Choi, Kim, Lim, Yoon, Yoon, and Yoon: Propofol Infusion Associated Metabolic Acidosis in Patients Undergoing Neurosurgical Anesthesia: A Retrospective Study
Abstract
Objective
Propofol and volatile anesthesia have been associated with metabolic acidosis induced by increased lactate. This study was designed to evaluate changes in pH, base excess (BE), and lactate in response to different anesthetic agents and to characterize propofol infusion-associated lactic acidosis.
Methods
The medical records of patients undergoing neurosurgical anesthesia between January 2005 and September 2012 were examined. Patients were divided into 2 groups : those who received propofol (total intravenous anesthesia, TIVA) and those who received sevoflurane (balanced inhalation anesthesia, BIA) anesthesia. Propensity analysis was performed (1 : 1 match, n=47), and the characteristics of the patients who developed severe acidosis were recorded.
Results
In the matched TIVA and BIA groups, the incidence of metabolic acidosis (11% vs. 13%, p=1) and base excess (p>0.05) were similar. All patients in the TIVA group who developed severe acidosis did so within 4 hours of the initiation of propofol infusion, and these patients improved when propofol was discontinued.
Conclusions
The incidence of metabolic acidosis was similar during neurosurgical anesthesia with propofol or sevoflurane. In addition, severe acidosis associated with propofol infusion appears to be reversible when propofol is discontinued.
Key Words: Acidosis ┬Ę Neurosurgery ┬Ę Propofol.
INTRODUCTION
Propofol infusion syndrome (PRIS) is rare and often fatal. Its initial indicators include new onset metabolic acidosis and cardiac dysfunction, and PRIS is diagnosed at the appearance of new onset rhabdomyolysis, hypertriglyceridemia, and/or renal failure 6,14). PRIS was first described in critically ill children undergoing prolonged high-dose propofol infusion 18). The overall incidence of PRIS was reported to be 9% in long-term sedated patients in the intensive care unit 4), and 6% in patients with severe head trauma 17). A prospective multicenter study involving 1017 adults reported a PRIS incidence of 1.1%, despite dose guidelines of <83 ┬Ąg/kg/min of propofol 14). In addition, short-term (average, 4.9 hours) high-dose propofol infusion during craniotomy reduced the average base excess (BE) and increased lactate concentrations in pediatric patients 17). Propofol infusion-associated metabolic acidosis is characterized by increased lactate concentrations. Although PRIS has not been observed in adults receiving prolonged propofol anesthesia, propofol infusion-associated metabolic acidosis has been observed in 6 adult 1,2,9,10,11,16,19) and 4 pediatric 7,8) patients anesthetized with propofol 7,8). Propofol infusion-associated metabolic acidosis may be a precursor of PRIS. Notably, lactic acidosis occurred in 9 of the 10 patients who experienced propofol infusion-associated metabolic acidosis, suggesting that lactic acidosis may be an early marker of PRIS 8,9). Moreover, the incidence of subclinical metabolic acidosis was higher in patients receiving low-dose propofol compared to those not infused with propofol, suggesting that care should be taken in patients who are administered propofol 3). However, a more recent study reported that volatile anesthesia was also associated with increased lactate levels 15). Given its ability to decrease intracranial pressure, propofol has been used widely for neurosurgical operations, especially operations involving brain tumors or cerebrovascular diseases, which require prolonged and high doses of infused propofol. However, volatile anesthetics are also acceptable components of most anesthetic regimens for neurosurgery. These observations, regarding the association of metabolic acidosis with propofol infusion, were the basis for the present study on patients undergoing neurosurgical anesthesia with prolonged and high-dose propofol infusion. This study was designed to evaluate changes in pH, BE, and lactate concentration in patients who received different anesthetic agents and to assess the characteristics of patients who experienced severe acidosis.
MATERIALS AND METHODS
This chart review study was performed at hospital and was approved by the Institutional Review Board (H-1008-143-330). The medical records of patients undergoing elective cerebral vascular surgery or brain tumor surgery between January 2005 and September 2012 were assessed retrospectively. Only patients with initially alert mentality were included. None received propofol during the pre-anesthetic period. Preoperative exclusion conditions included diseases in which metabolic acidosis could occur concomitantly or the performance of emergency operations; thus, patients with ASA class III or IV, those in poor general condition (massive bleeding or sepsis), those with pulmonary diseases such as asthma and chronic obstructive pulmonary disease, and those with drug intoxication were excluded. Intraoperative exclusion conditions included pre-existent acidosis on initial arterial blood gas analysis (ABGA) and events associated with tissue hypoxia-induced lactic acidosis, including hypotension, inadequate arterial saturation or a sudden decrease in hemoglobin <7 g/dL, and massive bleeding [transfusion of >10 units of packed red blood cells (pRBC) or estimated blood loss >70 mL/kg]. Only 1 case was included if the patient underwent anesthesia more than once during the study period.
We assessed the patients' baseline demographic and clinical characteristics; comorbidities including hypertension, diabetic mellitus, ischemic heart disease, cardiac disease, and cerebrovascular disease; medications including steroids and mannitol; and preoperative laboratory findings. Patients undergoing neurosurgery were anesthetized with either propofol or sevoflurane, under the discretion of the attending anesthesiologists, and were divided into 2 groups based on the primary anesthetic : propofol (total intravenous anesthesia, TIVA) or sevoflurane (balanced inhalation anesthesia, BIA).
Target-controlled infusion (TCI) was used for TIVA. A commercial TCI pump (Orchestra┬« Base Primea, Fresenius Vial, Brezins, France) was used for the effect-site TCI of propofol (50 mL Fresofol 2% inj.; Fresenius Kabi, Graz, Austria) and remifentanil (1 mg UltivaŌäó inj.; GlaxoSmithKline, Rixensart, Belgium), by using infusion models for propofol and remifentanil 12). General anesthesia was maintained with a bispectral index (BIS) value of 40-60 by using a TCI device that was adjusted to deliver target effect-site concentrations (Ce) of 3.5-5 ┬Ąg/mL propofol and 3-6 ng/mL remifentanil at final steady-state infusion rates of 5-15 mg/kg/h and 5-20 ┬Ąg/kg/h, respectively. Sevoflurane was used for BIA. Anesthesia was induced by intravenous (i.v.) 1% propofol (2 mg/kg) and was maintained with a BIS value of 40-60 by using a below 1 minimum alveolar concentration of sevoflurane inhalation (end-tidal concentration of 1.2-1.5 volume %) and continuous intravenous infusion via TCI of remifentanil (Ce, 3-6 ng/mL; final steady state infusion rate, 5-20 ┬Ąg/kg/h).
On arrival in the operating room, an invasive arterial catheter was inserted and the first ABGA was performed. After induction of anesthesia, ABGA was performed again within 1 hours and was routinely repeated every 2 hours until the end of surgery. During surgery, the tidal volume was adjusted to achieve normocarbia with the oxygen in air (FiO2 0.5) and was controlled by ABGA. The fluid management protocol during surgery included urine output >1 mL/kg/h, mean arterial pressure >60 mm Hg, and central venous pressure >8 mm Hg by using either crystalloid or colloid, depending on the situation. When the hemoglobin concentration fell below 8 g/dL, pRBCs were transfused according to the discretion of the attending anesthesiologist.
