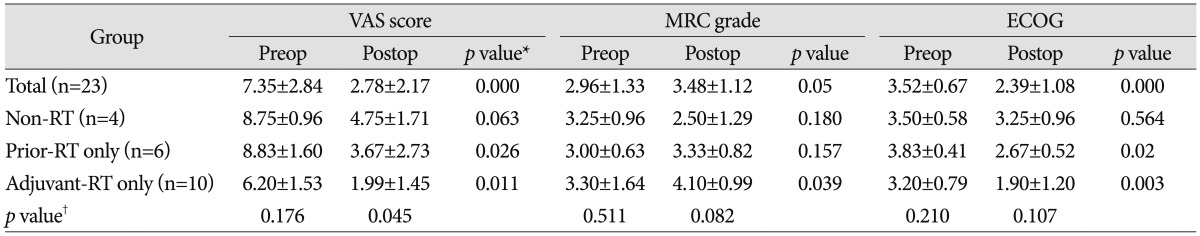
|
|