INTRODUCTION
Traumatic aneurysms of the middle meningeal artery (MMA) are rare occurrences that are usually associated with an underlying skull fracture4), which comprise less than 1% of all intracranial aneurysms3,15). Most of these aneurysms are actually false aneurysms, or pseudoaneurysms, which are caused by the rupture of entire vessel wall layers, with the wall of the aneurysm being formed by the surrounding cerebral structures10). Acute or delayed epidural hematoma is the most frequent presentation of traumatic pseudoaneurysms10,15), but it can be associated with subdural, subarachnoid, or even intracerebral hematoma1,4). Because of a high mortality rate (20%) they should be recognized early. On the other hand, spontaneous resolution was also reported in a few literature17). Overall, the natural course of these pseudoaneurysms is well not recognized. The simple presence of a pseudoaneurysm is an indication for intervention or surgery is also unclear and there are no definite treatment guidelines. We report a case of patient with angiographical progressive change of traumatic pseudoaneurysm for one week and discuss natural course and treatment guidelines.
CASE REPORT
Case 1
A 47-year-old woman with diabetes mellitus presented to the emergency department of our hospital with head and facial injury. The patient was found in collapsed state in the street and could not remember anything. On admission, her mental status was drowsy with Glasgow Coma Scale (GCS) score of 13/15. The 3rd nerve palsy signs of ptosis, extraoculor movement (EOM) limitation and non reactive pupil were shown in left eye.
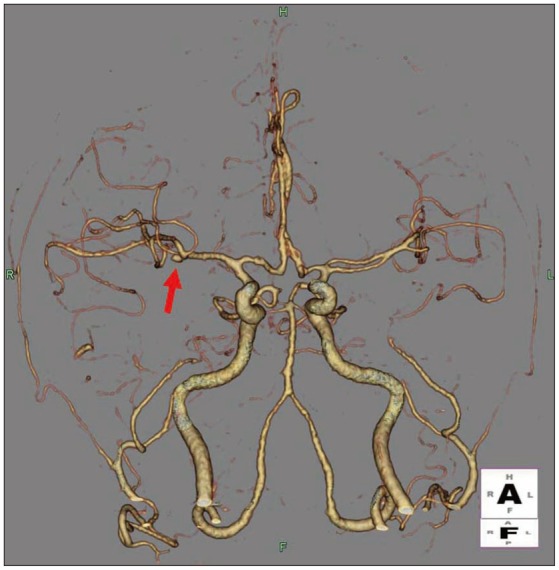
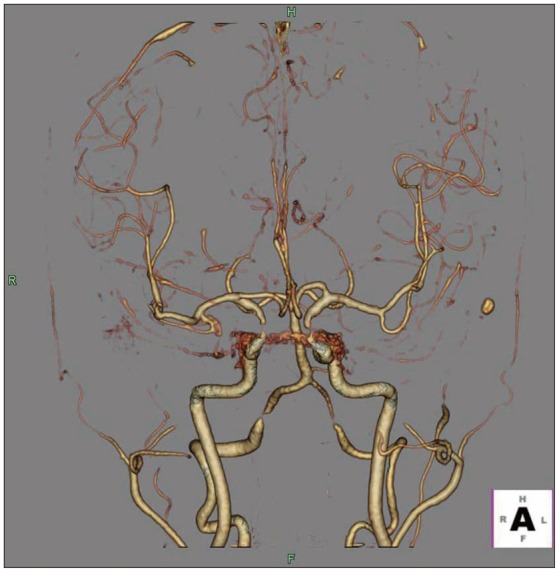
Initial brain computed tomography (CT) revealed a skull fracture, epidural hematoma without mass effect in the right hemisphere and subarachnoid hemorrhage in both sylvian fissures and basal cistern, which were more dominant in left side (Fig. 1). The CT angiogram revealed an aneurysm of right middle cerebral artery bifurcation. We think this one was unruptured aneurysm, because dominance of subarachnoid hemorrhage was definite in left sylvian fissure and basal cistern (Fig. 2).