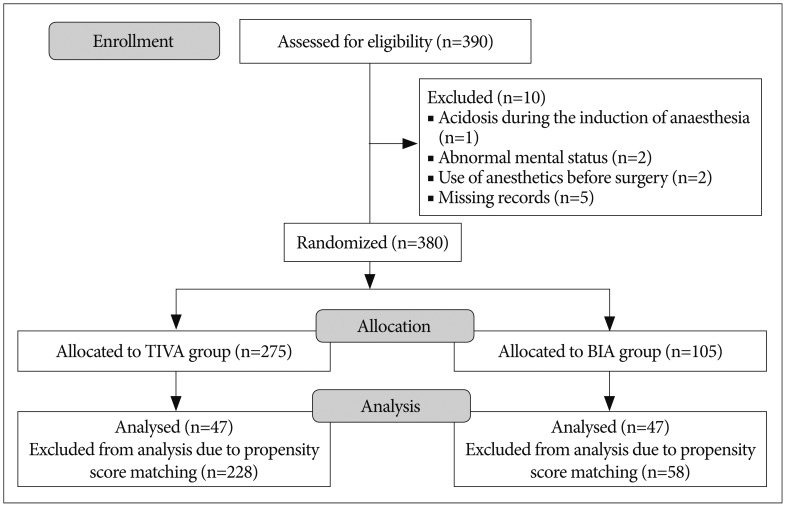
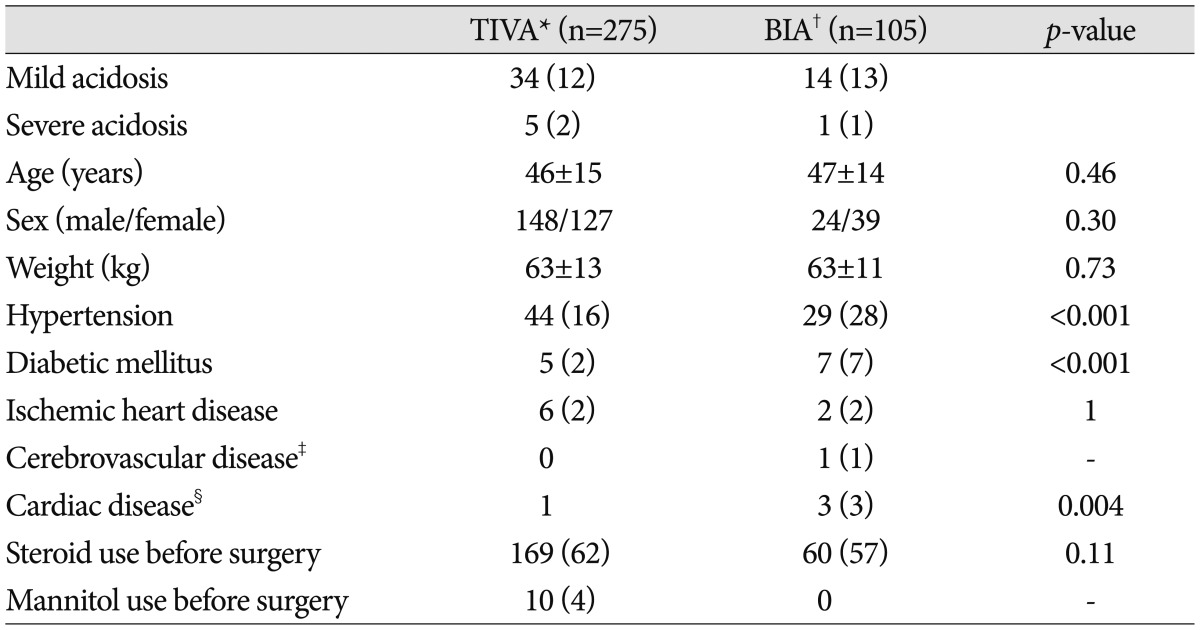
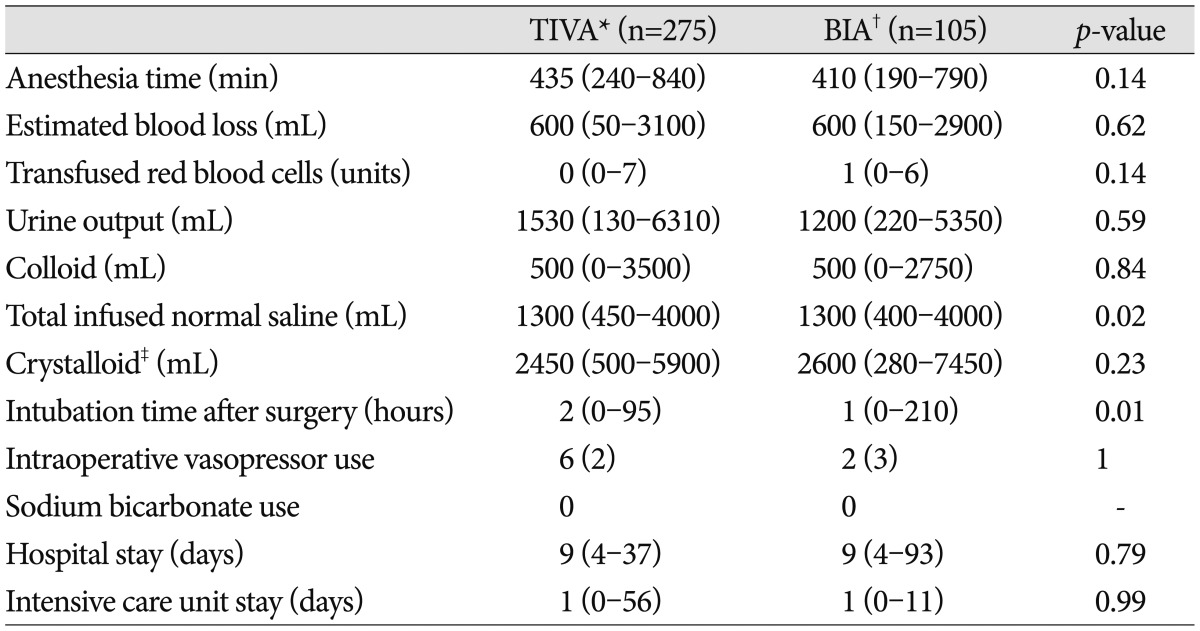
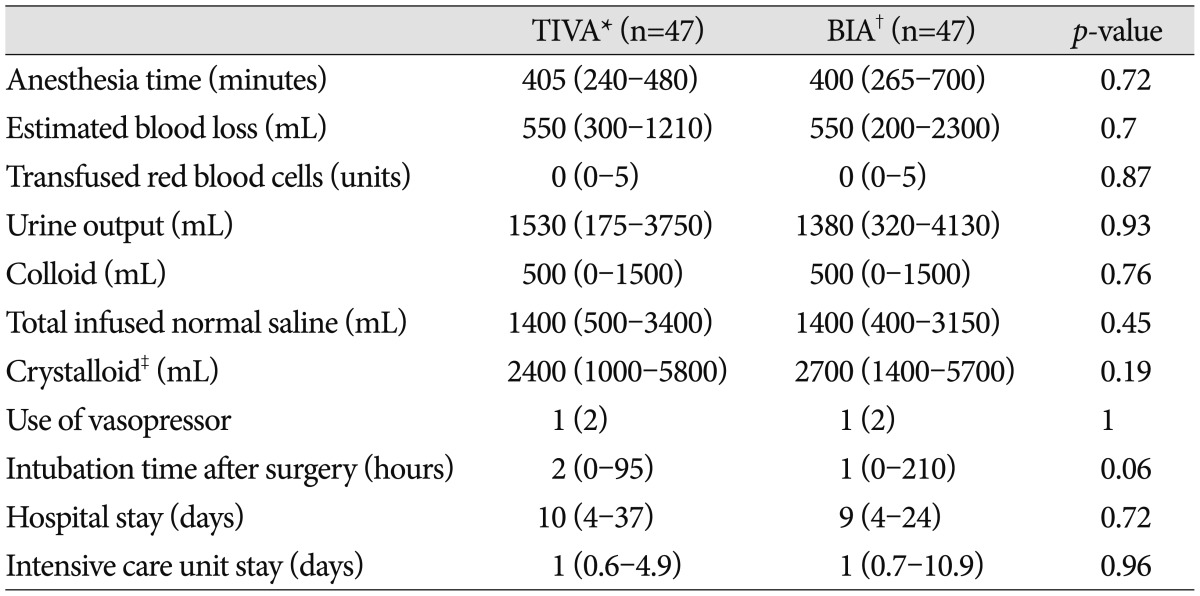
The rates of metabolic acidosis and severe acidosis were determined. Mild metabolic acidosis was defined as an arterial pH <7.35 and BE Ōēż-2 mEq/L or serum lactate Ōēź3 mmol/L 3,5). Although PRIS is characterized by a BE value that is more negative than the aforementioned value, the goal of this study was to detect an early indicator of PRIS (i.e., mild metabolic acidosis). In addition, the initial BE was -2 to -3 mEq/L in several of the case reports regarding PRIS. Severe metabolic acidosis was defined as an arterial pH <7.30 and a BE Ōēż-8 mEq/L or serum lactate Ōēź8 mmol/L 2,10,16). Patients were classified as having metabolic acidosis even if they recovered with the next ABGA. A flow diagram of the progression through the study is shown in Fig. 1. Of the 390 patients enrolled, 10 were excluded because of acidosis during the induction of anesthesia, abnormal mental status, use of anesthetics before surgery, or missing records. Thus, 380 patients were studied who were anesthetized with TIVA (n=275) or BIA (n=105) between January 2005 and September 2012. All covariates that could cause metabolic acidosis in these patients are shown in Table 1, 2. The characteristics assessed in the TIVA and BIA groups were the serum lactate concentration, anesthesia time, estimated