INTRODUCTION
Spinal cord lipomas are rare and account for about 1% of all spinal cord tumors2,4,6,7,8,10,11,12,16,17,18). They are usually associated with lumbo-sacral spinal dysraphism, and these lesions extend to the subcutaneous tissue through a defect in the posterior elements of the spine. Non-dysraphic spinal cord lipomas are rare tumors of the spinal cord2,4,6,7,8,10,11,16).
CASE REPORT
A 49-year-old male patient who was suffering from aggravation of posterior neck pain, numbness in the left hand, pain in the left lower limb, and gait disturbance since 3 years visited our out-patient department. He had been diagnosed as having non-dysraphic cervical intradural lipoma and was operated in August 1990. This case was previously reported15).
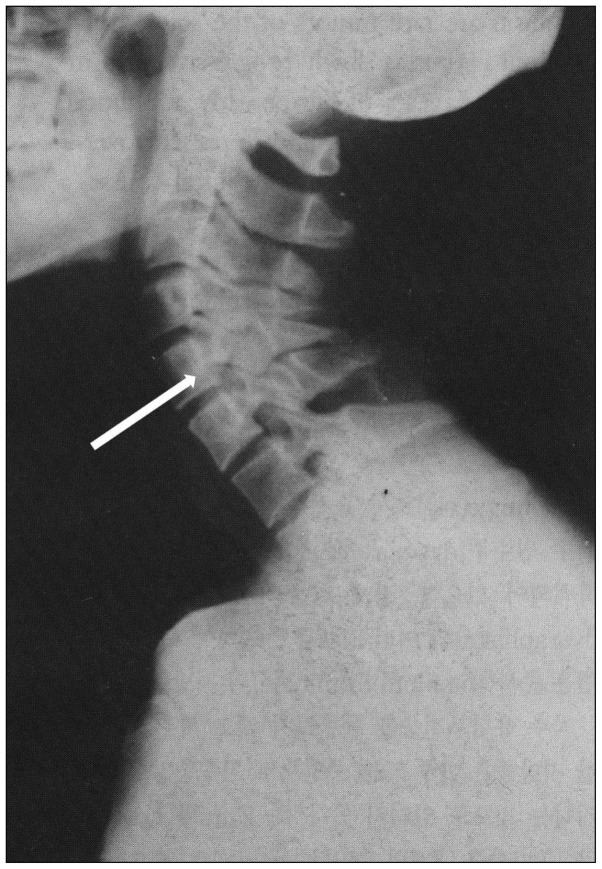
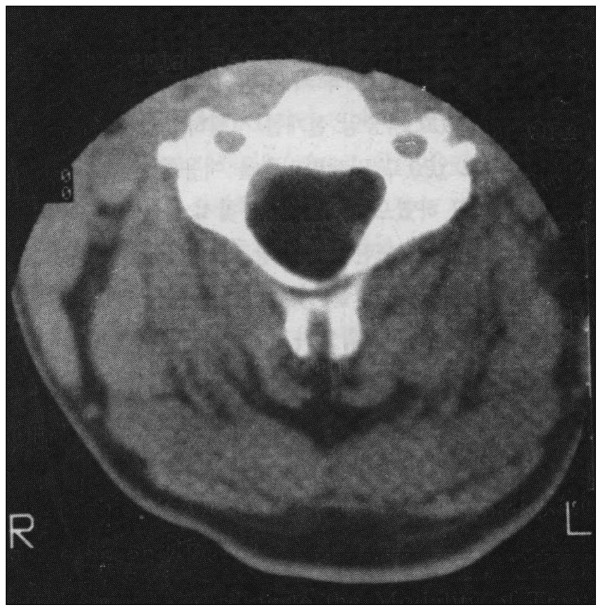
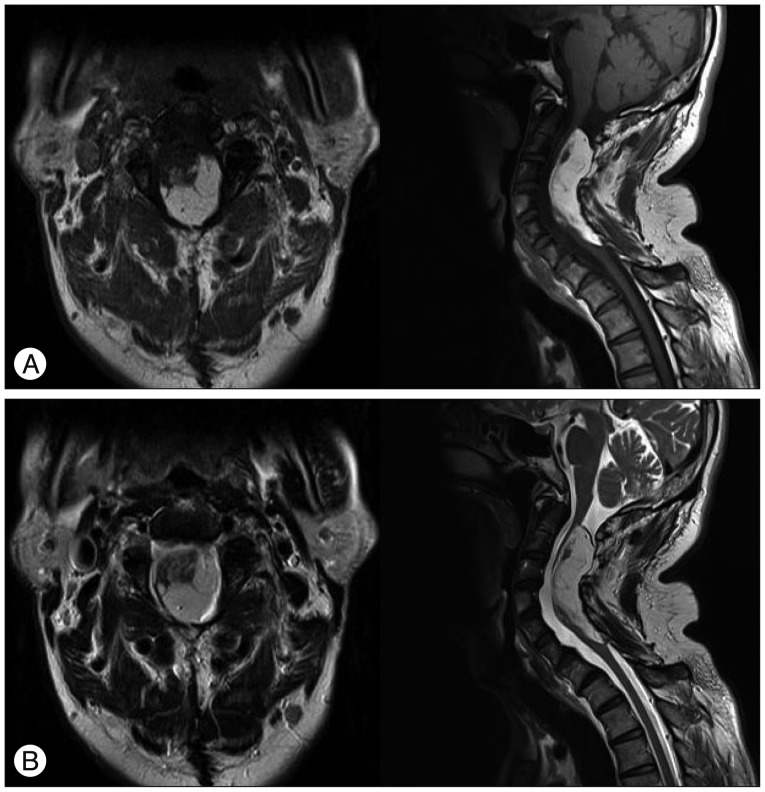
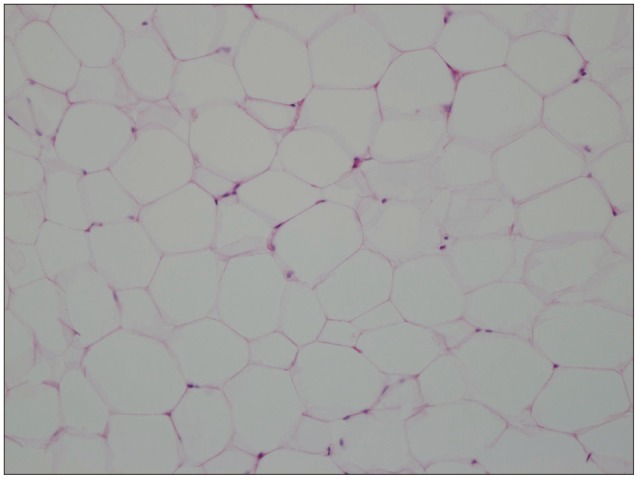
We had reviewed the patient's previous chart since he re-visited our out-patient department. According to the previous chart, he had been suffering from posterior neck pain for one year, and at that time, there were no neurologic symptoms except for neck pain. Physical examination did not reveal any stigmata such as dimples, hair, fistula, or any masses on his vertebral