INTRODUCTION
Most osteoporotic compression fractures heal with mild residual deformities, and clinical complications are usually rare5). When conservative treatment offers no symptomatic improvement, percutaneous vertebroplasty or balloon kyphoplasty have been safely used and have provided rapid pain relief with mechanical stabilization10). Sometimes, however, patients complain about both back pain and newly developed leg pain following vertebral compression fractures. The main symptom can be radicular leg pain, rather than axial pain, which mimics foraminal stenosis or disc herniation. This radiculopathy is thought to be caused by the encroachment of the intervertebral foramen2). In those cases, it is difficult to perform bone cement augmentation because it is known that percutaneous vertebroplasty is a relative contraindication to the conditions causing radicular symptoms in patients who present with canal encroachment1). This study aimed to investigate the risk for newly developed radiculopathic leg pain following lumbar osteoporotic compression fracture by analyzing the fracture pattern. We also studied whether bone cement augmentation would lead to a good or poor clinical outcome.
MATERIALS AND METHODS
Between May 2008 and April 2010, 238 patients underwent single-level vertebroplasty or balloon kyphoplasty for osteoporotic compression fractures in our institute.
The inclusion criteria were as follows : 1) fracture location under L2 level that can lead to radiculopathic leg pain following vertebral compression fracture; 2) osteoporotic spine (T-score by bone mineral densitometry lower than -3.0); 3) follow-up period longer than 6 months; and 4) no radiculopathic leg pain before the osteoporotic compression fracture.
Patients with obvious burst fractures at the time of injury, with previous history of spine surgery or radiculopathic symptom before compression fracture, were excluded in this study. Of these 238 patients, 59 who had osteoporotic compression fractures and underwent percutaneous vertebroplasty or balloon kyphoplasty under the L2 level were enrolled in this study.