blood loss, units of transfused red blood cells, urine output, total volume of colloid, total infused volume of normal saline, total volume of crystalloid, intubation time, stay in the intensive care unit, and stay in the hospital.
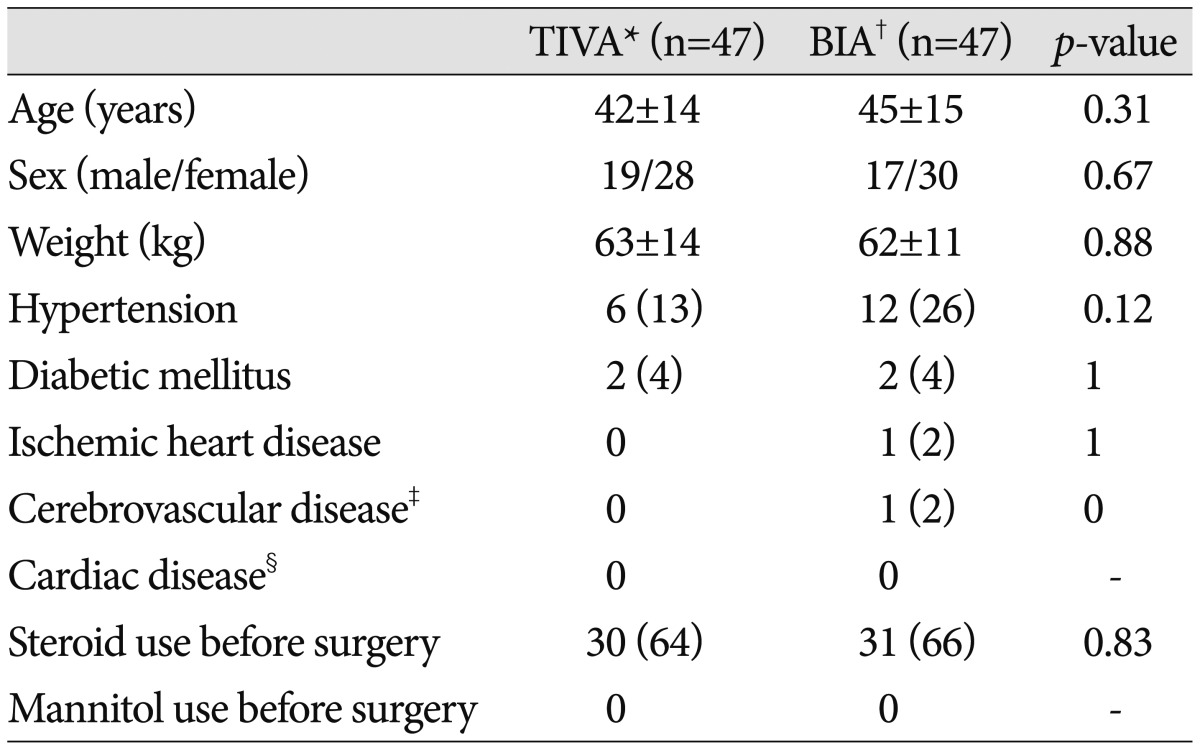
Continuous variables are represented as means┬▒standard deviations or medians (ranges) and categorical variables as numbers (%). Between-group differences in continuous variables were compared by using the Student's t-test or the Mann-Whitney rank-sum test, whereas differences in categorical variables were compared by using the Žć2 test or Fisher's exact test, as appropriate. Propensity score matching was used to minimize selection bias before comparing the TIVA and BIA groups and to evaluate the effects of anesthetic agents alone on neurosurgical anesthesia. The propensity score was defined as the probability of a subject receiving the treatment (in this case, an anesthetic agent) based on the subject's covariate profile. To generate propensity score-matched pairs without replacement, patients in the BIA and TIVA groups were matched 1 : 1. By using this analytic technique, 47 propensity-matched pairs were identified. The effect of anesthetic agents in these matched groups was compared by using the McNemer test. All statistical analyses were performed by using SAS 9.2 (SAS Institute Inc., Cary, NC, USA). p-values <0.05 were considered statistically significant.
