INTRODUCTION
Oblique basal skull fractures involving both clivus and occipital condyle are uncommon and typically result from high impact lateral crushing injuries. In addition, basal skull fractures may cause multiple cranial nerve deficits and vascular complications due to the tight neural and vascular entry and exit routes present in this region6,8). However, the diagnosis of basal skull fracture is difficult by routine cranial radiography due to the presence of radiographically dense petrous temporal bones, and presumably, this explains the small number of cases described in the literature. Nonetheless, modern imaging modalities are capable of providing a diagnosis of basal skull fractures and potential cranial injuries. Here, we report a unique case of basal skull fracture, involving both the clivus and occipital condyle that presented with sixth and contralateral twelfth cranial nerve palsies. Diagnosis was easily diagnosed by 3-dimensional computed tomography (CT). We discuss the CT characteristics and clinical findings of this case, and the courses of cranial nerve deficits.
CASE REPORT
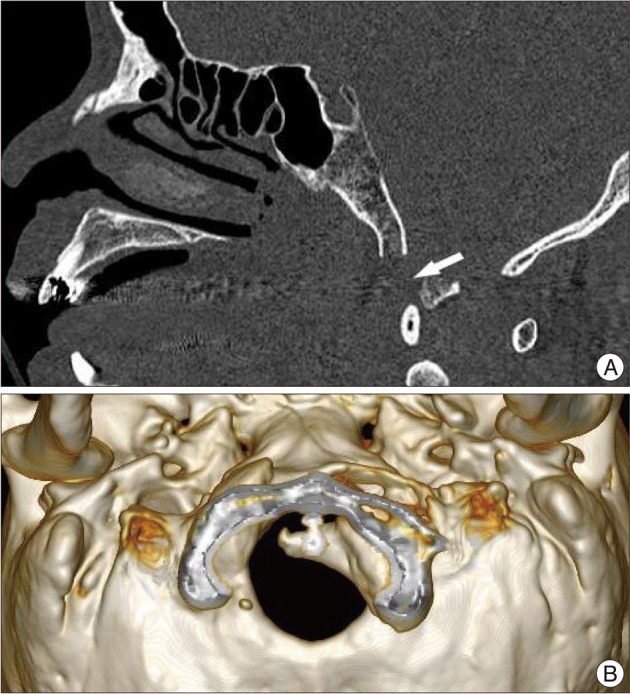
A 45-year-old male patient who sustained major cranial injuries following a high-speed motorcycle accident was referred to our emergency room. On initial examination, he was alert and fully oriented, and there was no evidence of otorrhea, rhinorrhea, or hematorrhea. However, a detailed neurological examination revealed right VI and left XII cranial nerve deficits (Fig. 1), and a CT scan revealed a fracture line extending obliquely through the clivus and an avulsion fracture of the occipital condyle (Fig. 2). CT also showed massive pneumocephalus with air ventricles, but no shift of the midline structure was evident. Clinically, the patient remained awake, alert, and oriented without hemiparesis, and non-operative supportive treatment was administered. A repeat CT scan 10 days after presentation demonstrated complete resolution of the pneumocephalus, and a neurological examination performed at three months after presentation revealed partial improvement of right VI cranial nerve function but an unchanged XII cranial nerve deficit.
DISCUSSION
Basal skull fractures account for 21% of all skull fractures and occur in 4% of all head injury cases4). Historically, fractures of the skull base have most often been identified based on clinical findings, such as, cranial nerve palsies and cerebrospinal fluid leaks.
These fractures are difficult to diagnose by simple radiography, and reportedly are only identified in 20% of cases5,7). However, due to the ever-increasing sophistication of CT imaging, including three-dimensional reconstruction, trauma surgeons can now rapidly diagnose basal skull fractures and related cranial injuries. The skull base contains a number of areas where bones are weak and through which fractures tend to extend. These areas include the internal and external auditory canal, middle ear, carotid canal and foramen lacerum, jugular foramen, hyoglossal canal, occipital condyle, and foramen magnum9). Pneumocephalus is an important condition to be vigilant of, along with symptoms of increased intracranial pressure, such as, anisocoria, hemiparesis, and signs of meningeal irritation2). Cranial nerve injury is another serious complication of basilar skull fractures3). Frontobasal fractures generally injure olfactory or optic nerves, whereas cranial nerve palsy of nerves III, IV, V, and VI have been reported for fractures involving the cavernous sinus and superior orbital fissure, because these nerves exit the skull base through the superior orbital fissure. In particular, for fractures of the skull base, the long intracranial course of the sixth nerve renders it particularly susceptible to injury. As mentioned above, CN VI may be damaged in the superior orbital fissure and is classically accompanied by CN III and CN IV palsies. However, in the described case, right VI nerve palsy was associated with a clivus fracture without fracture of the right side of the superior orbital fissure. Furthermore, vertical movement of the brain stem during trauma may stretch or avulse the nerve on leaving the pons in the absence of a fracture of the superior orbital fissure. Treatment is conservative and in most cases, abducens nerve injury recovers spontaneously after approximately 4 weeks. The glossopharyngeal, vagus, and spinal accessory nerves exit the skull base in the jugular foramen, whereas the hypoglossal nerve passes though the hypoglossal foramen just medial to the jugular foramen. Palsies of nerves IX, X, XI, and XII have been reported in patients with basal skull fractures, especially in patients with occipital condyle fractures. Three types of occipital condyle fractures have been described by Anderson and Montesano1). In the described case, the fracture was believed to be an avulsion fracture of the occipital condyle by the alar ligament injury, which corresponded to a type III occipital condyle fracture, and caused depression into the foramen magnum resulting in XII nerve palsy.