column. Previous preoperative cervical plain film images showed severe cervical lordosis and increased anteroposterior diameter of the spinal canal (Fig. 1). Previous computed tomography (CT) and magnetic resonance imaging (MRI) images showed a huge lipomatous mass, which was located intradurally and it encircled and compressed the spinal cord from the C2 to C7 level (Fig. 2, 3). Although he was neurologically intact, we performed adequate debulking of the lipomatous mass with subtotal laminectomy from the C2 to C7 level in order to prevent neurological deterioration. Histopathological examination showed mature and uniform adipose cells without any cellular pleomorphism, suggesting the diagnosis of a benign lipoma.
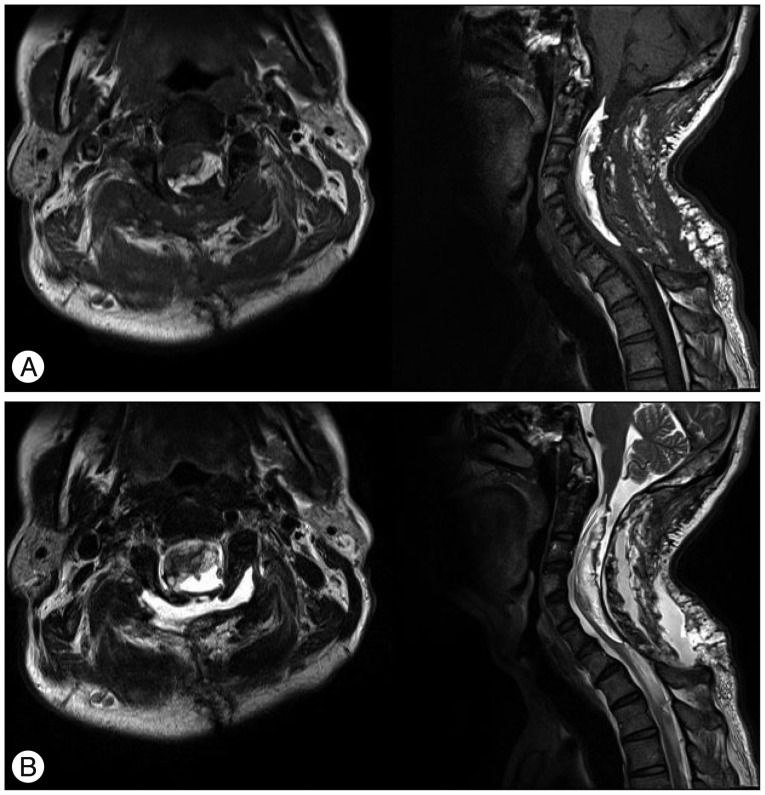
When the patient re-visited our outpatient department, neurological examination showed slightly decreased motor power in the left lower limb (MRC grade 4/5), numbness in the left hand along the C6 and C7 dermatomes, and posterior neck pain radiating to the left shoulder. On radiologic examination, we found regrowth of the lipomatous mass from the C2 to C7 level, which encircled and compressed the cervical spinal cord. Previous subtotal laminectomy from C2 to C7 and severe cervical lordosis were also observed (Fig. 4, 5).