RESULTS
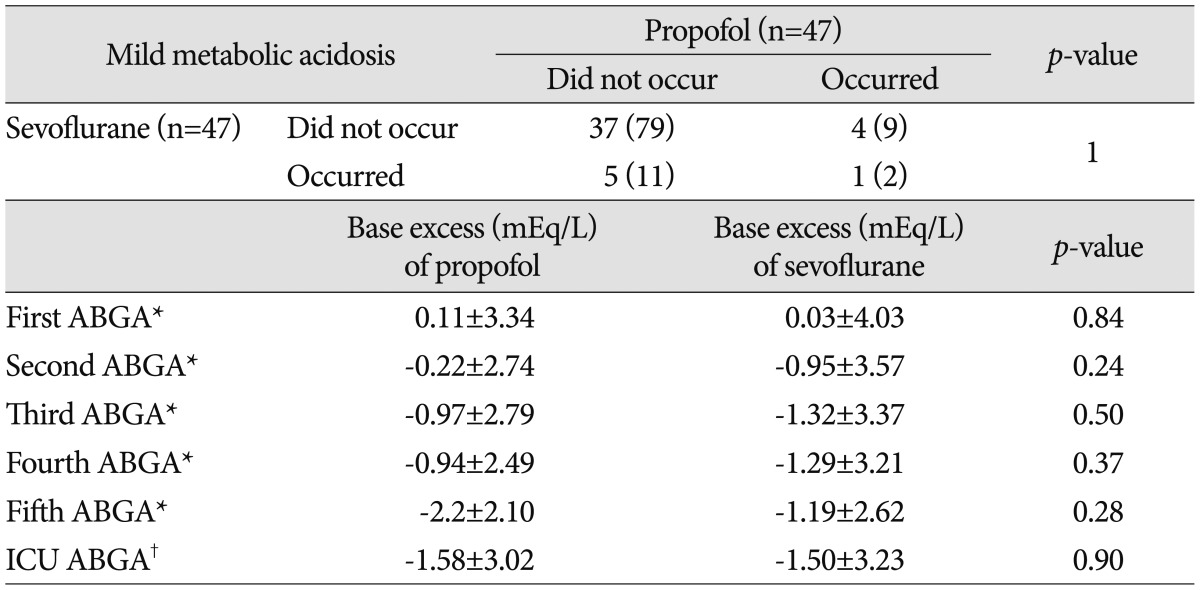
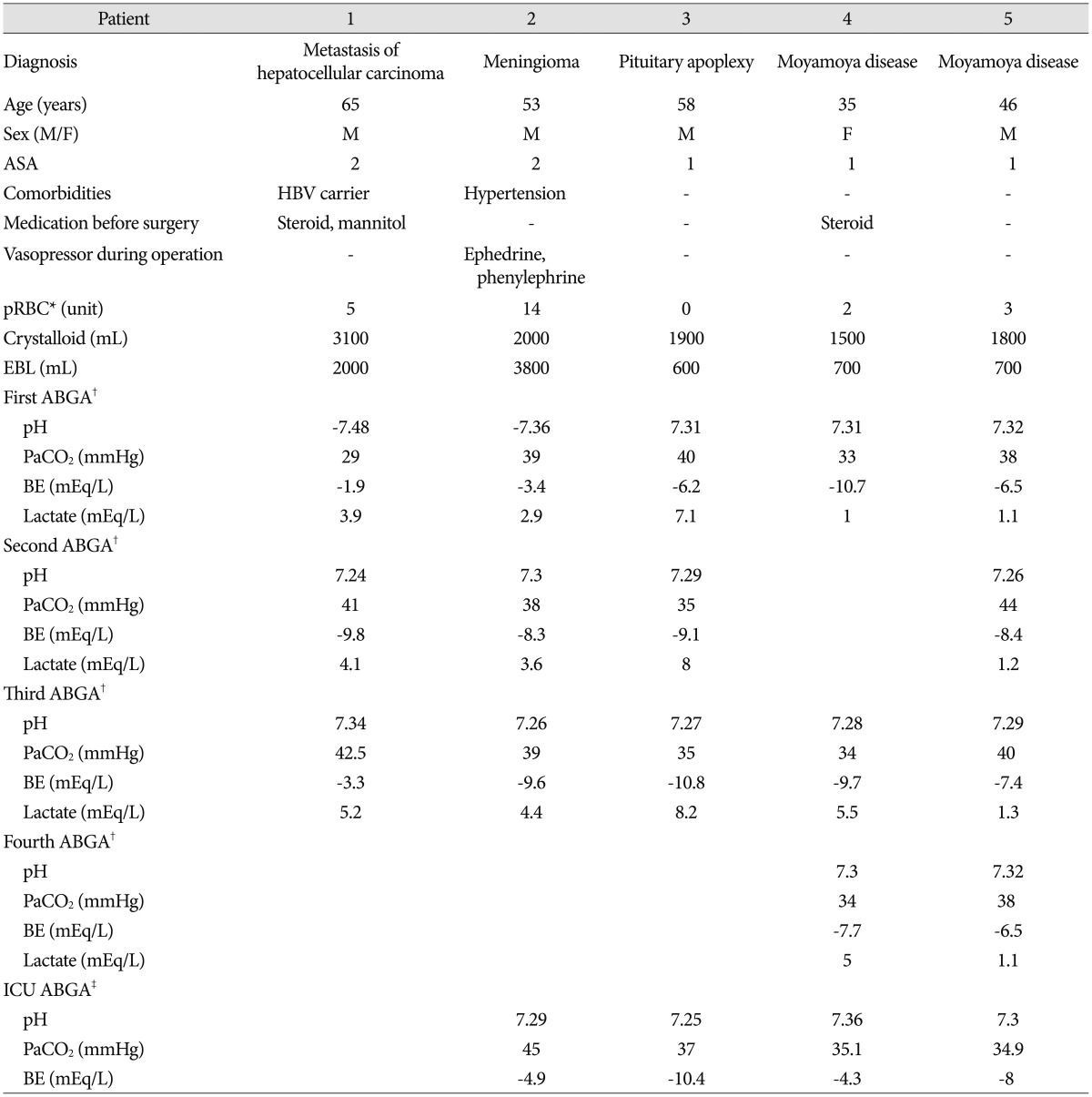
A review of the patient records identified 380 neurosurgery patients who met the inclusion criteria, with 275 patients undergoing TIVA and 105 patients undergoing BIA anesthesia. The preoperative characteristics and the risk factors 3,15,17) of the entire cohort and of the TIVA and BIA groups are shown in Table 1, 2. Using a p-value <0.2 to indicate statistical significance, the following factors differed significantly in the TIVA and BIA groups : the rates of hypertension, diabetic mellitus, cardiac disease, and use of mannitol before surgery, anesthesia time, number of transfused units of red blood cells, total infused volume of normal saline, and intubation time after surgery. Propensity score matching was performed to minimize selection bias before comparing these 2 groups. We identified a propensity-matched subset that consisted of 47 patients each in the TIVA and BIA groups; the perioperative characteristics of these patients are shown in Table 3, 4. The incidence of metabolic acidosis was similar in these 2 matched groups (11% vs. 13%, p=1) ( Table 5); the BE was also similar between these groups. The data from the 5 patients who developed severe acidosis during anesthesia are shown in Table 6. Severe acidosis was detected 2 hours after the induction of anesthesia in patients 1, 3, and 5, and 4 hours after the induction of anesthesia in patients 2 and 4. Immediately upon the detection of severe acidosis, propofol infusion was discontinued in all 5 patients, and the anesthetic agent was changed from TIVA to BIA. All patients recovered from severe acidosis after propofol cessation. None of these patients required additional treatment for cardiovascular collapse or exhibited other cardiovascular symptoms of PRIS.