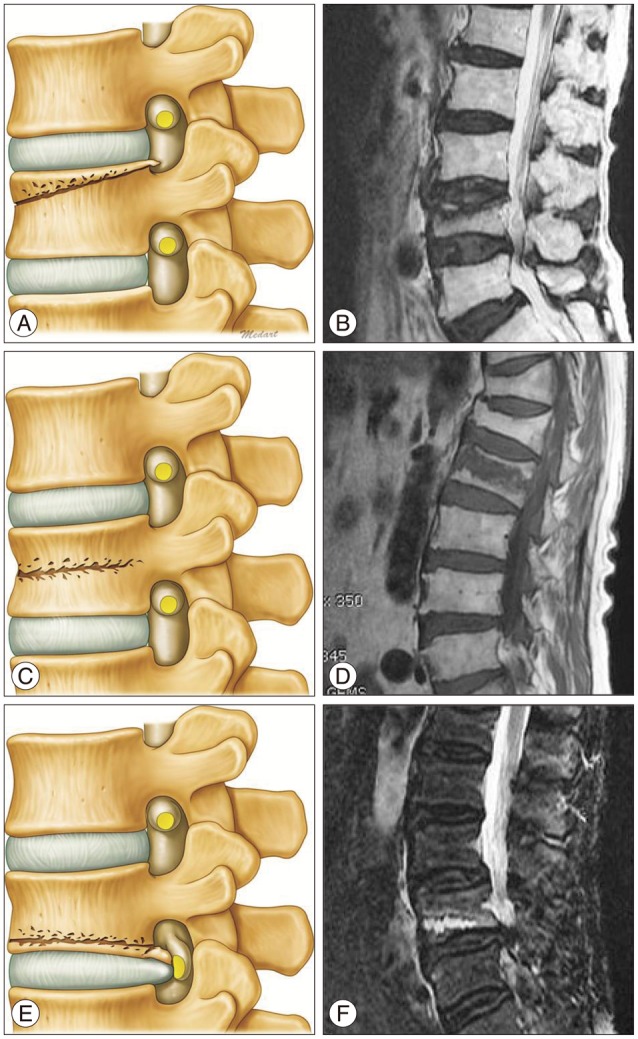
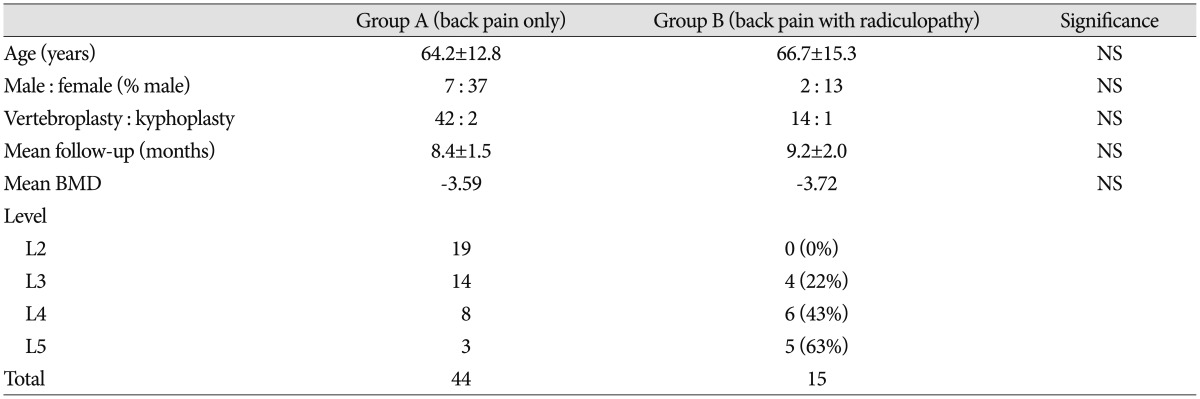
To study whether the fracture pattern influences the newly developed radiculopathy and back pain, the 59 patients were divided into two groups, namely group A (n=44), back pain-only, and group B (n=15), back pain with newly developed unilateral leg pain. Fractures were evaluated using early magnetic resonance imaging (MRI) based on Kanchiku's method and we classified into three types according to the main position of the fracture line on the basis of T1, T2-weighted fat and suppression images (superior, middle, and inferior) (Fig. 1)6). The statistical significance of each fracture pattern relative to radiculopathy was examined and analyzed. The preoperative group differences data were evaluated by the unpaired Student t-test using the SPSS program (SPSS Inc., Chicago, IL, USA), and intragroup changes associated with the procedure were evaluated using the Student t-test for paired data with a p<0.01 considered the significance level.
RESULTS
The anatomical distribution of the 59 patients was as follows : L2 (n=19), L3 (n=18), L4 (n=14), and L5 (n=8). Among them, 56 patients underwent percutaneous vertebroplasty and 3 patients underwent balloon kyphoplasty. There were no significant differences between group A and group B with respect to age and gender. The overall incidence of radiculopathic leg pain under the L2 level was 25% (n=15). There was no newly developed radiculopathy at the L2 level, and the frequency of radiculopathic leg pain increased with descending levels (Table 1).
Although vertebral collapse was not severe in lumbar radiographs and MRI, 10 of 15 patients in the group B showed compression fracture and suspicious impingement of the corresponding nerve root at the intervertebral foramen.