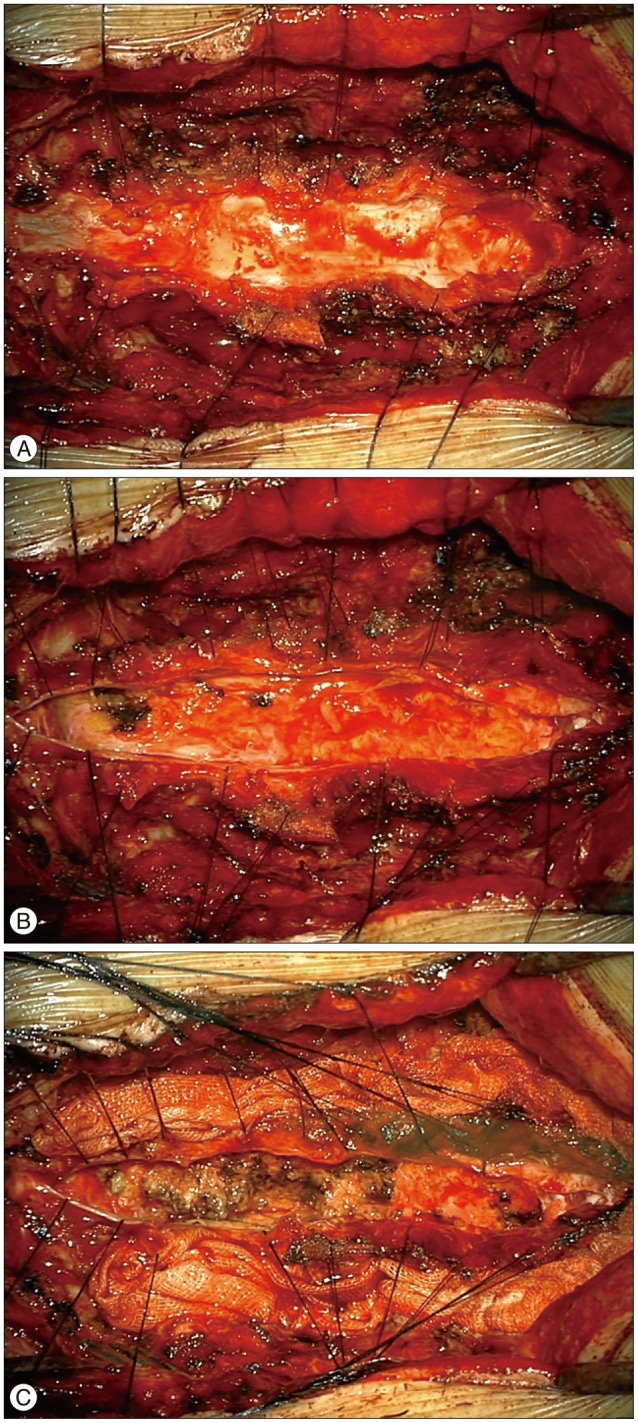
We performed subtotal laminectomy of C1 in order to identify the normal elements of cervical dura because there were severe adhesions between paraspinal muscles, soft tissues and cervical dura. After that, we could perform dissection of the previous adhesions and could identify the cervical dura (Fig. 6A). When the dura was opened, we found a huge, yellowish mass in the intradural space, which encircled and compressed the cervical spinal cord (Fig. 6B). We performed subtotal debulking of the lipomatous mass using ultrasonic tissue ablation system paying careful attention to signals of intraoperative neurophysiological monitoring (IONM). There were no complications during IONM in the intraoperative course. We performed an adequate decompression of the spinal canal, and therefore we could suture the dura watertightly without duraplasty (Fig. 6C). On the postoperative day 2, we found a cystic mass at the surgical site and it had gradually increased in size. On MRI, the cystic mass showed low signal intensity on T1-weighted images and high signal intensity on T2-weighted images; it suggested the presence of cerebrospinal fluid (CSF) (Fig. 7). We gently aspirated the cystic mass with a 24 gauge needle attached to the syringe, and then the surgical site was continuously compressed. After that, the cystic mass spontaneously disappeared. Histopathologic examination showed mature adipose tissue and fibrous tissue without cellular pleomorphism, suggesting the diagnosis of a benign lipoma (Fig. 8).