DISCUSSION
The results of the present study showed that the type of anesthetic agent did not significantly influence the incidence of anesthesia-associated metabolic acidosis in patients undergoing neurosurgical anesthesia.
A study published in 2007 showed that the incidence of subclinical metabolic acidosis was significantly higher in patients receiving low-dose propofol infusion compared to that in patients who did not receive propofol, suggesting that caution should be used whenever propofol is administered 3). However, that study was limited by the lack of an appropriate control group, and by the lack of baseline and continuous ABGA sampling. Moreover, it did not examine critically ill patients or the effect of prolonged high-dose propofol infusion. A second, more recent, study 15) showed that lactate concentrations were higher in patients receiving volatile anesthesia compared to the concentrations in those receiving propofol anesthesia, suggesting that propofol-based general anesthesia is less likely to cause lactic acidosis than is volatile anesthesia. That study was also limited by its retrospective design, making it difficult to rule out other causes of metabolic acidosis in these patients. To our knowledge, the present study is the first to evaluate the effect of anesthetic agents on the incidence of metabolic acidosis. In contrast to the 2 previous studies, our patients received prolonged high-dose propofol infusion and underwent regular surgery 13). Similarly, a study evaluating short-duration high-dose propofol infusion showed that the average BE became significantly more negative, from -0.4┬▒1.3 to -1.3┬▒1.4 mEq/L, and that lactate concentrations also increased significantly 17). However, in that study, only pediatric patients undergoing craniotomy were evaluated, and none of the patients received volatile anesthesia. The reported onset time of PRIS varies. PRIS was initially described in critically ill children receiving long-term (>48 hours) high-dose propofol infusions 18). However, propofol infusion-associated metabolic acidosis has been reported even after short-term administration in pediatric 7,8) and adult 2,10,16) patients receiving anesthesia or sedation in operating rooms or intensive care units. Metabolic acidosis during propofol anesthesia has been reported in 4 adults without risk factors for PRIS, with blood lactate concentrations or the base deficit starting to increase 4 hours after the initiation of propofol infusion 2,10,16). Similarly, most of our patients who experienced lactic acidosis did so within 2-5 hours after the initiation of propofol infusion. Examining lipid metabolism and genetics in patients who experience metabolic acidosis may be important because a key pathogenic mechanism in PRIS appears to be an imbalance between energy demand and utilization. Propofol-associated inhibition of free fatty acid utilization may result in some degradation of the cardiac and peripheral muscles by myocytolysis 18). Therefore, propofol should not be used in patients with inborn errors in mitochondrial fatty acid metabolism. In addition, the increased sympathetic nervous system outflow and elevated cortisol and growth hormone concentrations commonly observed in critically ill patients have been hypothesized to promote lipolysis and fat oxidation, resulting in further increases in free fatty acid concentrations. Liver dysfunction due to circulatory failure or the direct hepatotoxic effects of propofol may also adversely affect lipid kinetics. Finally, lipemia resulting from high-dose propofol infusion can impair mitochondrial oxygen uptake, contributing to the accelerated development and refractory nature of PRIS 13). Therefore, future studies of PRIS should examine the lipid metabolism and/or genetics of the study population. In our study, patient 2 ( Table 6) may have been affected by hemodynamic effects, including transient hypotension or hypovolemia. Further, previous steroid infusion may have influenced metabolic acidosis in patients 1 and 4. However, metabolic acidosis in patients 3 and 5 occurred in the absence of hemodynamic instability, an underlying medical comorbidity, or drugs that could affect metabolic acidosis. Metabolic acidosis due to propofol infusion could not be ruled out definitively even in the other 3 patients (patients 1, 2, and 4). However, the patients who experienced severe acidosis recovered after propofol infusion was stopped, suggesting that early detection of severe metabolic acidosis and discontinuing propofol infusion could correct propofol-induced severe acidosis. This study had several limitations. The BIA group was also given propofol during the induction of anesthesia. However, this dose was small, and propofol was administered only during the induction period, suggesting that this dose of propofol (1% propofol; 2 mg/kg; i.v.) had little effect on our results.
CONCLUSION
In conclusion, propofol infusion may be a leading cause of metabolic acidosis in patients receiving neurosurgical anesthesia. However, volatile anesthesia also may have a similar effect on metabolic acidosis. Assessment of the effects of propofol on metabolic acidosis requires prospective controlled trials.
Acknowledgements
We thank Minkyung Oh, Ph.D., of the Department of Pharmacology, Division of Biostatistics, Inje University Busan Paik Hospital, Busan, Korea, for valuable contributions to our statistical analyses.
This study was performed at Seoul National University.
This work was supported by the Industrial Strategic Technology Program of the Ministry of Knowledge Economy (10041120).
