INTRODUCTION
The occurrence of intracranial meningioma is rare in children; the most prevalent age is the fifth decade4). It accounts for 0.4-4.6% of all primary brain tumors in children and 0.9-3.1% of all intracranial meningiomas3). Bauchet et al.1) studied a series of 1017 primary brain tumors in children and, reported 24 cases (2.4%) of the brain tumor in children below 4 years of age; however, he did not report any case of transitional meningioma. In our department, 416 intracranial meningiomas and 94 childhood primary brain tumors have been treated from 1990 to 2010, but only one tumor has been noted in a child below 2 years of age.
Meningiomas that occur in children have several different characterisitics than those occurring in adults; it shows a higher frequency of secondary degeneration (cystic or sarcomatous), male predominance (M : F=1.16 : 1), absence of dural attachment (dural tail sign), and higher incidence in the intraventricular location6). Here, we report a rare case of a meningioma in a 20-month-old boy.
CASE REPORT
In May 2010, a 20-month-old boy presented with seizure and left hemiparesis; he was admitted to the pediatric department at our hospital. He appeared irritable and had an abnormal pattern of sleep; no other neurological deficits were noted. Laboratory finding were negative for hemato-oncological abnormality. Electroencephalography findings showed complex partial seizure, dialeptic type with left hand palsy.
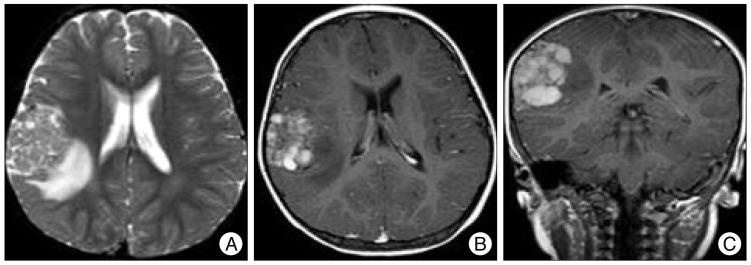
The brain magnetic resonance image (MRI) showed a 4 cm-sized, inhomogeneously enhancing mass with an irregular margin and peritumoral edema in the right frontal lobe (Fig. 1). Based on these radiological findings, the initial diagnosis was an intra-axial tumor, such as pilocytic astrocytoma or dysembryoplastic neuroepithelial tumor. He was transferred to the neurosurgery unit for brain tumor surgery. Because of the peritumoral edema, the steroid (dexamethasone) was administered before the surgery.
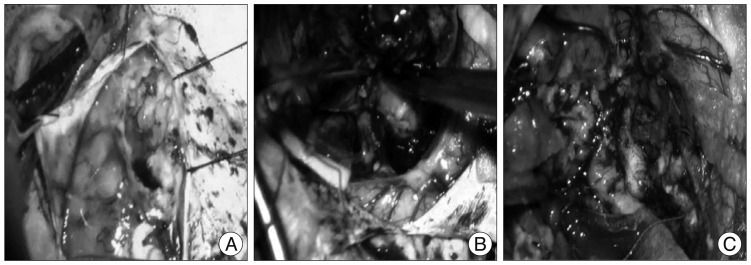
The patient underwent a major surgery with frontal craniotomy. The dura mater was tense. After the dura mater was opened, the tumor was seen to be partially adhered to the surrounding brain tissue but it had no dural attachment. Since the tumor originated from the parenchyme, it was designated as an intra-axial tumor. The intraparenchymal tumor located in right frontoparietal area was removed. After the tumor was removed, intraparenchymal tumor bed was seen (Fig. 2).
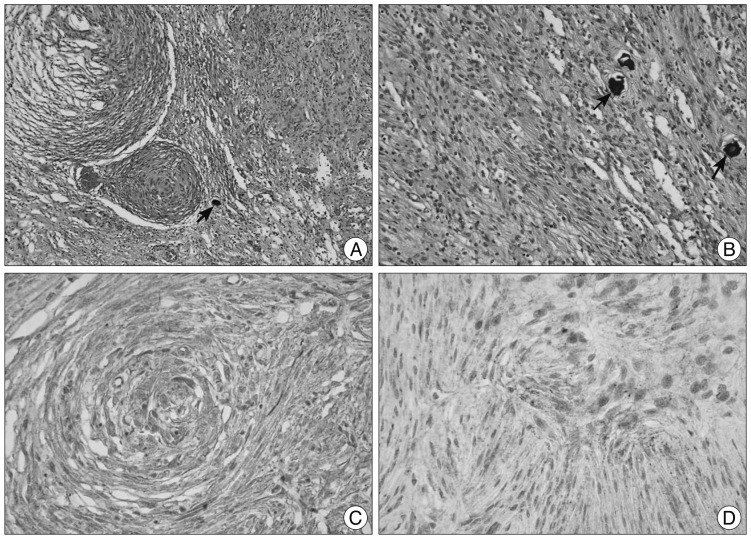
The tumor showed mixed patterns of lobular meningothelial cells, and fibrous spindle cells forming parallel bundles and occasional psammoma bodies.