Fracture pattern and radiculopathy
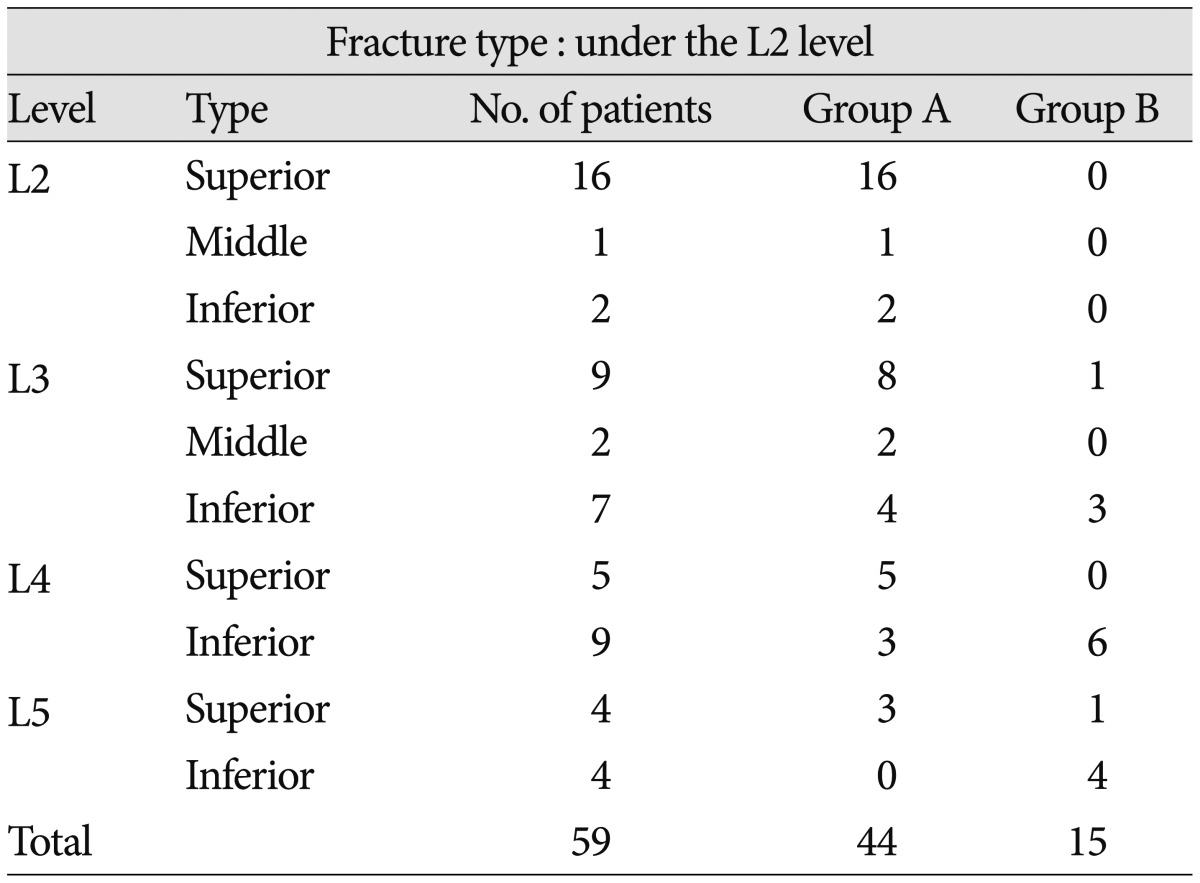
In the analysis of fracture pattern under the L2 level, which showed radiculopathy, only the back pain group (group A) demonstrated symptoms relating to the superior fracture type. However, the fracture pattern in the group with back and radiculopathic pains (group B) was mostly related to the inferior fracture type (Table 2). Such a difference was statistically significant (p<0.01) and can be attributed to the different pathophysiological mechanism in the two groups (Fig. 2).
Clinical outcome
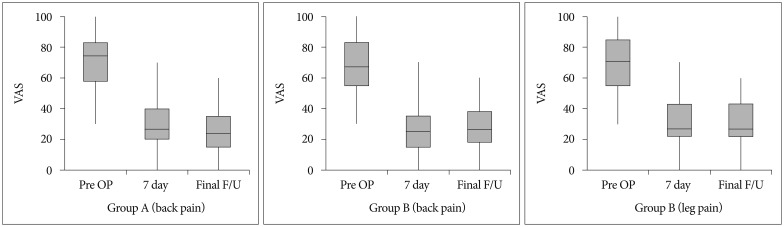
The mean back pain score of both groups showed significant improvement at the last follow-up. Interestingly, the mean pain score of leg pain in group B also showed significant improvement after bone cement augmentation without decompressive open surgery.
The visual analogue scale decreased from a preoperative score of 6.5 to 3.0 at 7 postoperative days and it was maintained at final follow-up with respect to radiculopathy (Fig. 3). Three patients (2 in L4 and 1 in L5) in group B had recurrent radicular pain during the follow-up period, but their pain was tolerable, as controlled by analgesics (Fig. 4, 5).