References
1. Betrosian AP, Papanikoleou M, Frantzeskaki F, Diakalis C, Georgiadis G : Myoglobinemia and propofol infusion. Acta Anaesthesiol Scand 2005, 49 : 720,   2. Burow BK, Johnson ME, Packer DL : Metabolic acidosis associated with propofol in the absence of other causative factors. Anesthesiology 2004, 101 : 239-241,   3. Cravens GT, Packer DL, Johnson ME : Incidence of propofol infusion syndrome during noninvasive radiofrequency ablation for atrial flutter or fibrillation. Anesthesiology 2007, 106 : 1134-1138,   4. Cremer OL, Moons KG, Bouman EA, Kruijswijk JE, de Smet AM, Kalkman CJ : Long-term propofol infusion and cardiac failure in adult head-injured patients. Lancet 2001, 357 : 117-118,   5. De Waele JJ, Hoste E : Propofol infusion syndrome in a patient with sepsis. Anaesth Intensive Care 2006, 34 : 676-677,   6. Fudickar A, Bein B, Tonner PH : Propofol infusion syndrome in anaesthesia and intensive care medicine. Curr Opin Anaesthesiol 2006, 19 : 404-410,   7. Haase R, Sauer H, Eichler G : Lactic acidosis following short-term propofol infusion may be an early warning of propofol infusion syndrome. J Neurosurg Anesthesiol 2005, 17 : 122-123,   8. Kill C, Leonhardt A, Wulf H : Lacticacidosis after short-term infusion of propofol for anaesthesia in a child with osteogenesis imperfecta. Paediatr Anaesth 2003, 13 : 823-826,   9. Koch M, De Backer D, Vincent JL : Lactic acidosis : an early marker of propofol infusion syndrome? Intensive Care Med 2004, 30 : 522,   10. Liolios A, Gu├®rit JM, Scholtes JL, Raftopoulos C, Hantson P : Propofol infusion syndrome associated with short-term large-dose infusion during surgical anesthesia in an adult. Anesth Analg 2005, 100 : 1804-1806,   11. Marinella MA : Lactic acidosis associated with propofol. Chest 1996, 109 : 292,   12. Marsh B, White M, Morton N, Kenny GN : Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth 1991, 67 : 41-48,   13. Otterspoor LC, Kalkman CJ, Cremer OL : Update on the propofol infusion syndrome in ICU management of patients with head injury. Curr Opin Anaesthesiol 2008, 21 : 544-551,   14. Roberts RJ, Barletta JF, Fong JJ, Schumaker G, Kuper PJ, Papadopoulos S, et al : Incidence of propofol-related infusion syndrome in critically ill adults : a prospective, multicenter study. Crit Care 2009, 13 : R169,    15. Rozet I, Tontisirin N, Vavilala MS, Treggiari MM, Lee LA, Lam AM : Prolonged propofol anesthesia is not associated with an increase in blood lactate. Anesth Analg 2009, 109 : 1105-1110,   16. Salengros JC, Velghe-Lenelle CE, Bollens R, Engelman E, Barvais L : Lactic acidosis during propofol-remifentanil anesthesia in an adult. Anesthesiology 2004, 101 : 241-243,   17. T├╝re H, Mercan A, Koner O, Aykac B, T├╝re U : The effects of propofol infusion on hepatic and pancreatic function and acid-base