Immunohistochemical findings showed that the tumor cells were positive for vimentin and focal positive for epithelial membrane antigen.
On the basis of these finding, it was concluded that the tumor was a WHO grade I meningioma, transitional type (Fig. 3).
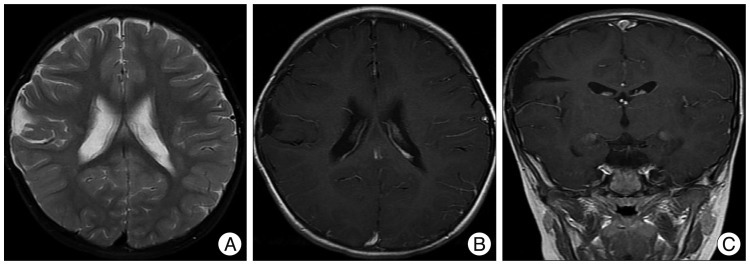
Postoperative follow-up computed tomography scans showed no residual tumor. The patient showed remnant neurological deficit, the left hemiparesis. But, no seizure attack was noted. Anticonvulsant therapy was maintained. During the follow-up 9 months after the surgery, he appeared well and did not experience seizure and recovered the full motor power. The brain MRI showed no recurrence of the tumor, porencephaly in a site where the tumor has been resected (Fig. 4).
DISCUSSION
Meningiomas usually occur in the fifth decade of life4). Infantile meningiomas are extremely rare; less than 30 cases are reported in infants below 1 year of age8,10).
We report a rare case of a meningioma in a 20-month-old boy.
As compared to meningiomas occurring in adults, those occurring in children have several characteristics; they have a higher frequency of secondary degeneration (cystic or sarcomatous), male predominance (M : F=1.16 : 1), absence of dural attachment (dural tail sign) and higher incidence in the intraventricular location6).
Most patients experience headache, vomiting due to increased intracranial pressure and seizure; other common symptoms include nausea, irritability, papilledema, gross motor developmental delay, monoparesis, impaired vision, and diplopia5,8). Our patient presented with seizure and left hemiparesis.
The reported radiological features of childhood meningiomas vary in the literature.
High rate of cyst formation of 15-63.6% which differs from the meningiomas in adults is most commonly mentioned4,6,10). One common neuroradiological finding was the high rate of inhomogeneous enhancement of the tumor (36.2%), which might easily lead to misdiagnosis for glioma or other intra-axial tumors, especially with coexistent cystic components4).
Therefore, diagnosis of meningioma in childhood was challenged because of its rarity and atypical radiologic appearance, unusual location5).
For meningiomas, the primary treatment is surgery9). Complete tumor resection is the most important factor in prevention of tumor reccurence5). Radiation therapy is indicated for patients whose tumors cannot be completely resected, such as tumors that have deep location, large size, and adherence to the vital structure or the tumors that will result in extensive invasion to adjacent structures or severe blood loss during resection4,8). In the present case, the tumor was grossly total resected, and therefore, additional postoperative therapy such as radiotherapy or chemotherapy was not necessary.
Recurrence of a meningioma depends on the extent of removal, its location of tumor, and histological subtype4). The extent of resection seems to be the most important factor influencing the prognosis of a meningioma.
According to different authors, the prognosis of a meningioma in young children is controversial. However, in a recent study conducted by Luigi et al., it was reported that owing to progress in microneurosurgical and anesthesiological techniques, 89% patients showed no recurrence of the tumor on follow-up image study3). Our patient showed no remnant neurological deficit after surgery. Follow-up MRI after 9 months of the surgery showed no recurrence of the tumor.
CONCLUSION
We experienced a rare intracranial meningioma in a 20-month-old boy. The gross total surgical removal was achieved. After the surgery, patient recovered without seizure. Although there are no typical imaging features that are suggestive of meningioma in children, the diagnosis of a meningioma should be considered if a large, solid, cystic enhancing tumor with a relatively Songsharp demarcation is detected in children.