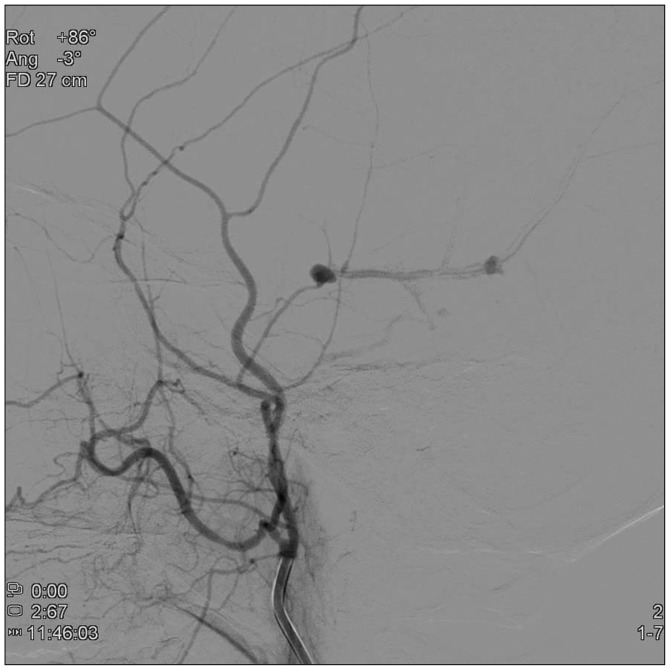
The cerebral angiogram was performed to identify the cause of 3rd nerve palsy or other possible vascular abnormality. There is no intracranial vascular lesion, but two pseudoaneurysms arising from the right MMA adjacent to the fracture line of temporal bone were found (Fig. 3).
This MMA pseudoaneurysm was presumed to be related to the temporal bone fracture and was probably the cause of the epidural hematoma. The 3rd nerve palsy was thought to be traumatic isolation palsy. The patient was managed conservatively with steroid and remained clinically stable.
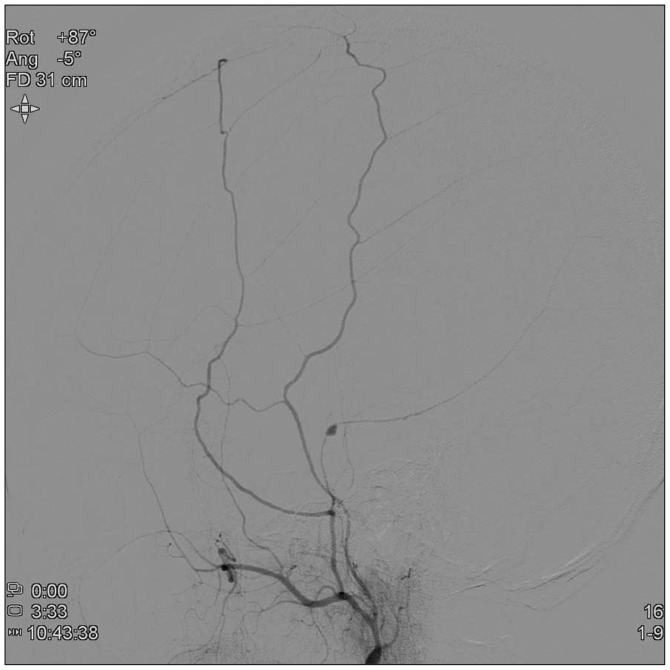
After 1 week, cerebral angiogram was repeated to re-evaluate the pseudoaneurysm and to determine the treatment plan. The angiogram showed that the one pseudoaneurysm changed more aggravating appearance. The initially found distal pseudoaneurysm is collapsed, and another aneurysm was found more aggravating appearance (Fig. 4). We think that the aggravating change or rupture risk is higher than spontaneous thrombosis. In addition, the prognosis in traumatic pseudoaneurysms has been reported to be generally poor, immediately, the treatment was planned. The right external carotid artery and then the posterior branch of right MMA were selectively catheterized. Endovascular embolization for the posterior branch with glue was performed. The glue that we used was histoacryl mixed with lipiodol. The amount of histoacryl was 0.5 cc, and the ratio of histoacryl and lipiodol was 1 : 3.