status in children undergoing craniotomy and receiving phenytoin. Anesth Analg 2009, 109 : 366-371,   18. Vasile B, Rasulo F, Candiani A, Latronico N : The pathophysiology of propofol infusion syndrome : a simple name for a complex syndrome. Intensive Care Med 2003, 29 : 1417-1425,   19. Wolf AR, Potter F : Propofol infusion in children : when does an anesthetic tool become an intensive care liability? Paediatr Anaesth 2004, 14 : 435-438,  
Fig.┬Ā1
Flow diagram of the progression through the study. TIVA : total intravenous anesthesia, BIA : balanced inhalation anesthesia. 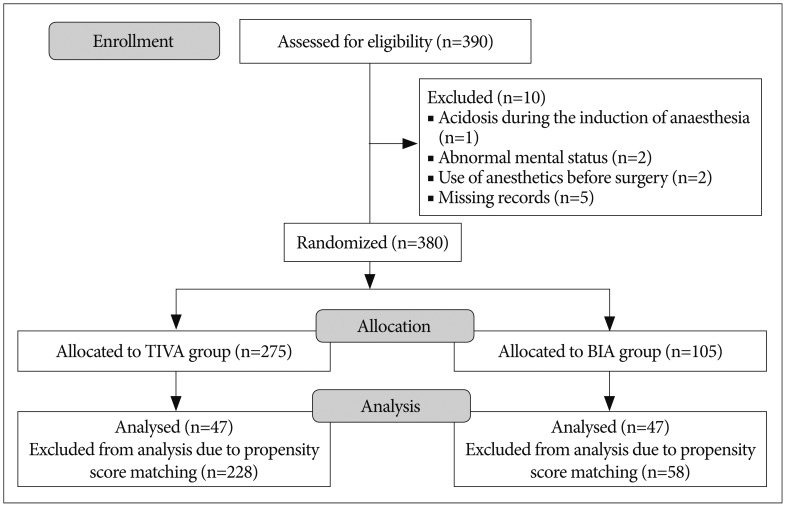
Table┬Ā1
Demographic and clinical characteristics of the TIVA and BIA groups and the incidences of metabolic acidosis 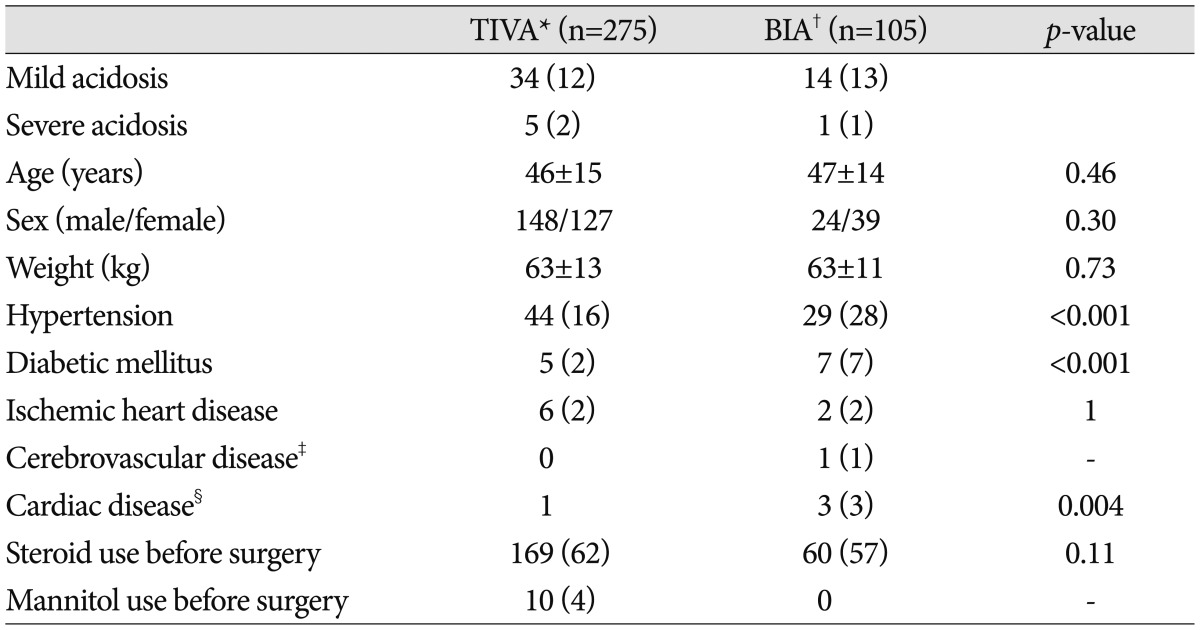
Table┬Ā2
Intraoperative variables and postoperative outcomes of the TIVA and BIA groups 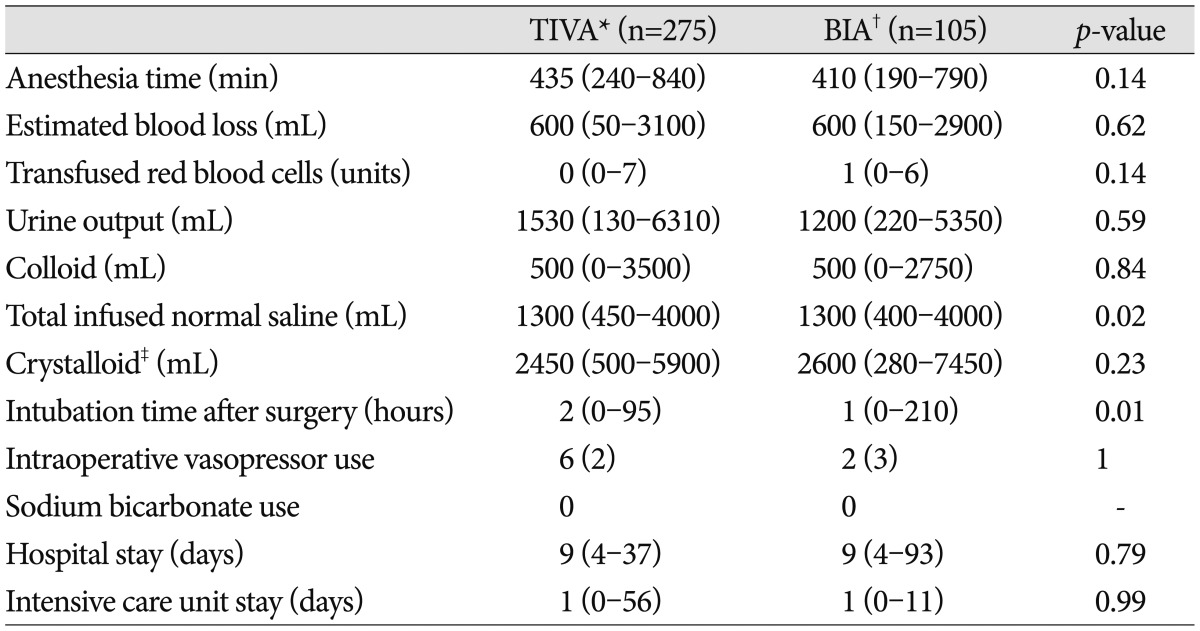
Table┬Ā3
Distribution of demographic risk factors in the propensity-matched cohort 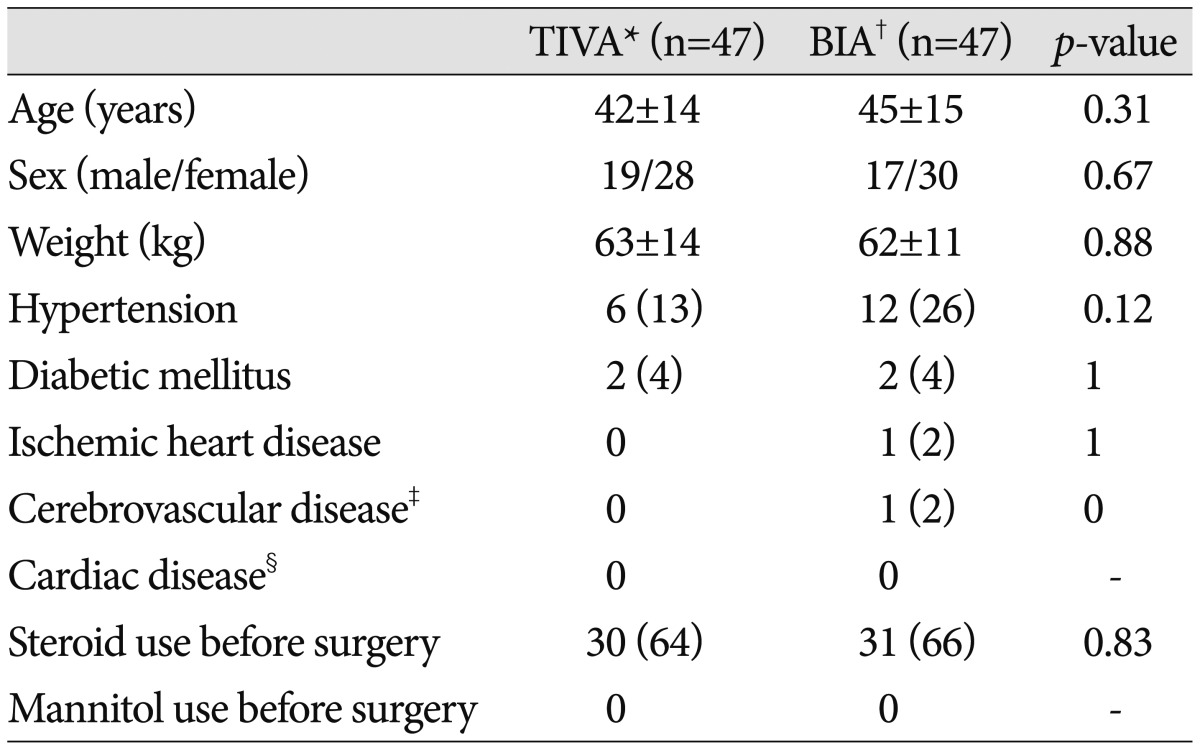
Table┬Ā4
Distribution of perioperative risk factors in the propensity-matched cohort 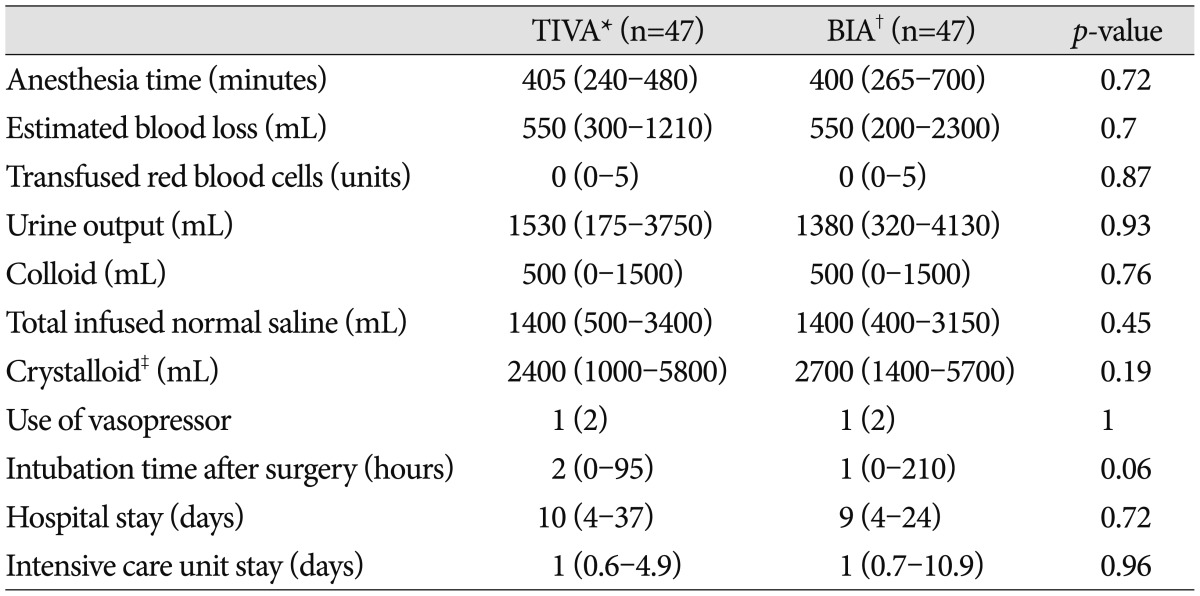
Table┬Ā5
Incidences of metabolic acidosis and base excesses in the propensity-matched cohort 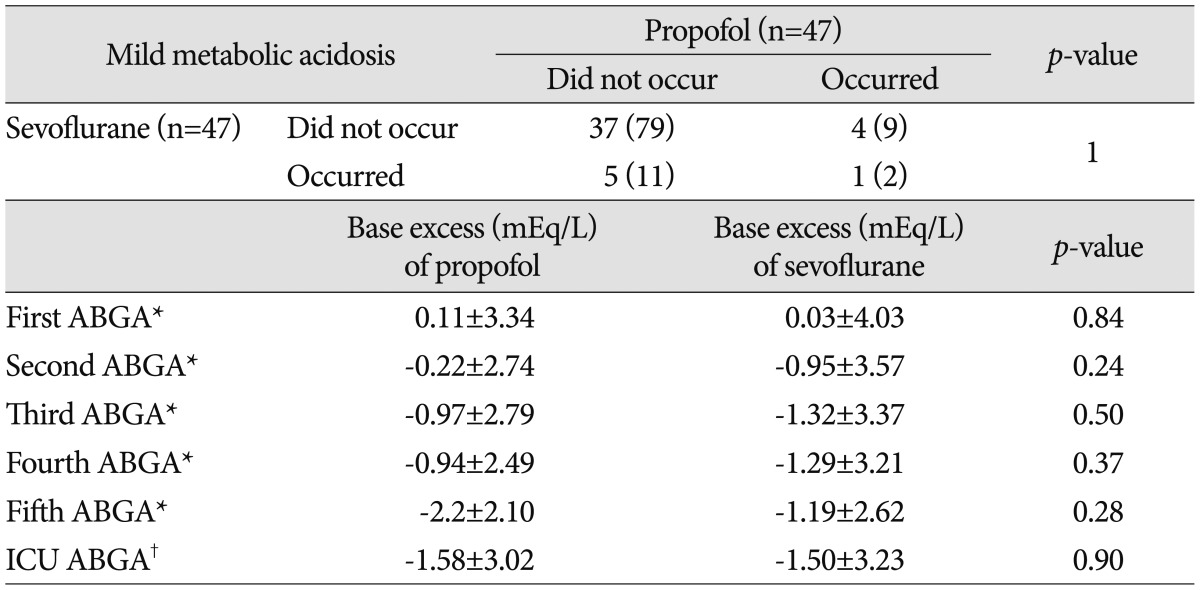
Table┬Ā6
Characteristics of the 5 patients who experienced severe acidosis 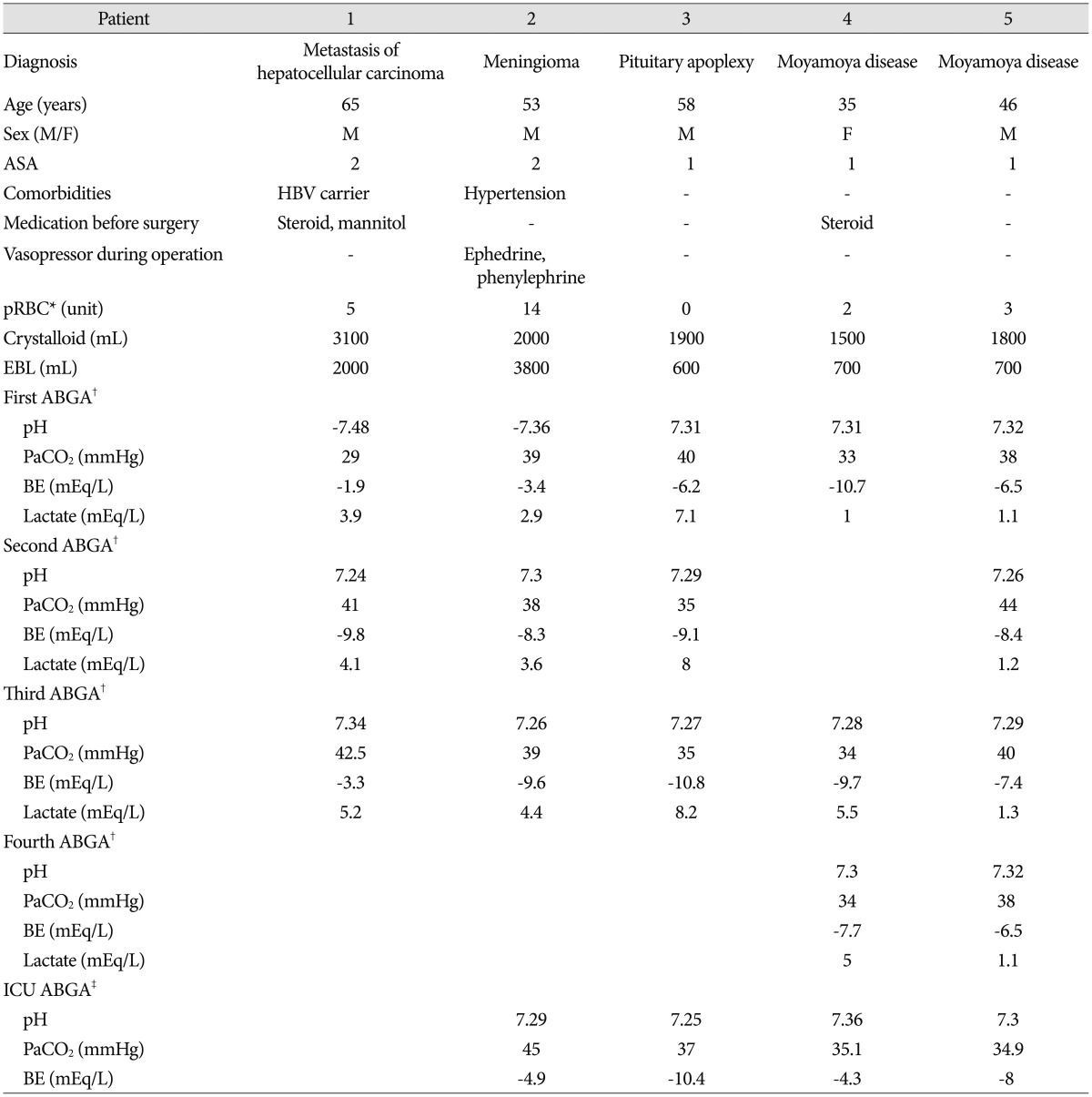
|
|