DISCUSSION
Compression fractures caused by osteoporosis are common in the elderly and are often encountered by spine surgeons. It is well known that bone cement augmentation procedures such as percutaneous vertebroplasty or balloon kyphoplasty improve back pain from osteoporotic compression fractures4,8). However, in some instances, lumbar osteoporotic compression fractures without evident canal compromise cause radiculopathic radiating pain and spinal canal stenosis leading to claudication7). Treatment of osteoporotic compression fractures accompanying radiculopathic radiating pain or spinal stenosis is challenging. Conservative treatment using a lumbar brace for compression fracture forces the posture in lumbar extension, worsening central or foraminal stenosis2). Surgical treatment of lumbar stenosis with open decompression with instrumented stabilization has the potential for significant complications because of comorbidities related to advancing age, especially severe osteoporosis and high risk for instrumentation failure9).
This study was performed to clarify and analyze whether an early fracture pattern based on MRI classification influences the newly developed radiculopathy in osteoporotic compression fractures and clinical outcome after bone cement augmentation procedure. In this study, the incidences of acute and newly developed leg pain after osteoporotic vertebral compression fractures have increased gradually from the L3 to L5 levels. Most patients in those cases have inferior-type fractures. The possible cause of radiculopathic leg pain after osteoporotic compression fracture may be considered to be the following mechanism : when the osteoporotic vertebral fracture occurs, if the bony fragments from the collapsed body invade the foraminal space, the root can be compressed directly, leading to radiculopathy. The decreased foraminal height by vertebral body collapse will be worse. By categorizing fractures on the basis of fracture line, we found that inferior-type fractures were related to radiculopathic leg pain. The second plausible mechanism may be considered to be a referred pain, which is distributed far from the site of injury. Doo et al.3) reported that the posterior branches can be irritated by the narrowing of the intervertebral foramen resulting from the decreased height of the vertebral bodies, their pain may have been distributed in these areas as a radicular or somatic referred pain.
We performed bone cement augmentation alone because it is a simple and less invasive procedure, and it was efficacious in providing satisfactory pain relief, not requiring open decompressive surgery even in radiculopathy.
The pain relief mechanisms by vertebral augmentation procedures may be deduced as the following mechanism. First, segmental stability provided by the cement augmentation is increased, and second, retropulsion and foraminal narrowing are decreased. As spondylotic changes progress in the lumbar spine during aging, the foraminal space decreases with facet hypertrophy, reduced disc height, and foraminal or extraforaminal disc herniations. This process may accompany senile osteoporosis. Actually, the radicular pain in most patients in group B was aggravated in the erect position. Because the posterior wall of the vertebral body inferior to the pedicle constitutes a large portion of intervertebral foramen, the size of the intervertebral foramen will diminish when the compression fracture involves that part of the vertebra. If the root impingement occurs by a combination of spondylotic foraminal stenosis and vertebral fracture, the degree of root compression will increase by weight loading because of the decreased stiffness of the vertebral body. If this is the main mechanism of the patients' symptoms, bone cement augmentation may play a major role in relieving the radicular pain secondary to some degree of fracture reduction and mechanical stabilization. We could achieve favorable clinical outcome by bone cement augmentation procedure alone.
Despite our successful results, this study has some limitations. The authors' proposed pathomechanism is presumptive and is supported mainly by the patient's immediate and symptomatic improvement during follow-up. For a more scientific approach to this subject, experimental data include accurate measurement of the size of the intervertebral foramen according to the weight loading in a fractured vertebra. Experimental study with the finite element model can be a good method that can confirm our results. In the near future, randomized clinical trials for comparative studies in a larger population for a longer period are necessary.
CONCLUSION
By categorizing fractures on the basis of fracture line, we found that inferior-type fractures were more related to the development of radiculopathic leg pain. Bone cement augmentation alone can be a safe and efficient option in patients with painful osteoporotic compression fracture and radiculopathy.