After embolization, selective injections of the right external carotid artery and the right MMA showed normal filling of the MMA except posterior branch and no filling of the pseudoaneurysm (Fig. 5).
The patient was discharged from the hospital with no neurologic deficits except 3rd nerve palsy. A 3-month follow-up, ptosis and EOM was mild improved and CT showed complete resolution of epidural hematoma.
Case 2
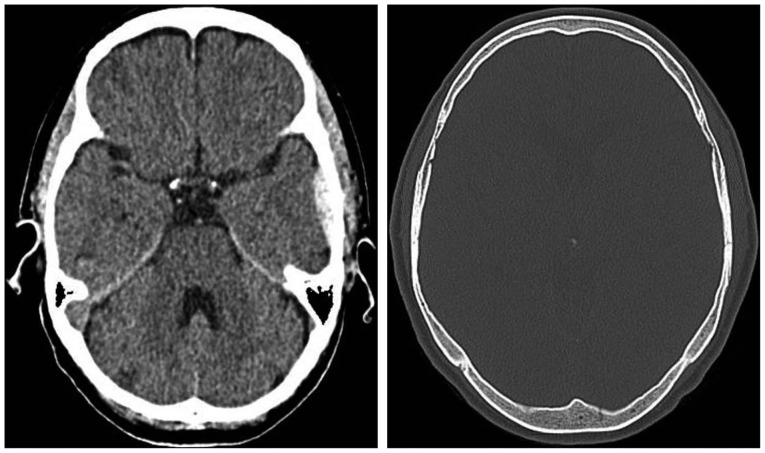
A 70-year-old woman presented to the emergency department of our hospital with head injury. The patient slipped down in the street and had loss of consciousness. On admission, the patient with scalp contusion was alert and GCS score was 15/15 without any neurologic deficit. The patient complained headache and nausea. Initial brain CT revealed a skull fracture, epidural hematoma without mass effect in the left temporal area (Fig. 6). The CT angiogram showed bilateral internal carotid artery stenosis (Fig. 7).
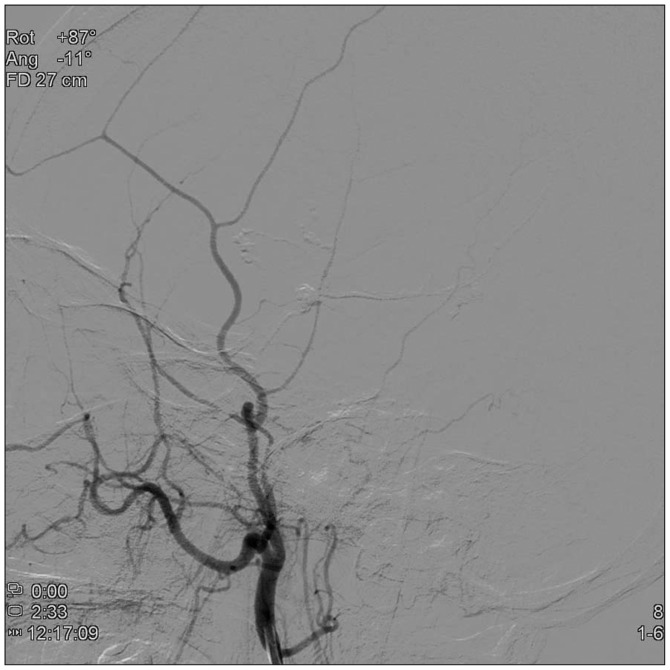
The cerebral angiogram was performed to evaluate carotid stenosis or other vascular abnormalities. There were right vertebral artery stenosis, and a pseudoaneurysm arising from the left MMA (Fig. 8).
After 1 week, we performed cerebral angiogram to re-evaluate the pseudoaneurysm and determine the treatment plan. The pseudoaneurysm changed to more aggravating appearance (Fig. 9), need to be treated. We catheterized the left external carotid artery then the posterior branch of left MMA. Endovascular embolization for posterior branch of left MMA with glue was performed. The glue that we used was histoacryl mixed with lipiodol. The amount of histoacryl was 0.5 cc, and the ratio of histoacryl and lipiodol was 1 : 3. After embolization, selective injections of the left external carotid artery and the left MMA showed normal filling of the MMA except posterior branch, and no filling of the pseudoaneurysm (Fig. 10).