We are following up the patient for 24 months at the out-patient department, and his neurological symptoms have improved.
DISCUSSION
Spinal cord lipomas are usually associated with spinal dysraphism, and they account for 1% of all spinal cord tumors. The number of non-dysraphic spinal cord lipomas is less than that of dysraphic spinal cord lipomas, and they are usually located intradurally. Thus, they usually do not present as subcutaneous lesions3,10,18). In this case, according to the previous chart, there were no subcutaneous lesions on the patient's vertebral column.
Non-dysraphic intradural lipomas are commonly located in the thoracic spine; like our case, non-dysraphic cervical intradural lipomas account for only one-seventh or one-eighth of the spinal cord lipomas8,9). Most of these lipomas are found in the posterior part of the spinal cord, and they usually distort and expand the spinal cord. In our case, we could observe increased anteroposterior diameter of the cervical spinal canal (Fig. 1). Most of these lipomas are subpial or juxtamedullary in location, and hence true intramedullary lipomas are very rare with only a few cases having been reported in the literature2,10,11). In this case, the radiologist deciphered that the lipomatous mass was juxtamedullary in location, and we were also able to identify the mass in that location.
About half of the patients who had spinal cord lipomas developed neurologic symptoms during their young adult age, and approximately one-fourth of the patients were in their childhood years and above 40 years of age2,8,10). Neurologic symptoms usually present in the form of myelopathies such as radiating pain, weakness or numbness in limbs of patients in the young adult age group. The symptoms are often delayed and they worsen gradually. Unfortunately, most of the patients suffer from spinal cord lipomas for 2 years before visiting the hospital2,8,10,13). Kabir et al.10) stated that most of the patients who have cervical cord lipomas take more than 10 years for seeking medical advice. It took approximately 20 years for the development of neurologic symptoms in our patient after the initial operation.
Since Elsberg et al.5) reported about the danger associated with total removal of spinal cord lipomas, which caused postoperative quadriplegia in 1925, many authors have changed their management strategy from conservative care to operation. Recently, several authors agree that proper treatment of these lesions includes surgical removal using microsurgical techniques with IONM in order to preserve the normal neurological tissues2,6,10,12,14,16,17). Adequate bony decompression is also recommended. Although many authors have mentioned and performed duraplasty, it is still controversial whether surgeons should perform duraplasty in all of the patients10,12). In our case, as described above, we mentioned that we could perform watertight closure of the cervical dura without duraplasty after subtotal debulking. Although CSF leakage occurred as an acute postoperative complication, we cautiously concluded that lack of duraplasty is not the reason for development of this complication. On reviewing the literature, we could not find the same complication in patients with similar disease; thus further studies are required to determine whether surgeons should perform duraplasty in all of the patients.
Meanwhile, the relationship between growth of these lesions and lipid metabolism was reported and debated by many authors1,2,6,10,14,16). Fleming et al.6) described 5 cases of non-dysraphic pediatric intramedullary spinal cord lipomas in 2010; they reported 2 cases of recurrence, and re-operation was needed in these 2 cases. They suspect that the number of adipocytes within non-dysraphic spinal cord lipomas can increase over time. Pruthi et al.16) reported their experience with eight cases of non-dysraphic intradural lipomas in 2010, and they suggested that the spinal cord lipomas are not associated with obesity and metabolism of body fat. Our patient was thin and his weight had not changed since the time he underwent surgery in 1990. Furthermore, there was no increase in the lipid level on serum analysis. All of the authors had a similar opinion that further clinical and experimental studies are necessary for confirming the conclusions. To the best of our knowledge, only a few articles have reported regarding regrowth of cervical intradural lipomas6,14,16). Therefore, more studies are needed to understand the relationship between regrowth of cervical intradural lipomas and lipid metabolism.