The patient was discharged with no neurologic deficits, and a 2-month follow-up, the brain CT showed much resolved epidural hematoma.
DISCUSSION
Aneurysms of the MMA are very rare phenomena and known to be of 2 types : the true aneurysm and the pseudoaneurysm4). The true aneurysm is usually accompanied with other pathologic conditions such as Paget disease, hypertension, meningioma, and dural arteriovenous malformations and has the same histologic characteristics that is presented in intracranial cerebral aneurysms6,13,14,16). Pseudoaneurysms, on the other hand, are associated with a head trauma causing a tear in the arterial wall in most cases4). About 70-90% of cases of traumatic MMA pseudoaneurysm are associated with a fracture crossing the MMA or one of its two branches in the temporal region7). In a histologic perspective, there is only fibroconnective tissue or hematoma surrounding, covered the hole in the wall, thus forming a pseudoaneurysm. Generally, none of the normal arterial layers are present in the pseudoaneurysm4).
Traumatic pseudoaneurysms show specific characteristics on angiography, which include peripheral location, absence of neck, sometimes irregular shape. Its filling and emptying are delayed and very slow during angiogram, which means that the contrast medium has time to settle at the bottom of the aneurysm and the pre- and post-aneurysmal segments of the meningeal artery are not opacified at the same time. These features explain why traumatic meningeal pseudoaneurysms are usually visible only in the late injection stages of selective external carotid angiography5,8,9).
Usually, meningeal pseudoaneurysms are known to present with acute or delayed epidural hematoma, but occasionally, they can also be associated with subdural, subarachnoid, or intracerebral hemorrhage1,4). The natural evolution of these lesions is not clear. But in some reports, progressive change of traumatic aneurysms has been demonstrated on repeated angiograms8,11). Spontaneous thrombosis of MMA pseudoaneurysm is a rare event that has been reported before by Namba et al.12) One possible mechanism of progressive change is that initially, a small tear which is not large enough to result in an epidural hematoma is occurred in the meningeal artery. And formation of clot that contains further leakage of blood is created, then recanalize and form a false lumen. This pseudoaneurysm gradually enlarge and can be ruptured8,10). This pseudoaneurysm tends to be ruptured in a delayed fashion, resulting in an intracranial hematoma and clinical deterioration. This series of events has been reported with meningeal pseudoaneurysms in which the patients typically recovered completely after the initial trauma but deteriorated clinically in a delayed fashion from secondary rupture of the pseudoaneurysm after initial tear of the arterial wall2,5).
Based on review of literatures, the true frequencies of these pseudoaneurysms are unclear. The simple presence of a pseudoaneurysm is an indication for intervention or surgery is also unclear. Because only a few cases of MMA pseudoaneurysms has been reported in the literature and the incidence of incidental pseudoaneurysms is essentially unknown, there are no definite treatment guidelines, yet. Some authors recommend that treatment be carried out without any delay because of the risk of secondary rupture4). Some author presented spontaneous thrombosis of pseudoaneurysm17).
In our patients, conservative management and observation were performed for the one week and then the pseudoaneurysms were re-evaluated on conventional angiogram; however, revealed that the one pseudoaneurysm changed more aggravating appearance and the other was only mildly improved. We carefully think that the aggravating change or rupture risk is higher than spontaneous thrombosis. In addition, the prognosis in traumatic pseudoaneurysms has been reported to be generally poor. A mortality rate of 20% has been reported in the literature4). Therefore, considering the risk of a secondary rupture and poor prognosis, we suggest that the treatment of traumatic pseudoaneurysms should be performed without delay.
CONCLUSION
Although the incidence of traumatic MMA pseudoaneurysm is rare, it should be considered possibility of meningeal pseudoaneurysms in cases of head trauma, especially if the fracture crosses the expected location of the middle meningeal artery. Because this pseudoaneurysm may have aggravating course and secondary bleeding, we suggest it should be treated as soon as possible.